Abstract
Regardless of outstanding developments in the endoscopic field, laryngopharyngeal lesions are generally considered as a field of otolaryngology, and thus it is thought that not a lot of gastrointestinal endoscopists commonly take interest in these lesions during the upper gastrointestinal endoscopic examinations. Therefore, here in this thesis, I reviewed the availability of upper gastrointestinal endoscopy in laryngopharyngeal area, normal structures of laryngopharynx, and the lesions that can be observed with the standard upper gastrointestinal endoscopic procedure.
With the rapid increase in the number of upper and lower gastrointestinal endoscopic procedures as a part of the national cancer screening project, early detection of various gastrointestinal precancerous or cancerous lesions have been increased, recently. These early detection of the lesions in early stage has been greatly helpful for the enhancement of the quality of life or life prolongation and have also allowed the significant reduction of medical costs through the endoscopic surgery without cutting the abdomen or chest.1-3 Regardless of such rapid development in the endoscopic field, laryngopharyngeal lesions are generally considered as a field of otolaryngology, and thus it is thought that not a lot of gastrointestinal endoscopists commonly take interest in these lesions during the upper gastrointestinal endoscopic examinations. Therefore, most laryngopharyngeal lesions are difficult to be detected by gastrointestinal endoscopists. The laryngopharynx is a structure that must be passed inevitably during upper gastrointestinal endoscopic insertion; hence various diseases can be detected if the area is examined in detail during endoscopy. According to the reports which have studied laryngopharyngeal lesions that can be observed during upper gastrointestinal endoscopic procedures, 0.9% to 3.5% of all tests have displayed abnormalities in the laryngopharynx.4-10 Furthermore, the field of endoscopic treatment is expanding to include laryngopharynx lesions.11 Accordingly, this thesis will review the availability of upper gastrointestinal endoscopy in laryngopharyngeal area, normal structures of laryngopharynx, and the lesions that can be observed with the standard upper gastrointestinal endoscopic procedure.
The pharynx is divided into three parts: nasopharynx, oropharynx, and hypopharynx. From the soft palate, the top part is the nasopharynx, and from the soft palate to the epiglottis is the oropharynx, and from the bottom of the epiglottis to the entrance of the esophagus is the hypopharynx. The hypopharynx applies to the back of the larynx.12 The larynx is the vocal organ that includes the vocal cords, and the oropharynx is located on the top, with the trachea located on the bottom and the hypopharynx on the back. The oropharynx and larynx can be observed in a standard upper gastrointestinal endoscopy, and the nasopharynx can be observed with the recently developed endoscopy, although its use is not popular.
There are differences based on the type of mouth-piece used during endoscopic procedures, but when the endoscope is inserted using the most commonly used tongue depressor type mouth-piece, observations can be conducted from the soft palate. After the uvula and both tonsils connected to the soft palate are observed, and when the tube is progressed further, the epiglottis and lymph nodes near the root of the tongue are seen, followed by most of the larynx and parts of the hypopharynx can be seen. Here, the vocal cords, insides of the epiglottis, the corniculate cartilage, arytenoids cartilage, and pyriform sinus can be observed (Fig. 1). However, when air is released while these parts are observed, severe coughing can occur due to the inflow of secretion through the airway, thus air must be inflowed as less as possible, and the parts must be observed within a short period of time. If necessary, the area should be reobserved when removing the endoscope after observing the esophagus, stomach, and duodenum.
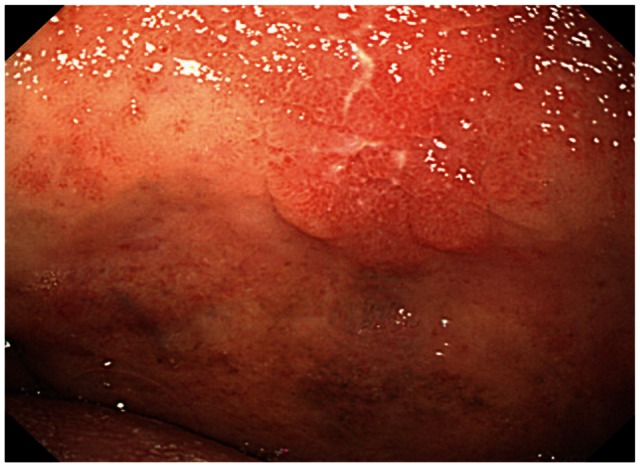
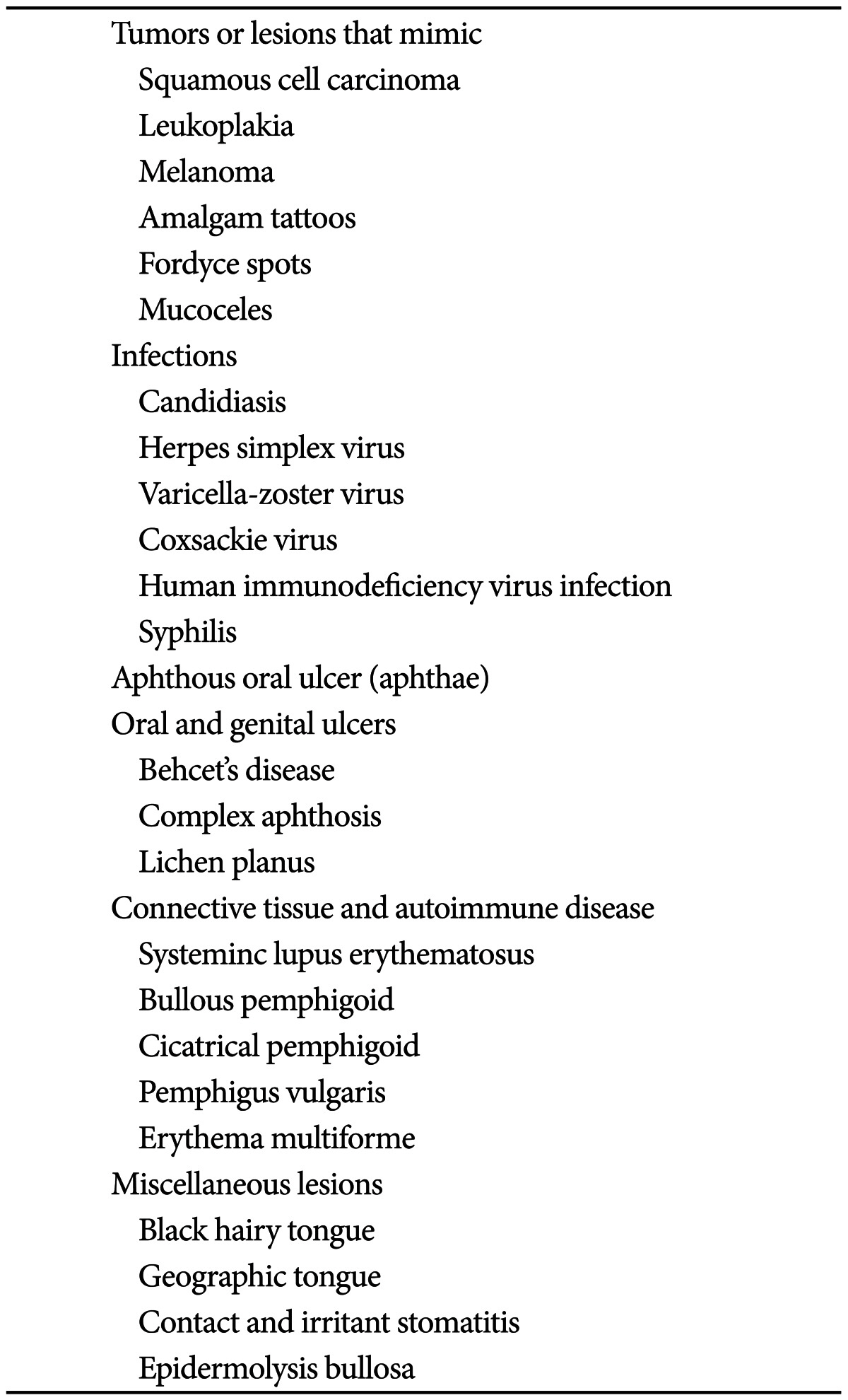
A part of the mouth can sometimes be observed-there are not many parts that can be observed thoroughly due to the mouthpiece used during the endoscopic procedure; however, soft palate lesions can sometimes be observed quite easily, with greater care. The diseases that can occur within the oral cavity, such as the lips, gums, teeth, hard palate, and soft palate have been shown on Table 1. It includes various diseases based on various causes; oral ulcers, connective tissue diseases, various infectious diseases, and benign or malignant tumors (Fig. 2). Even if lesions do exist, it is difficult to discover them during the actual endoscopic procedure because the parts covered by the mouth-piece are commonly affected. However, when suspicious lesions are discovered, biopsy should be taken or consulted to the laryngologist, if available.
The gastroesophageal reflux disease does not only display esophageal symptoms but also includes various extraesophageal symptoms or complications, including coughing, laryngitis, asthma, dental caries, pharyngitis, sinusitis, pulmonary fibrosis, otitis media, etc.13 LPR refers to the effect of gastric contents, such as gastric acid or pepsin passing through the upper esophageal sphincter to the laryngopharynx, and may display symptoms such as abnormal vocalization, hoarse voice, globus, dysphagia, and chronic coughing.14,15
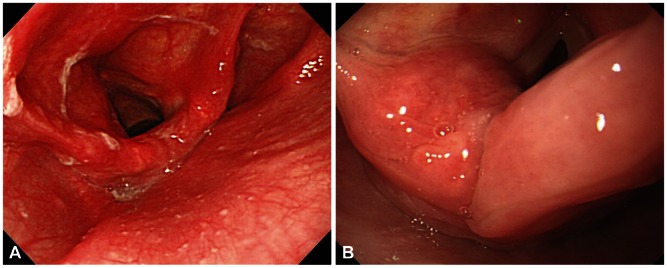
Meanwhile, laryngitis occurs due to various causes, but most of them display similar appearances by the naked eye with no relation to the causes; LPR can also become an important cause, and laryngitis caused by LPR is referred to as reflux laryngitis. There may be controversy on standard diagnostic methods that can easily be conducted concerning the diagnosis of LPR. If abnormal findings are found with the aforementioned symptoms during the endoscopy or laryngoscopy, the diagnosis of LPR can be considered with priority. These abnormal finding may include various appearances, such as erythema, edema, granuloma, and stenosis. Erythema and edema which occur in the mucous membrane between the arytenoid and back of the arytenoid are the most common findings of reflux laryngitis, considering the positional relationship with the upper esophageal sphincter (Fig. 3).16 However, there is diagnostic limitation in that these abnormalities can occur in as high as 70% of general people who do not display specific symptoms, and in that standards of dividing normality and abnormality are not clear.17-19
There have been many studies conducted under the presumption that the 24-hour pH monitoring is the most superior of all diagnostic tools for LPR.20 However, there is no clearcut standard, and there are also reports which show large amount of false positive results, displaying a positive rate of 10% to 60% in healthy people with no symptoms. Thus, this test is not recommended to all patients.21
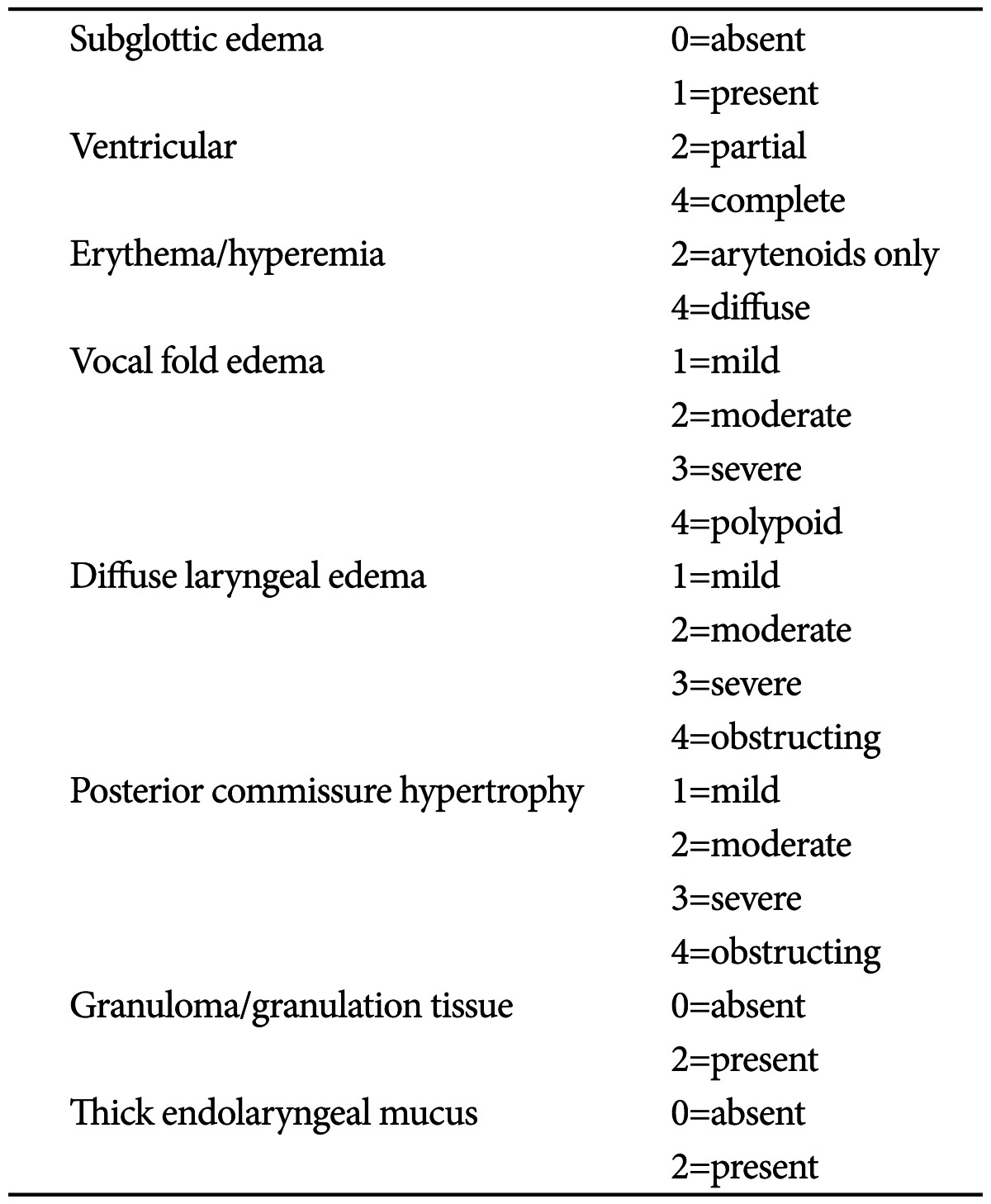
Recently, reflux finding score, which consists of eight categories observed through the laryngoscope, has been proposed in the otolaryngologic field to standardize the diagnosis of LPR (Table 2).22 This system displayed a highly significant consistency within and between the observers, as well as reproducibility, and was reported to help the judgment of improvement after the treatment of reflux laryngitis. Furthermore, this scoring system and a survey that grades reflux symptoms have been used in reports that have successfully researched the reaction to treatments, thus is considered as being an element worth considering for use in the gastroenterologic field.23-25
Other than in special cases, such as having no consciousness or being unable to communicate, caustic damage can generally be predicted through medical history taking. Various findings can be shown based on the causing material. Erythema, edema, and bleeding can be seen during the acute phase, and as time progresses, edema, and erythema can decrease, with change in the surrounding tissues due to fibrosis. During the chronic phase, stenosis due to deformity becomes the greatest problem.26
White membranous substances similar to esophageal candidiasis can be seen in the oral membrane or the laryngopharynx, and can commonly occur in situations with suppressed immunity, such as with chronic diseases or use of steroids. Membranous substances can be diagnosed by dying potassium hydroxide.27
There is a need to suspect laryngeal cancer in patients with changes in their voice. The larynx is located directly above the vocal cord, so laryngeal cancer is relatively easy to detect. However, if the cancer is located in the dented area between the epiglottis and vocal cord, it may be difficult to diagnose. It is observed in various shapes, and can easily bleed on contact with the endoscope, and displays a tendency of easy friability during biopsies.28 Caution must be taken during biopsies so that pulmonary aspiration due to bleeding does not occur.
During endoscopic procedure, the scope enters through the left pyriform sinus, thus hypopharyngeal cancer located on the back of the left arytenoid is occasionally found. If the mass is large, it can easily be found, but without care, it can easily be missed even after several procedures. The shape is very diverse and is almost undistinguishable with the naked eye, but it displays easy bleeding on contact with the scope, and thus can be diagnosed by biopsies. The surface of oral cavity, larynx, and hypopharynx is composed of squamous epithelium, just as the esophagus. Thus, laryngeal or hypopharyngeal cancer can occur synchronously or metachronously with esophageal cancer.29 Therefore, the hypopharynx or larynx must thoroughly be examined in esophageal cancer patients,30 and inversely, it is necessary to thoroughly examine the esophagus in hypopharynx or laryngeal cancer patients. Recently, new video imaging methods such as narrow band imaging are contributing to the early detection of these diseases.31
Papillomas, cysts, vocal fold polyps, lipomas, hymangiomas, and other various benign tumors can be discovered in the larynx, hypopharynx, epiglottis, and oral cavity.32 Sometimes local leukoplakia is found in various parts. This is a precancerous lesion and it is recommended to be removed, if possible.
As side effects of tracheal intubation in patients treated with mechanical ventilation or general anesthesia, tracheostenosis, organ-esophageal fistula, and granulomas may occur due to the fibrosis of the stimulated area.33 It is known that the intubation period or early laryngeal damage cannot predict the occurrence of granulomas. If a hoarse voice continues 7 to 10 days after extubation, the formation of a granuloma should be suspected and a diagnostic evaluation is recommended. Many cases require surgical removal.
Laryngopharyngeal edemas may occur after forceful inserting of the scope or during tracheal intubation, thus caution is needed. It also may occur after repetitive procedures due to hematemesis, or after difficult procedure due to severe vomiting.
Various deformities may be observed after the operation of laryngeal or hypopharyngeal cancer. In those cases, there is a need to confirm the surgical history of the patient through detailed medical history taking before the procedure. If one side of the pyriform sinus is closed after surgery, the scope must be entered through the pyriform sinus located on the opposite side. And thorough observation for synchronous or metachronous lesions is needed.
Unlike simple aphthous ulcers, oral ulcers based on Behcet's disease are not easily healed, and frequently relapse. If ulcers also occur in other areas, such as the genital area, this disease may be suspected. Most ulcers occur in the mouth, but also can occur in the pharynx or hypopharynx. Deformity of the surrounding areas can also be developed due to deep ulcers.
Local discoloration may occur on the mucous membrane due to angiodysplasia or infections, and it can also be observed before or after the formation of ulcers.
Vocal cord paralysis can occur due to a large variety of causes, such as gastric acid reflux, exercise, stress, postoperation, neurological disorders, etc. It is commonly accompanied by the change in voice. Although, recently, endoscopic procedures under conscious sedation may restrict observation of the vocal cords, vocal cord paralysis can also be confirmed by allowing the patient to use the vocal cord during the diagnosis.34
As mentioned, oral and laryngopharyngeal lesions which can easily be observed with careful upper gastrointestinal endoscopic procedure were reviewed. On the other hands, these lesions may easily be missed if careful examination is not performed. Considering the current medical circumstances in Korea where a large number of patients must be examined within a short period of time, it is not easy to diagnose the lesions which exist in these oropharyngolaryngeal areas. However, with thorough examinations conducted with great care within the possible area, various diseases can be detected in early stage and it can be a great help to the patients. These careful examinations are also expected to increase the effectiveness of the endoscopic procedures.
References
1. Chang DK. Current status of colorectal endoscopic submucosal dissection in Korea. Clin Endosc. 2012; 45:288–289. PMID: 22977820.

2. Goh PG, Jeong HY, Kim MJ, et al. Clinical outcomes of endoscopic submucosal dissection for undifferentiated or submucosal invasive early gastric cancer. Clin Endosc. 2011; 44:116–122. PMID: 22741122.

3. Kim YS, Cho WY, Cho JY, Jin SY. Successful treatment of early gastric cancer adjacent to a fundal varix by endoscopic submucosal dissection and endoscopic cyanoacrylate therapy. Clin Endosc. 2012; 45:169–173. PMID: 22866260.

4. Katsinelos P, Kountouras J, Chatzimavroudis G, et al. Should inspection of the laryngopharyngeal area be part of routine upper gastrointestinal endoscopy? A prospective study. Dig Liver Dis. 2009; 41:283–288. PMID: 18701359.

5. Cammarota G, Galli J, Agostino S, et al. Accuracy of laryngeal examination during upper gastrointestinal endoscopy for premalignancy screening: prospective study in patients with and without reflux symptoms. Endoscopy. 2006; 38:376–381. PMID: 16680637.

6. Raju GS. Value of screening the laryngopharyngeal area during routine upper gastrointestinal endoscopy. Nat Clin Pract Gastroenterol Hepatol. 2005; 2:22–23. PMID: 16265096.

7. Mullhaupt B, Jenny D, Albert S, Schmid S, Fried M. Controlled prospective evaluation of the diagnostic yield of a laryngopharyngeal screening examination during upper gastrointestinal endoscopy. Gut. 2004; 53:1232–1234. PMID: 15306576.

8. Yarze JC, Chase MP, Herlihy KJ. Laryngopharyngeal examination: an important but not-so-new role of upper gastrointestinal endoscopy. Ann Intern Med. 2000; 133:314–315. PMID: 10929187.

9. Kozarek RA. Evaluation of the larynx, hypopharynx, and nasopharynx at the time of diagnostic upper gastrointestinal endoscopy. Gastrointest Endosc. 1985; 31:271–273. PMID: 4029577.

10. Lehman G, Compton M, Meadows J, Elmore M. Screening examination of the larynx and pharynx during upper gastrointestinal panendoscopy. Gastrointest Endosc. 1982; 28:176–178. PMID: 7129039.

11. Choi JH, Park JJ, Jee JB, et al. Endoscopic treatment of benign hypopharyngeal tumors. Korean J Gastrointest Endosc. 2005; 31:306–310.
12. Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008; 19:691–707. PMID: 18940636.

13. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006; 101:1900–1920. PMID: 16928254.

14. Ford CN. Evaluation and management of laryngopharyngeal reflux. JAMA. 2005; 294:1534–1540. PMID: 16189367.

15. Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991; 101(4 Pt 2):Suppl 53. 1–78. PMID: 1895864.
16. Hickson C, Simpson CB, Falcon R. Laryngeal pseudosulcus as a predictor of laryngopharyngeal reflux. Laryngoscope. 2001; 111:1742–1745. PMID: 11801937.

17. Qadeer MA, Swoger J, Milstein C, et al. Correlation between symptoms and laryngeal signs in laryngopharyngeal reflux. Laryngoscope. 2005; 115:1947–1952. PMID: 16319603.

18. Hicks DM, Ours TM, Abelson TI, Vaezi MF, Richter JE. The prevalence of hypopharynx findings associated with gastroesophageal reflux in normal volunteers. J Voice. 2002; 16:564–579. PMID: 12512644.

19. Branski RC, Bhattacharyya N, Shapiro J. The reliability of the assessment of endoscopic laryngeal findings associated with laryngopharyngeal reflux disease. Laryngoscope. 2002; 112:1019–1024. PMID: 12160267.

20. Merati AL, Lim HJ, Ulualp SO, Toohill RJ. Meta-analysis of upper probe measurements in normal subjects and patients with laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2005; 114:177–182. PMID: 15825565.

21. Noordzij JP, Khidr A, Desper E, Meek RB, Reibel JF, Levine PA. Correlation of pH probe-measured laryngopharyngeal reflux with symptoms and signs of reflux laryngitis. Laryngoscope. 2002; 112:2192–2195. PMID: 12461340.

22. Belafsky PC, Postma GN, Koufman JA. The validity and reliability of the reflux finding score (RFS). Laryngoscope. 2001; 111:1313–1317. PMID: 11568561.

23. Lien HC, Wang CC, Hsu JY, et al. Classical reflux symptoms, hiatus hernia and overweight independently predict pharyngeal acid exposure in patients with suspected reflux laryngitis. Aliment Pharmacol Ther. 2011; 33:89–98. PMID: 21083591.

24. Reichel O, Dressel H, Wiederänders K, Issing WJ. Double-blind, placebo-controlled trial with esomeprazole for symptoms and signs associated with laryngopharyngeal reflux. Otolaryngol Head Neck Surg. 2008; 139:414–420. PMID: 18722223.

25. Belafsky PC, Postma GN, Koufman JA. Laryngopharyngeal reflux symptoms improve before changes in physical findings. Laryngoscope. 2001; 111:979–981. PMID: 11404607.

26. Scott JC, Jones B, Eisele DW, Ravich WJ. Caustic ingestion injuries of the upper aerodigestive tract. Laryngoscope. 1992; 102:1–8. PMID: 1731151.

27. Giannini PJ, Shetty KV. Diagnosis and management of oral candidiasis. Otolaryngol Clin North Am. 2011; 44:231–240. PMID: 21093632.

28. Chu EA, Kim YJ. Laryngeal cancer: diagnosis and preoperative work-up. Otolaryngol Clin North Am. 2008; 41:673–695. PMID: 18570953.

29. Kim JH, Park JE, Nam JH, et al. A case of synchronous esophageal basaloid squamous carcinoma and cancer of the base of tongue. Korean J Gastrointest Endosc. 2005; 31:383–386.
30. Chung KW, Sun HS, Park DH, et al. A case of esophageal cancer with metastasis to the pharynx. Korean J Gastrointest Endosc. 1996; 16:63–67.
31. Yoshimura N, Goda K, Tajiri H, et al. Diagnostic utility of narrow-band imaging endoscopy for pharyngeal superficial carcinoma. World J Gastroenterol. 2011; 17:4999–5006. PMID: 22174550.

32. Tanaka S, Morita Y, Fujita T, et al. Clinicopathological characteristics of abnormal micro-lesions at the oro-hypopharynx detected by a magnifying narrow band imaging system. Dig Endosc. 2012; 24:100–109. PMID: 22348834.

33. Sue RD, Susanto I. Long-term complications of artificial airways. Clin Chest Med. 2003; 24:457–471. PMID: 14535220.

34. Jung SW. Two cases of vocal cord paralysis complicated by upper gastrointestinal endoscopy. Korean J Gastrointest Endosc. 2006; 33:32–36.
Fig. 1
Normal laryngopharyngeal structure under upper gastrointestinal endoscopic procedure. The vocal cords, insides of the epiglottis, the corniculate cartilage, arytenoids cartilage, and pyriform sinus can be observed.
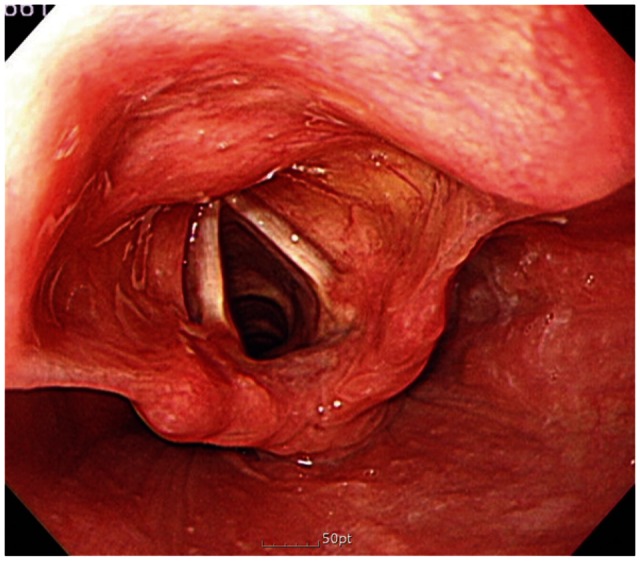
Fig. 2
Soft palate cancer. In a 75-year-old asymptomatic male patient, ill demarcated friable lesion is found on the soft palate.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download