INTRODUCTION
Obesity is a highly prevalent chronic condition associated with significant morbidity and mortality [
123], including increased risk for developing cardiovascular diseases, such as hypertension, heart failure, arrhythmia and coronary artery disease (CAD), as it has maladaptive effects on various cardiovascular risk factors and adverse effects on cardiovascular structure and function [
145]. The prevalence of obesity between 1976–1980 and 2009–2010 among the world's population aged between 20–74 years has more than doubled due to changes in diet and daily life activities [
26].
Comprehensive cardiac rehabilitation (CR) is an effective secondary preventive post-myocardial infarction measure that can reduce the risk of re-infarction and cardiovascular mortality and morbidity [
7]. The increase in the number of obese people has increased the overall risks for CAD. Overweight and obese patients account for >80% of CR participants [
89]. Obesity significantly alters the effectiveness of CR because of the increased risk for CAD and adverse effects on cardiac structure. Studies on Westerners have reported that both obese and non-obese patients revealed significant gains in functional capacity from CR [
51011], and obese patients had smaller gains in functional capacity than non-obese patients [
1011]. Several studies have been performed on understanding the effects of CR on functional capacity in obese and non-obese Western patients; however, few studies have investigated the effectiveness of CR on functional capacity in Koreans.
The classification and the characteristics of obesity in Koreans differ from those of Westerners. The World Health Organization (WHO) recommends using body mass index (BMI) as a screening tool for obesity and defined overt obesity as BMI >30 kg/m
2. BMI between 25–30 kg/m
2 is considered as overweight based on data from Western populations [
12]. However, a BMI of 25 kg/m
2 is considered as the cut-off for obesity in Koreans because these subjects have a higher percentage of body fat and thicker subcutaneous fat at a given BMI and are at substantial risk for comorbidities [
1314]. Results from the 2009–2010 National Health and Nutrition Examination Survey (NHANES) indicate that an estimated 33.0% of US adults aged ≥20 years are overweight (BMI 25–29.9 kg/m
2), 35.7% are obese (BMI 30–39.9 kg/m
2), and 6.3% are extremely obese (BMI ≥40 kg/m
2) [
6]. However, the 2007 Korea National Health and Nutrition Examination Survey (K-NHANES) announced that the overall prevalence of obesity in Korean adults (BMI ≥25 kg/m
2) is 36.7% in men and 25.6% in women (i.e., 4.1% of men and women have BMI ≥30 kg/m
2) [
15]. For this reason, we hypothesized that the effects of CR on functional capacity between obese and non-obese Koreans patients who have suffered an acute myocardial infarction (AMI) may differ from the effects in Westerners. Therefore, this study evaluated the effects of CR on functional capacity and BMI in obese and non-obese Korean patients who have suffered an AMI.
MATERIALS AND METHODS
Subjects
This study recruited 359 Korean patients who were diagnosed with AMI, treated with percutaneous coronary intervention at the Department of Cardiovascular Medicine of Chonnam National University Hospital, and referred to the Cardiac Rehabilitation Center of Chonnam National University Hospital, Gwangju, Korea from 2010 to 2015. We divided the patients into obese group (BMI ≥25 kg/m2) and non-obese group (BMI <25 kg/m2) according to obesity criteria for Koreans. Before entering phase II CR, height and weight of each patient were measured, and BMI was calculated. All patients underwent exercise tolerance test (ETT) successfully before and after CR, and completely finished phase II CR in 6 weeks.
Program
All patients participated in home- or hospital-based phase II CR program, which consisted of risk factor modification, home- or hospital-based aerobic exercise for 6 weeks, and an education and counseling program about psychological, vocational, and sexual aspects of recovery. Exercise sessions comprising of a 10-minute warm-up followed by 30 minutes of aerobic exercise, and a 10-minute cool-down were conducted for 50 minutes. The intensity of exercise was prescribed individually based on target heart rate (HR) calculated as:
In addition, patients were encouraged to exercise at least three times per week. All patients who participated in hospital-based phase II CR program completed exercise sessions based on the prescribed exercise capacity under the supervision of a physical therapist. Patients who participated in home-based phase II CR program were also educated to perform appropriate exercises on a regular basis based on the prescribed exercise capacity and maintain an appropriate perceived exertion level based on their functional capacity evaluated before CR (light, moderate, somewhat hard) during exercise. They were guided to write down their exercise time and frequency in a pocket diary as a mean of confirming exercise performance. After CR, the diaries were collected.
Measurements
Clinical data of all enrolled subjects were collected retrospectively from their medical records, including patient's sociodemographic characteristics, type of myocardial infarction (e.g., STEMI vs. NSTEMI), medication (e.g., anti-platelet agent, β-blocker, angiotensin-convertingenzyme inhibitor [ACEi], and statin), ejection fraction (EF) from two-dimensional echocardiography performed during admission, and risk factors for AMI (e.g., diabetes mellitus, hypertension, hyperlipidemia, and smoking). All patients underwent the ETT on a treadmill (MedTrack ST55; Quinton Instrument, Fort Riley, KS, USA) using the modified Bruce protocol at baseline and after completing CR. We measured the patients' cardiopulmonary function at baseline and during the ETT using an integrated metabolic measurement system (TrueOne 2400 Metabolic system; Parvo Medics, Sandy, UT, USA), including resting HR (HRrest), maximal HR (HRmax), resting systolic blood pressure (SBPrest), maximal systolic blood pressure (SBPmax), maximal metabolic equivalents (METs), total exercise duration (TED), and maximal oxygen consumption (VO2max).
Statistical analysis
The independent t-test was used to compare demographic characteristics between the obese and non-obese groups. The correlations between significant factors and obesity were evaluated by the chi-square test and Spearman correlation analysis. An analysis of co-variance (ANCOVA) adjusted for age was performed to compare cardiopulmonary exercise capacity variables between the groups, and the paired t-test was used to compare before and after phase II CR in each group. The p-values <0.05 were considered significant. All statistical analyses were performed using IBM SPSS Statistics ver. 20.0 software (IBM Corp. Armonk, NY, USA).
RESULTS
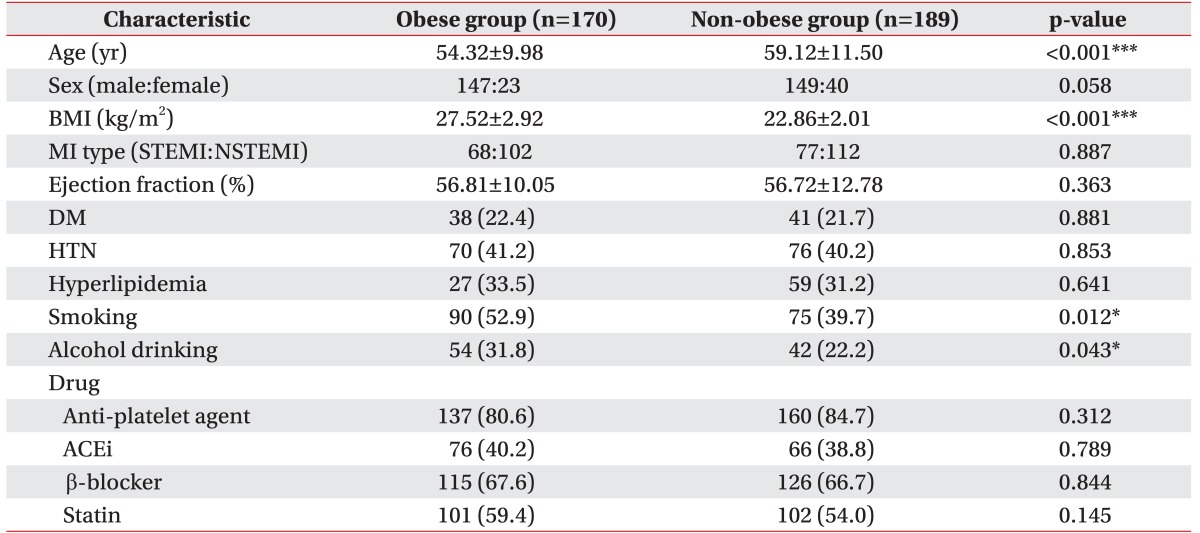
Overall, 359 Korean patients with AMI were evaluated and were divided into obese (BMI ≥25 kg/m
2, n=170) and non-obese group (BMI <25 kg/m
2, n=189). BMI and age were very significantly different between the groups (age: obese group 54.32±9.98 years, non-obese group 59.12±11.50 years, p<0.001; BMI: obese group 27.53±2.92 kg/m
2, non-obese group 22.86±2.01 kg/m
2, p<0.001). Smoking pattern and alcohol drinking were significantly different between the two groups (smoking, p=0.012; alcohol drinking, p=0.042). No differences were detected for sex, type of MI, EF, drugs, diabetes mellitus, hypertension, or hyperlipidemia (
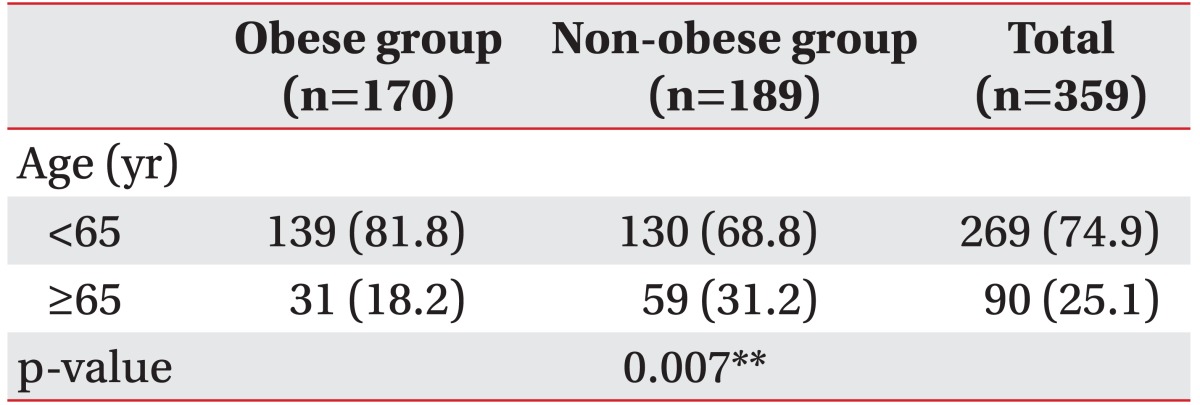
Table 1). Number of old patients (≥65 years; n=90, 25.1%) was much less than young patients (<65 years; n=269, 74.9%), and young patients dominated in the obese group than the non-obese group (p=0.007) (
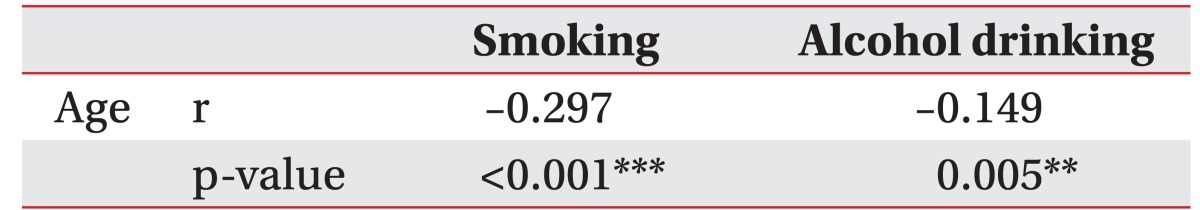
Table 2). Smoking (p<0.001, r=−0.297) and alcohol drinking (p=0.005, r=−0.149) were negatively correlated with age (
Table 3).
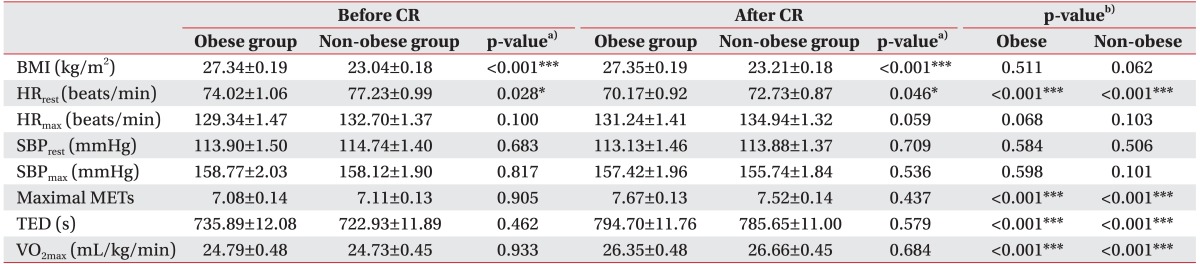
Significant improvements in HR
rest (p<0.001), maximal METs (p<0.001), TED (p<0.001), and VO
2max (p<0.001) were observed in the obese and non-obese groups after CR. Cardiopulmonary exercise capacity from the ETT results at baseline and completion of phase II CR was not different between the groups, except for HR
rest (before CR, p=0.028; after CR, p=0.046), after adjusting for age as a confounding factor. No significant difference in maximal METs at baseline was detected between the two groups (obese group 7.08±0.14; non-obese group 7.11±0.13; p=0.905) (
Table 4).
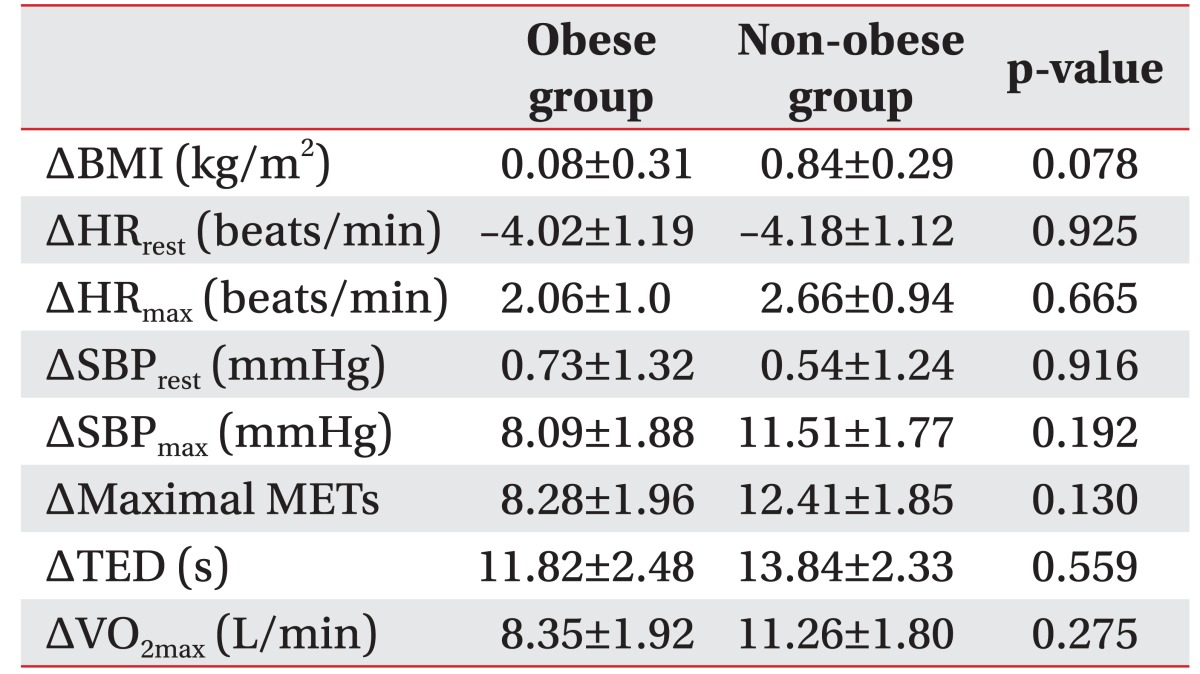
In addition, the change in the rate of each cardiopulmonary exercise capacity variable was used to reduce error caused by differences in the baseline values, but no differences were observed between the groups after adjusting for age as a confounding factor (
Table 5).
DISCUSSION
Obesity is a highly prevalent chronic condition associated with significant morbidity and mortality [
123]. Obesity is an important and independent risk factor that increases the risk of developing cardiovascular diseases, including hypertension, heart failure, arrhythmia, and CAD because it has maladaptive effects on various cardiovascular risk factors and adverse effects on cardiovascular structure and function that increase arterial blood pressure, left ventricular hypertrophy, decreases insulin sensitivity, and adversely affects plasma lipid levels [
145]. Despite the importance of obesity in the development of CAD, very little information is available about the effects of CR on functional capacity between obese and non-obese Korean patients who have suffered an AMI. In this study, we demonstrated the effects of CR on functional capacity between obese and non-obese patients who have suffered an AMI.
In the present study, 47.3% (n=170) of the Korean patients in CR were obese. This result was similar to that of study performed on Western patients (40%) [
5]. Our obese group was about 4.8 years younger than the nonobese group, but no differences in the prevalence of comorbidities such as hypertension, hyperlipidemia, or diabetes mellitus, were found in our cohort. The higher frequency of smoking and alcohol drinking in the obese group than the non-obese group observed in this study may be due to the difference in age between the groups. Obese patients are more vulnerable to chronic health conditions than non-obese patients [
12], and the prevalence of obesity increases steadily among older age groups [
16]. The differences between our study and previous reports are due to the "obesity paradox" between BMI and age. Some potential explanations for the obesity paradox were observed in our study. First, obese patients present earlier in the progression of AMI symptoms and undergo revascularization procedures at a younger age when compared to non-obese patients who have provision for more aggressive treatment during hospitalization. This may be due to concerns that they may be at increased risk for AMI or because of more severe symptoms due to increased myocardial demands that accompany excess weight [
17]. Second, the paradox may be due to selection bias if only a subgroup of the "healthiest" obese patients is surviving to revascularization or being selected for revascularization [
18].
The present study found no significant difference in functional capacity between the obese (METs, 7.08±0.14) and non-obese (METs, 7.11±0.13) groups at baseline before CR, which is different from the concept that obese subjects have lower functional capacity and exercise performance than normal-weight subjects [
919]. However, few studies showed rather lower functional capacity of non-obese patients in comparison to obese patients [
1011]. It is hypothesized that the difference may be due to the difference in age between the obese and non-obese groups, and participation of obese patients who would have a relatively lower risk for the ETT.
Our results show that obese patients may have attained significant and similar functional capacity (METs) and cardiovascular fitness (VO2max) benefits as non-obese patients during phase II CR, as they could exercise longer after completing CR. In addition, no associations were observed between BMI and changes in the rate of any of the cardiopulmonary exercise capacity variables after adjusting for age, indicating that CR improved functional capacity (METs) and exercise performance in both the groups.
Our results are consistent with the findings of most of the reported studies [
511202122]. Several studies reported that CR improves functional capacity in a consistent and significant manner [
9212324]. Lavie and Milani [
511] demonstrated equal improvement in functional capacity in obese and non-obese groups after CR. They also reported that increase in VO
2max and improvement in peripheral muscle mechanics or work efficiency led to improvement in functional capacity [
25]. Ades reported that general cardioprotective effects of exercise in patients with CAD might be due to enhancement in endothelium-dependent vasodilatation of coronary arteries [
21]. CR can also improve adverse effects exhibited by obesity on many CAD risk factors, including arterial pressure, insulin resistance, plasma lipid levels, physical activity, and left ventricular hypertrophy [
5].
However, considering the adverse effect of obesity on exercise performance, the finding in this study that obesity does not influence the effects of CR is difficult to interpret. As not all patients performed hospital-based aerobic exercise, there were some limitations in confirming exercise intensity, frequency, and total amount exactly. Patients might have performed less exercise than the prescription due to several reasons, or total quality and amount of exercise might have been different between the two groups. As explained earlier, obese patients were of young age than non-obese patients and might have been more willing to perform exercise, so there was a possibility that obese patients exercised more than prescribed.
Although there were no significant differences between both the groups, the non-obese group tended to show more improvements in HR
rest, maximal METs, TED, and VO
2max than the obese group. In general VO
2max increases about 10%–15% after CR [
22]. Our obese group showed less improvement (8.35%) in VO
2max as compared to previous studies. One study showed that obese patients have lower work capacity at both baseline and after CR [
10]. Seres et al. [
26] reported association between obesity and reduced exercise performance during each session, which could ultimately result in smaller gains in functional capacity during CR. Furthermore, they demonstrated that a large weight reduction in obese patients was associated with a marked increase in exercise capacity and increased TED and that obese patients performed the same amount of external work with lower cardiorespiratory response and energy consumption as compared to non-obese patients [
26].
HR
rest is one of the most powerful predictors of cardiac mortality [
27]. Obese patients have a significantly higher HR
rest than non-obese patients [
28]. The higher HR
rest in obese patients is due to increased sympathetic tone and reduced vagal tone [
2729]. However, our results show that HR
rest was lower in the obese group as compared to non-obese group before and after CR. This result may also be due to the difference in age between the groups and our obese group had a younger population than the non-obese group. In addition, there is a probability that we made a mistake of including healthy people with lot of muscle mass in obese group based on BMI to classify obesity. Therefore, healthier obese patients having relatively lower risk for the ETT participated in CR. To a certain extent, significant improvement in HR
rest was observed equally in both the groups after CR, suggesting that a regular exercise program corrects the autonomic imbalance and improves cardiopulmonary exercise capacity regardless of obesity.
In contrast with previous study, we found no difference in the change in the rate of BMI after completion of CR in each group. Most of the studies have reported that CR reduces body weight [
911202324]. This difference could be attributed to many factors including inadequate exercise performance, short duration of phase II CR, and inadequate diet. In addition, there is a probability that obese patients in this study were less obese as compared to the ones reported in western studies, because the definition of obesity in this study is not the reported BMI ≥30 kg/m
2, but a BMI ≥25 kg/m
2. Furthermore, there can be a problem in simply applying a definition of BMI as ≥25kg/m
2 to Koreans, because the definition of obesity of Koreans is based on the WHO studies of obesity for Asian Indians, Chinese and Creoles in Asia-Pacific regions [
30].
This study has some limitations. First, because this study was a single center study, the results in this study are difficult to accept as a general characteristic in Koreans. More structured multi-center studies are needed to represent characteristics of Koreans in CR. Second, in this study, phase II CR programs consisted of home- or hospital-based aerobic exercise. We recommended patients to perform hospital-based aerobic exercise to the extent possible, but most of the patients performed home-based aerobic exercise due to economical, occupational, geographical, or time factors. They were educated enough to exercise regularly and record their exercise time and frequency in a pocket diary provided by doctor, physical therapist and nurse. Most of the patients recorded their exercise performance and completed the prescribed amount of exercise, but some patients lost their diaries, or did not record, and not all the recorded data were reliable. There were some limitations in confirming exercise performance exactly, and the amount of exercise may not have been enough as prescribed. These discrepancies might affect overall functional capacity in both the groups after CR. Third, we used BMI, which is a measure of body fat based on height and weight, as it is the most commonly used tool in epidemiological studies. However, we did not account for peripheral or central adiposity, lean body mass, or body fat percentage because body weight is the sum of fat, muscle, visceral organs, and bone. Thus, misclassification of body composition using BMI would be expected to predispose our results. Further studies are needed to investigate the effects of CR on obesity using parameters, such as fat free mass index, waist circumference, and the waist-to-hip rate, to assess abdominal obesity. Fourth, this study was retrospective in nature and short-termed, so selection bias could have been present. No improvement was noted in either of the groups after 1 month of phase II CR. It is hypothesized that the follow-up period might have affected the changes in BMI after CR. More long-term follow-up is needed to understand the effects of CR on BMI and the association between changes in BMI and functional capacity in Koreans.
We hypothesized that the effects of CR on functional capacity between obese and non-obese Koreans patients who have suffered an AMI may differ from the effects in Westerners because of the racial and ethnic differences in diagnostic criteria for obesity and fat distribution as explained earlier. However, there were no significant differences in the results between this study and studies concentrating on Western areas due to differences in race and ethnicity. There are some limitations to conclude that the results in this study represent characteristics of Koreans. Nevertheless, results from this study show that CR can effectively improve functional capacity in obese and non-obese patients. Well-structured multi-center studies are needed to investigate the effects of CR on functional capacity in obese and non-obese Korean patients with AMI.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download