A 75-year-old woman was admitted to the emergency room complaining of hematemesis and hematochezia. She also had epigastric pain, nausea, and vomiting but no fever, weight loss, or rash. Her blood pressure was 110/70 mm Hg, heart rate 72 beats per minute, and respiratory rate 18 breaths per minute. She ingested
Rhus extract 2 days prior. Laboratory examination results were as follows: leukocytes, 20,900/mm
3 (neutrophils, 82%; lymphocytes, 8.9%; eosinophils, 0.1%; monocytes, 8.9%; basophils, 0.1%); hemoglobin, 14.4 g/dL; platelets, 86,000/mm
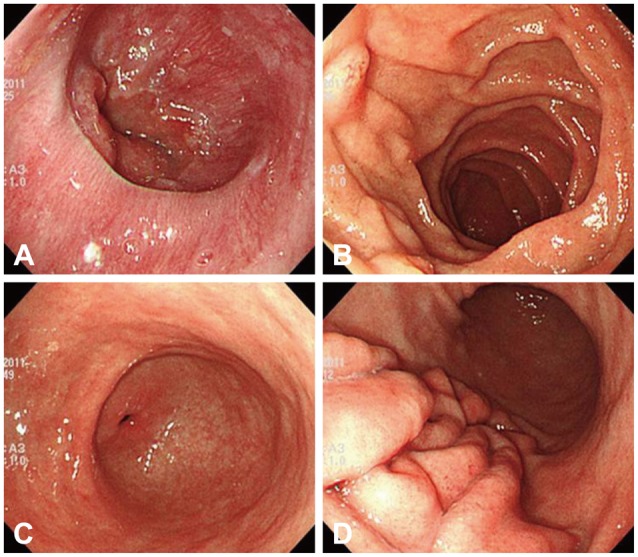
3; and immunoglobulin E, 81.90 IU/mL (normal range, 0 to 100). The albumin level was low (2.9 g/dL; normal range, 3.5 to 5.5 g/dL) but other liver and renal function indicators were within the normal range. Acute phase reactants were elevated (C-reactive protein, 13.8 mg/dL; erythrocyte sedimentation rate, 22 mm/hr). Parasitologic examination and bacterial culture of stool results were normal. Abdominal computed tomography revealed edematous wall thickening of the duodenum and proximal jejunal loops (
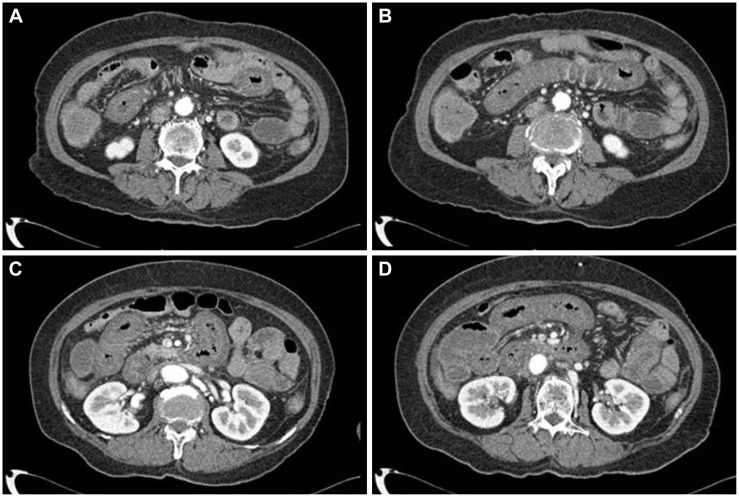
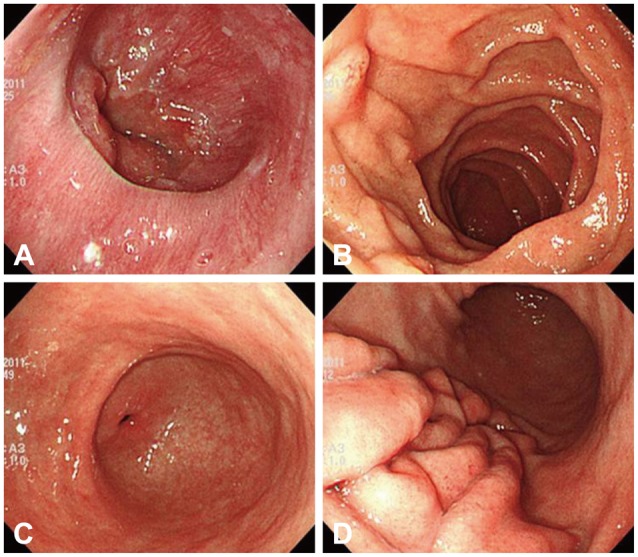
Fig. 1). Endoscopy showed friable and granular mucosal changes with touch bleeding in the second portion of the duodenum (
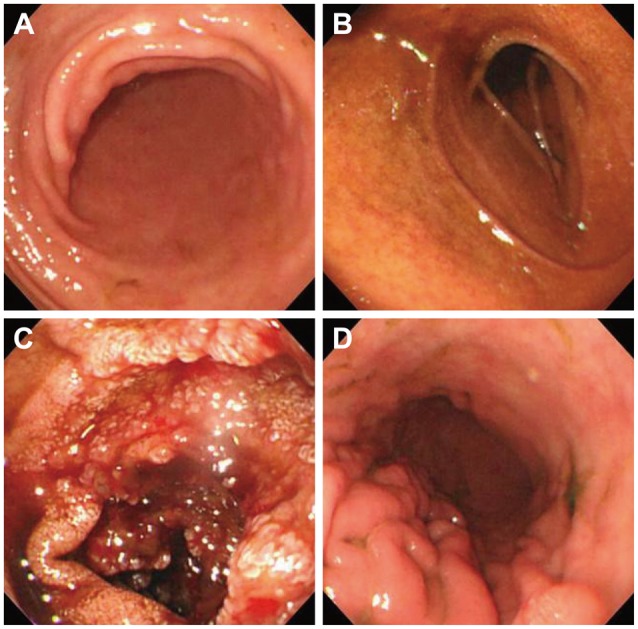
Fig. 2). During the endoscopic examina-tion, multiple duodenal biopsies were taken. Pathologic find-ings showed edematous gastric mucosa and diffusely infiltrated inflammatory cells containing over 100 eosinophils per high power field, consistent with EGE (
Fig. 3). For the evaluation of allergy, we performed a patch test with
Rhus extracts ingested by the patient. We applied the
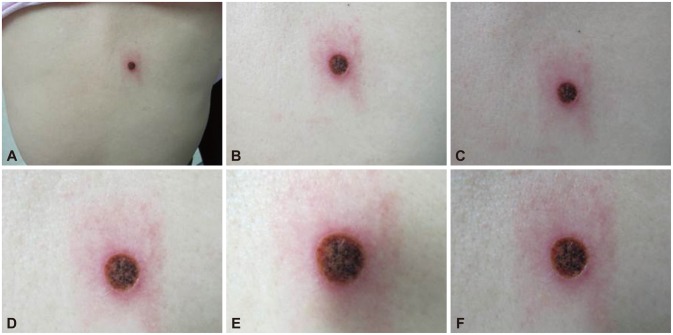
Rhus extract-containing patch to the patient's back for 48 hours and then removed it. Seventy-two hours after patch application, the skin showed erythematous infiltration with ulceration, indicating a strong positive reaction (
Fig. 4). We concluded that the
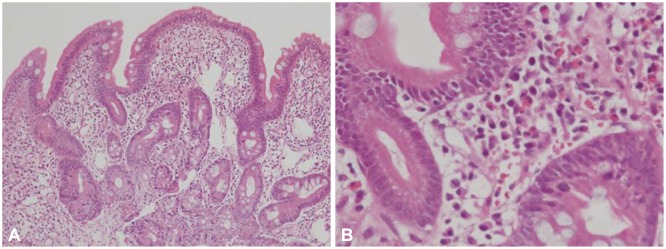
Rhus extract provoked a type IV hypersensitivity reaction on the skin, and that it may be the allergen causing EGE. After avoidance of the allergen, the patient's symptoms remitted. One-month follow-up endoscopy showed improving mucosal edema and nodularity in the duodenum (
Fig. 5).
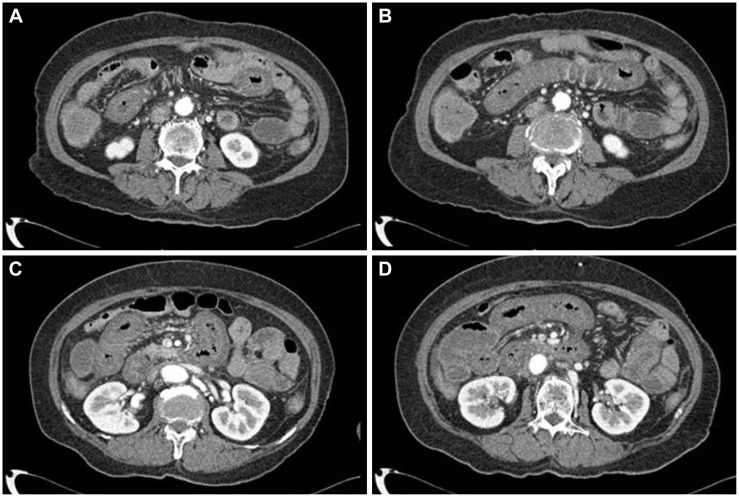 | Fig. 1(A-D) Abdominal computed tomography image showing edematous wall thickening in the duodenum and proximal jejunal loops.
|
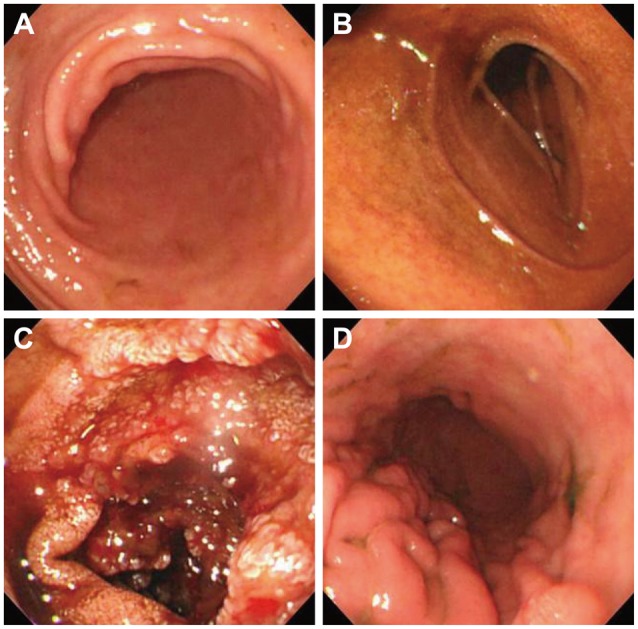 | Fig. 2(A-D) Endoscopy image showing friable and granular mucosal changes with touch bleeding in the second portion of the duodenum. However, there was no involvement of the stomach and duodenal bulb.
|
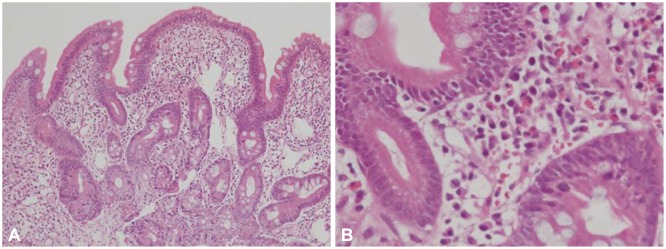 | Fig. 3Pathologic findings showing edematous gastric mucosa and diffusely infiltrated inflammatory cells containing over 100 eosinophils per high power field, consistent with eosinophilic gastroenteritis (A: H&E stain, ×100; B: H&E stain, ×400).
|
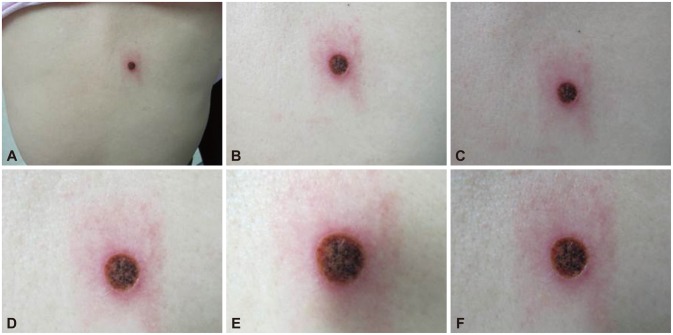 | Fig. 4(A-F) Patch test. A Rhus extract-containing patch was applied for 48 hours, and then removed. Seventy-two hours after application, the skin showed erythematous infiltration with ulceration, which is a strongly positive reaction.
|
 | Fig. 5(A-D) Follow-up endoscopy image showing continued improvement of the mucosal edema and nodularity in the duodenum.
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download