Abstract
Nowadays, endoscopic mucosal resection or endoscopic submucosal dissection has shown effectiveness equivalent to that of gastrectomy and has emerged as a popular technique for curative treatment of gastric cancer. However, noncurative resection or resection beyond the indication may lead to lymphatic and extended organ metastasis resulting in loss of the opportunity for full recovery. Therefore, it is an important issue to decide the range of curative resection in the endoscopic resection field. Furthermore, management of noncurative endoscopic resection in early gastric cancer is also important. The most favorable treatment after noncurative resection would be surgery. However, other noninvasive treatments such as argon plasma coagulation, additional endoscopic resection and close observation for recurrence are thought to be the optional treatments after the noncurative resection. In the future, prospective research studies and observations are expected to verify the effectiveness of noninvasive treatments.
Rising interest in health and regular medical checkups have promoted detection of early cancer. Likewise, in stomach cancer, detection rates for early stages are higher than those for progressive cancer. Consequentially, chances of making a complete recovery are higher nowadays. Traditionally, gastrectomy has generally been regarded as the standard therapy for treatment of gastric cancer. However, endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) has shown effectiveness equivalent to that of gastrectomy and has emerged as a popular technique for curative treatment of gastric cancer. By removing only the lesion, stomach conserving is possible and the quality of life is much improved. However, noncurative resection or resection beyond the indication may lead to lymphatic and extended organ metastasis resulting in loss of the opportunity for full recovery. No prospective studies comparing the results between gastrectomy and endoscopic resection have been reported. Retrospective studies have reported similar results between gastrectomy and endoscopic resection.1 Because the results were similar between patients treated by absolute indications and expanded indications,2,3 many hospitals tend to apply endoscopic removal following expanded indications. Not only treatment indications but also the patients' age, underlying disease, and the clinicians' preference are all carefully considered in the selection of endoscopic removal. On occasion, clinicians contemplate the course of therapy when endoscopic resection is performed outside the indications or curative resection is not achieved despite complete resection. In this section, we discuss further treatment options in the situation of noncurative resection.
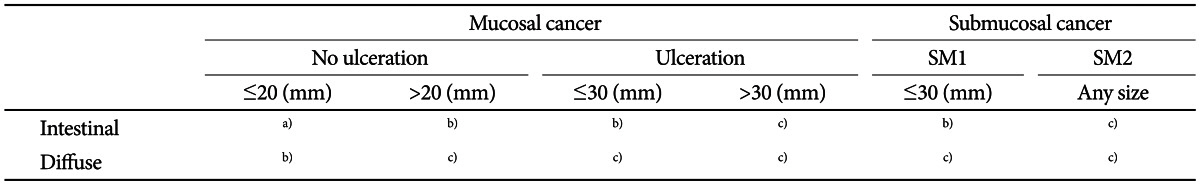
To understand the definition of noncurative resection, one should be aware of the indications of endoscopic resection. Endoscopic resection should be performed only in cases where lymphatic metastasis is unlikely and en bloc resection is possible. According to Korean gastric cancer guidelines, absolute indications for endoscopic resection are: 1) differentiated cancer confined to the mucosa; 2) longer diameter than 2 cm; 3) no evidence of an ulcer or ulcer scar; and 4) no lymphatic invasion of cancer cells.4 The Japanese Gastric Cancer Association recommends EMR/ESD in such cases.5 Expanded indications include: 1) differentiated not ulcerous mucosal cancer, regardless of size; 2) differentiated ulcerous mucosal adenocarcinoma smaller than 3 cm; 3) poorly differentiated not ulcerous mucosal adenocarcinoma smaller than 2 cm; and 4) differentiated adenocarcinoma in which invasion depth is less than 500 µm (SM1). According to the Japanese Gastric Cancer Association guidelines, SM1 differentiated adenocarcinoma is not included in the expansive indications (it is still included in the indication for noncurative resection). If the expanded indication is satisfied, investigational treatment by ESD (not EMR) is suggested. In Korean guidelines, there have been no remarks regarding recommendation of ESD for expanded indications. However, attempts to expand the indications on treatment by ESD have been reported (Table 1).6-8
Although no large scale clinical study has been conducted and no hard evidence has been found, most clinics perform ESD as a standard therapy for complete cure rather than experimental treatment. Because there are difficulties in officially recommending ESD by expanded indication, careful interpretation by expanded indications should be required.
Curative resection is only defined as when the adenocarcinoma is completely resected and lymphatic metastasis is not risky. Absolute indications are: 1) en bloc resection; 2) less than 2 cm; 3) differentiated type; 4) confined to the mucosa; 5) complete resection along the horizontal margin (HM0) and the vertical margin (VM0); and 6) no lymphovascular metastasis (ly (-), v (-)). All of these conditions should be satisfied for the absolute indication. Curative resection after ESD according to the expanded indications are: en bloc resection, HM0, VM0, ly (-), v (-) should be possible; 1) larger than 2 cm, differentiated type confined to the mucosa without an ulcer; 2) smaller than 3 cm, differentiated type confined to the mucosa with an ulcer; 3) smaller than 2 cm, poorly differentiated mucosal cancer without an ulcer; and 4) differentiated cancer smaller than 3 cm and submucosal depth invasion less than 500 µm (SM1). Therefore, noncurative resection is defined as cases that do not satisfy the indications described above.
In practice, histological results after ESD may or may not satisfy the above indications. It is particularly confusing when differentiated cancer and poorly differentiated cancer are mixed.
Despite weak supporting evidence: 1) differentiated mucosal cancer larger than 2 cm without ulcers mixed with poorly differentiated cancer larger than 2 cm; 2) differentiated mucosal cancer with ulcers smaller than 3 cm mixed with poorly differentiated cancer; and 3) poorly differentiated cancer with submucosal invasion are classified as noncurative resection.
As mentioned above, size, differentiation, and ulcers are important factors in classifying the indications and judging curative resection. The pathologist's report is important in defining ulcers; however, endoscopic or radiological judgment is also referred to.5 If complete resection is not possible, it is called 'incomplete resection' or 'impossible to judge' (complete resection according to endoscopy but impossible to judge by pathology).9 Therefore, 'complete resection' is often decided according to the subjective opinion of the physician performing the endoscopy. Since the definition of 'ulcer' differs between scholars, it seems appropriate to judge each case individually and yet comply with the basic principles.
According to National Comprehensive Cancer Network guidelines, history taking and physical examination should be performed every 3 to 6 months for the first 1 to 3 years, every 6 months during 3 to 6 years, and yearly afterwards for long-term observation after complete resection. Clinical chemistry tests, radiologic and endoscopic tests should be performed when needed.10 Korean gastric cancer standard treatment guidelines recommend yearly endoscopic follow-up for the possibility of synchronous or metachronous cancer. The Japanese Gastric Cancer Association recommends Helicobacter pylori eradication and endoscopic follow-up every 6 months or yearly after complete cure by absolute indication. H. pylori eradication, endoscopy, and computed tomography scan or ultrasonography is recommended after treatment by expanded indication.5 As discussed above, close observation and examination after curative resection is the appropriate treatment option. However, these guidelines are not established surveillance guidelines for noncurative resection.
The most favorable treatment after noncurative resection would be surgery. Among the expanded indications, mucosal cancer larger than 3 cm with ulcers, deep submucosal invasion, and lymphatic metastasis are typical indications.11 Recently, there have been many reports on the outcome of additional surgery after endoscopic resection. In a domestic research study analyzing patients who underwent radical gastrectomy after ESD, nine out of 13 patients with positive margin had residual cancer. Fifty percent of patients who underwent surgery for lymphatic invasion of ESD specimen showed positive lymph node metastasis.12 In another study involving 28 patients who underwent additional surgery after endoscopic resection, eight patients (28.6%) had residual cancer and one had lymphatic metastasis. The study found that piecemeal endoscopic resection or diffuse type of cancer, or positive vertical resection margin are risk factors for residual cancer.13 In a research study on indications for surgery after noncurative resection, 43 patients underwent additional surgery; 65.1% of them showed submucosal invasion, 39.5% had residual cancer, and 9.3% had lymphatic invasion. Curiously, margin negative SM1 differentiated cancer corresponding to the expanded indication had no lymphatic metastasis or residual cancer. However, one case of 4 cm sized mucosal cancer showed lymphatic metastasis.14 Fibrosis was found in pathology analyzed after endoscopic resection. This may be the result of biopsy performed before endoscopic resection; however, it may also be the result of ulcerous lesions. Therefore, over interpretation should be carefully considered. A multicenter domestic study regarding additional surgery after endoscopic resection was also reported. The patients were grouped according to five categories: submucosal invasion group, positive resection margin group, unknown resection margin positivity group, high probability of lymphatic invasion group, and local recurrence group. Among 44 resection margin positive patients, 11 had no signs of residual cancer or lymphatic metastasis.15 Among the total 86 patients, 56 (65.1%) had residual cancer and five (5.8%) had lymphatic metastasis. For these patients, surgery is generally required. However, this study contains many suggestions indicating that other treatment strategies rather than surgery were possible for certain groups.
Surgery is a desirable treatment; however, other treatment methods may be recommended based on the patient's general condition, underlying disease, age, and patient's refusal of surgery. In particular, when the possibility of lymphatic metastasis is low (after resection, for example), when differentiated mucosal cancer has positive margin only, when complete resection is achieved although piecemeal resection has been performed, etc., additional endoscopic resection, cauterization using laser or argon plasma coagulation (APC) and simply looking forward to the burn effect are all considered treatment methods while postponing additional treatment and closely observing the patient.16 According to Japanese Gastric Cancer Association guidelines, focally recurred adenocarcinoma after EMR/ESD should be treated with additional ESD. However, since supporting evidence is weak, this is just one experimental treatment modality.
Favorable treatment outcomes of ESD for local recurrence after endoscopic resection have been reported. In a retrospective analysis of 64 patients who had local recurrence of early gastric cancer (EGC) after EMR, patients treated with ESD had higher rates of complete resection and curative resection than patients who underwent repeated EMR. In the case of curative resection, there was no recurrence during follow-up.17 In another Japanese report, 15 patients underwent ESD for local recurrent EGC and curative resection rate was 93.9%. There was no recurrence during follow-up durations.18 In a study of 1,150 patients treated with ESD as primary treatment, eight out of 33 patients with positive margin underwent ESD once more and there were no signs of recurrence during follow-up. Recurrent tumors were observed in four out of 12 patients who had close follow-up without additional treatment.19 Recently, a researcher in Korea reported the results of 1,012 EGC patients; 107 of the patients had a positive HM or a positive VM; 45 patients underwent immediate surgery, and one patient received additional ESD. Lymphatic metastasis or residual cancer was detected in 37% (17 patients). Thirty-nine out of 56 patients who did not undergo additional treatment showed no recurrence during observation. Among 17 patients who had recurred, three received APC, and five underwent additional ESD. In one patient who received APC after recurrence, there was cancer progression. The authors concluded that although the residual cancer volume is larger in positive horizontal resection margin than positive vertical resection margin and the possibility of recurrence is higher (odds ratio, 2.05; 95% confidence interval, 1.22 to 3.44), lymphatic metastasis is rare. Therefore, they emphasized that immediate additional ESD before fibrosis can lower the risk of recurrence.20 In another domestic study of 427 EGC patients, 58 patients had incomplete removal after endoscopic resection. Three patients who underwent additional ESD showed satisfactory results. However, both patients treated with APC showed recurrence.21 As in the previously mentioned research studies, this study supports that APC appears to be less effective. However, in other studies using APC as initial treatment, only 10% showed recurrence and many showed favorable results. This is more likely when treated by a well trained and experienced endoscopy expert.22 Therefore, in high risk patients for endoscopic resection or surgery, rescue treatment with APC is thought to be the optional treatment.
If conservative or microinvasive treatment is impossible, close observation may also be acceptable. However, no research studies on observation alone have been reported. Some reports have noted that margin positive cancer shows no recurrence with surgery or observation.15,19,20 Therefore, close observation for recurrence may be another alternative for treatment.
Endoscopic resection by EMR/ESD is an important treatment method for EGC. Because of the increasing incidence of EGC, endoscopic resection rates have increased and there are many ongoing research studies regarding the expanded indications. The main target is curative radical resection. Therefore, it is an important issue to decide on the range of curative resection in the endoscopic resection field. Additional noninvasive strategies such as endoscopic resection, surgery, and APC are performed when curative resection is not achieved after resection. Salvage therapy for complete cure in surgery or conservative endoscopic therapy is effective in some patients. In the future, prospective research studies and observations are expected to verify the effectiveness of noninvasive treatments.
References
1. Choi KS, Jung HY, Choi KD, et al. EMR versus gastrectomy for intramucosal gastric cancer: comparison of long-term outcomes. Gastrointest Endosc. 2011; 73:942–948. PMID: 21392757.

2. Gotoda T, Iwasaki M, Kusano C, Seewald S, Oda I. Endoscopic resection of early gastric cancer treated by guideline and expanded National Cancer Centre criteria. Br J Surg. 2010; 97:868–871. PMID: 20301163.

3. Lee H, Yun WK, Min BH, et al. A feasibility study on the expanded indication for endoscopic submucosal dissection of early gastric cancer. Surg Endosc. 2011; 25:1985–1993. PMID: 21136092.

4. Korean Academy of Medical Science. Korean Clinical Practice Guide-lines for Gastric Cancer. Seoul: Korean Academy of Medical Science;2012.
5. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123. PMID: 21573742.
6. Ahn JY, Jung HY, Choi KD, et al. Endoscopic and oncologic outcomes after endoscopic resection for early gastric cancer: 1370 cases of absolute and extended indications. Gastrointest Endosc. 2011; 74:485–493. PMID: 21741645.

7. Oda I, Saito D, Tada M, et al. A multicenter retrospective study of endoscopic resection for early gastric cancer. Gastric Cancer. 2006; 9:262–270. PMID: 17235627.

8. Goh PG, Jeong HY, Kim MJ, et al. Clinical outcomes of endoscopic submucosal dissection for undifferentiated or submucosal invasive early gastric cancer. Clin Endosc. 2011; 44:116–122. PMID: 22741122.

9. Ono H. Early gastric cancer: diagnosis, pathology, treatment techniques and treatment outcomes. Eur J Gastroenterol Hepatol. 2006; 18:863–866. PMID: 16825902.

10. Ajani JA, Barthel JS, Bekaii-Saab T, et al. Gastric cancer. J Natl Compr Canc Netw. 2010; 8:378–409. PMID: 20410333.
11. Rembacken BJ, Gotoda T, Fujii T, Axon AT. Endoscopic mucosal resection. Endoscopy. 2001; 33:709–718. PMID: 11490390.

12. Noh H, Park JJ, Yun JW, et al. Clinicopathologic characteristics of patients who underwent curative additional gastrectomy after endoscopic submucosal dissection for early gastric cancer or adenoma. Korean J Gastroenterol. 2012; 59:289–295. PMID: 22544026.

13. Lee JH, Kim JH, Kim DH, et al. Is surgical treatment necessary after non-curative endoscopic resection for early gastric cancer? J Gastric Cancer. 2010; 10:182–187. PMID: 22076184.

14. Ryu KW, Choi IJ, Doh YW, et al. Surgical indication for non-curative endoscopic resection in early gastric cancer. Ann Surg Oncol. 2007; 14:3428–3434. PMID: 17899290.

15. Song KY, Hyung WJ, Kim HH, et al. Is gastrectomy mandatory for all residual or recurrent gastric cancer following endoscopic resection? A large-scale Korean multi-center study. J Surg Oncol. 2008; 98:6–10. PMID: 18521830.

16. Alfaro EE, Lauwers GY. Early gastric neoplasia: diagnosis and implications. Adv Anat Pathol. 2011; 18:268–280. PMID: 21654358.
17. Yokoi C, Gotoda T, Hamanaka H, Oda I. Endoscopic submucosal dissection allows curative resection of locally recurrent early gastric cancer after prior endoscopic mucosal resection. Gastrointest Endosc. 2006; 64:212–218. PMID: 16860071.

18. Oka S, Tanaka S, Kaneko I, et al. Endoscopic submucosal dissection for residual/local recurrence of early gastric cancer after endoscopic mucosal resection. Endoscopy. 2006; 38:996–1000. PMID: 17058164.

19. Kikuchi D, Iizuka T, Hoteya S, et al. Safety and efficacy of secondary endoscopic submucosal dissection for residual gastric carcinoma after primary endoscopic submucosal dissection. Digestion. 2012; 86:288–293. PMID: 23051712.

20. Yoon H, Kim SG, Choi J, et al. Risk factors of residual or recurrent tumor in patients with a tumor-positive resection margin after endoscopic resection of early gastric cancer. Surg Endosc. 2013; 27:1561–1568. PMID: 23263643.

21. Park JC, Lee SK, Seo JH, et al. Predictive factors for local recurrence after endoscopic resection for early gastric cancer: long-term clinical outcome in a single-center experience. Surg Endosc. 2010; 24:2842–2849. PMID: 20428894.

22. Tomita T, Arai E, Kohno T, et al. Outcomes of treatment of argon plasma coagulation therapy in elderly or high-risk patients with early gastric cancer: a comparison of outcomes among experienced and nonexperienced endoscopists. J Clin Gastroenterol. 2011; 45:e54–e59. PMID: 20838235.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download