Abstract
Objective
To evaluate the therapeutic effect of a Tibia Counter Rotator (TCR) with toe-out gait plate (GP) upon tibial internal torsion by a comparative analysis of transmalleolar angle (TMA) and gait analysis with GP alone.
Methods
Twenty participants with tibial internal torsion were recruited for this study. Each 10 participants were included in group A with TCR and GP application and in group B with GP application only. The TMA and the kinematic results were used for the evaluation of the therapeutic effects of orthoses.
Results
Within each group, TMA showed a significant increase after treatment. Group A showed a continuous improvement up to six months, however, group B showed an improvement up to five months only. Group A showed a significantly higher correction effect than group B after treatment. Regarding kinematic data, both groups showed a significantly decreased mean ankle adduction angle after treatment. However, group A showed a significantly lower mean ankle adduction angle than group B after six months.
Intoeing gait is a common gait problem in children, and tibial internal torsion is known to be one of the most common causes of intoeing gait [1,2,3,4]. Tibial internal torsion is a condition in which the distal tibial articular surface (ankle joint) is rotated internally along the proximal tibial articular surface (knee joint) in the transverse plane toward the body's midline [1]. According to some reports, tibial torsion may be medial or neutral at birth, however, as the child grows, lateral torsion develops and the adult level of 18°-23° of lateral torsion has been reached at seven or eight years [1,5,6,7,8].
However, in Asian people, such as in Korean and Japanese, who have the lifestyle of kneeling on the floor with internal rotation of the legs, tibial internal torsion commonly remains, even in older age, despite the natural course of tibial torsion angle [1,9]. Tibial internal torsion or excessive lateral torsion may cause esthetical, functional or psychological problems and may also induce degenerative arthritis in an older age. Therefore, several previous studies have recommended a proper treatment of severe tibial internal torsion at an early age [1,10,11,12].
A toe-out gait plate (GP) has commonly been used for the treatment of tibial internal torsion due to its advantages of lightness, better comfort and adjustable flexibility [13,14]. The therapeutic effect of GP upon tibial internal torsion has been reported in previous studies [13,14]. It was reported that Tibia Counter Rotator (TCR) can be an effective therapeutic tool in the management of tibial internal torsion [1,15,16]. It changes the direction of growth of tibial physeal cells and leads to a correction of a tibial internal torsion [1,15,16]. However, although the purpose of the correction of tibial internal torsion is to correct the intoeing gait pattern, no one has evaluated the effect of the tibia correction device using gait analysis on tibial internal torsion yet [1,13,16].
We investigated the therapeutic effect of TCR with GP by a comparative analysis of transmalleolar angle (TMA) and by a gait analysis with GP alone upon tibial internal torsion.
The study population was selected from children who visited the foot clinic of Yeungnam University Medical Center between January 2012 and August 2012. The diagnosis was made using clinical symptoms, image findings and physical examinations by two expert physiatrists. Participants whose diagnosis was in disagreement among two physiatrists were excluded. Patients were recruited according to the following criteria: 1) participants aged between 4 and 11 years; 2) participants whose TMA was less than 0° at the time of initial evaluation [1,5,17]; 3) no definite spasticity, somatosensory problem or abnormal neurologic conditions, including developmental delay; 4) no history of orthopedic surgery or traumatic event on lower extremities during the study period; 5) no history of significant cardiopulmonary, metabolic or neuromuscular condition, including tumors and inflammation; and 6) volunteers whose parents had applied to this study. Fifty-one patients diagnosed with tibial internal torsion were originally selected. Of 51 participants, 16 did not meet the age criterion, 12 were diagnosed with developmental delay, and three had a traumatic event on lower extremities during the study period and were excluded from the study participation therefore (Fig. 1). Finally, 20 participants (40 limbs; 10 males and 10 females; mean age 6.05±2.54 years; range 4-11 years) were included in the study. Of 20 participants were 10 participants (20 limbs; 3 males; mean age 6.80±2.74 years; range 4-10 years) randomly included in group A, the TCR with GP group, and the remaining 10 participants (20 limbs; 7 males; mean age 5.30±2.21 years; range 4-11 years) were included in group B, the GP alone group. We used the block randomization method to balance the numbers in this study. After randomization, all orthoses were individually molded and fitted. The study was approved by the Institutional Review Board at our hospital. Also, a written informed consent was obtained from the parents of all participants.
TCR consisted of well-padded straps (Velcro), foot plate, and metal brace (Fig. 2). The initial foot plate setting angle was the end point of leg lateral motion with a flexed knee position [15]. The patients visited our clinic monthly. If the patient had accommodated to a setting angle, we increased the foot plate angle by 5° [15] (Fig. 2C). However, foot plate angle was not changed in participants who did not accommodate to the setting angle or who did not show definite improvement compared with previous visits. The goal of treatment using TMA was 10° of external rotation or normal value as referred by Staheli et al. [2], Valmassy and Stanton [5], and Vanderwilde et al. [17]. The type of GP used in this study was a gait plate, which was composed of a polypropylene shell. All TCR and GP (Biomechanics Technology Co. Ltd., Goyang, Korea) were individually molded and fitted by one expert podiatrist.
The severity of tibial internal torsion was evaluated by TMA for all participants. TMA was measured monthly for overall 6 months after GP and/or TCR application [5,6,8,9,18]. TMA was measured using a gravity goniometer in the supine position after marking the medial malleolus of the tibia and lateral malleolus of the fibula while extending the knee to the coronal plane [5,6,8,9,18] (Fig. 3). The negative value refers to the internal rotation of the tibia, whereas the positive value refers to the external rotation. The TMA was independently assessed by an expert physiatrist and expert podiatrist who were unaware about the other assessment results. All participants were assessed by these two experts. The acquired data were averaged for statistical analysis.
Three-dimensional gait analysis was performed using a computerized VICON T40 motion analysis system with 12 infrared cameras (Oxford Metrics Inc., Oxford, UK) for the measurement of kinematic data during the gait cycle. During gait analysis, 14-mm diameter reflective markers were attached directly by the same trained investigator over the following anatomic locations of both pelvis and lower extremities: anterior superior iliac spines, posterior superior iliac spines, midway between the posterior superior iliac spines, lateral epicondyles of the knee joints, lateral malleoli, heels, second metatarsals and lateral aspects of the thigh and calf segments [19,20]. Gait analysis was performed before and six months after application of orthoses. Prior to performance of gait analysis, a static trial was captured in a static position in order to establish the relationship among the markers. All participants were instructed to walk barefoot at their self-selected speed along 10 m with the markers in place. For averaging of data, all participants walked at least three trials. Also each walking trial included more than three gait cycles. Motion capture, modeling and all trials were processed using VICON Nexus 1.7 software and kinematic data were computed using POLYGON software. All results of walking trials were accumulated and averaged. Data were normalized based on the entire gait cycle and kinematic parameters were measured.
Regarding kinematic data of the participants, positive mean ankle adduction angle refers to adduction of the ankle, whereas negative angle refers to abduction. Ankle adduction angle is the angle between the foot vector and the sagittal axis of the tibial shank, projected to the foot transverse plane. In terms of hip and knee internal rotation angle, a positive value refers to hip and knee internal rotation, whereas a negative value refers to hip and knee external rotation.
Independent sample t-test was used for comparison of demographic and clinical data of the participants except non-parametric data. Pearson chi-square test was used for non-parametric data including sex. One-way analysis of variance for repeated measurements followed by post-hoc analysis with Bonferroni adjustment was performed to analyze changes in each group for TMA and kinematic data of gait analysis including time effect. Comparative analysis between two groups for TMA and kinematic data of gait analysis was also performed. The inter-rater reliability of TMA was assessed to determine the intra-class correlation coefficient (ICC). The inter-rater ICC value of TMA between the two experts was 0.906, revealing excellent reproducibility. The Statistical Package for Social Sciences (SPSS) ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. The adopted level of significance was p<0.05.
A summary of demographic and clinical data for all 20 participants is shown in Table 1. In all variables, no significant difference was observed between the two groups. None of the participants dropped out during this study and no side effects, including moderate to severe pain or somatosensory problem on lower extremities were reported.
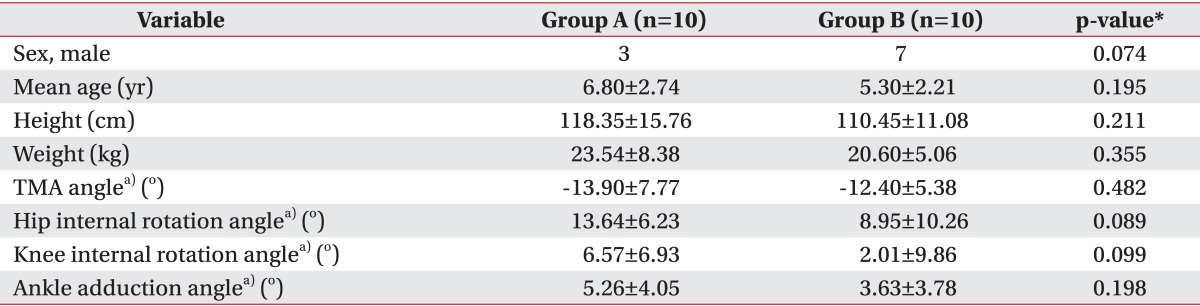
In group comparison, both groups showed significantly increased TMA six months after treatment (Fig. 4, Table 2). The mean TMA of group A improved from -13.9° to 10.9°. Group B showed an increased TMA from -12.4° to 2.1°. In detail, group A showed a sustained significant correction effect to 6 months of orthoses application, however, group B showed significant improvement to only 5 months, not from 5 to 6 months of therapeutic session. We also compared the therapeutic outcomes between the two groups. Group A showed a significantly increased mean value of TMA than group B after six months of treatment, although no significant difference was observed before the therapeutic session. In addition, no significant difference was observed between both groups from pretreatment to one month after treatment. However, group A showed a significantly increased mean value of TMA, compared with group B, from one month to two months and this difference continued to six months. Also, group A showed a significantly higher amount of interval change from pretreatment to one month, and this significant difference was maintained up to six months.
Regarding kinematic data, both groups showed a significantly decreased mean ankle adduction angle after treatment (Fig. 5, Table 2). The mean ankle adduction angle of group A improved from 5.26° to -7.87°. Group B also showed an improved ankle adduction angle, but the amount of change was 3.63° to 0.79° smaller than that of group A. We also compared the therapeutic progress between the two groups. No significant difference was observed between the groups before treatment (Table 1). However, after six months, group A showed significantly lower mean ankle adduction angle than group B. For the hip and knee angle, no significant difference was observed between group A and B, and no significant improvement was observed after the therapeutic session.
In the current study, we demonstrated the therapeutic effect of TCR on tibial internal torsion. The TCR with GP group showed a significantly better outcome and continued correction force compared with the GP only group.
The tibia correction device was first introduced as a tibial torsion transformer by Bresnahan and Lubert [15] in 1992. They reported that tibial torsion transformer had an advantage of better comfort because the feet are not linked together [15]. Since then, a few researchers have reported on the effectiveness of the device for treatment of pediatric intoeing [1,16]. In 2007, Song et al. [1] investigated the therapeutic effect of the device using TMA in 149 pediatric patients with tibial internal torsion. In this study, TMA increased from -10.93° to 7.54° after 12 months of treatment [1]. Another study by Lee et al. [16], measured the thigh foot angle and computed tomography (CT) for assessment of the tibia internal brace effect in 20 pediatric participants with tibial internal torsion. Thigh foot angle improved from -12.2° to 5.0° and tibial angle by CT increased from 22.6° to 26.0° [16]. In the current study, we also found that application of GP and/or TCR improved tibial internal torsion by increase of TMA and by decrease of mean ankle adduction angle. All participants in both groups were applied GP. However, the amount of improvement was significantly greater in the TCR with GP group than in the GP only group. Therefore, the authors suppose that these results can be attributed to the therapeutic effect of the tibia correction device on intoeing gait. The device could influence on capsule and/or ligament around knee joint as well as tibial growth plate [15]. Previous study using CT reported increased bony tibial torsion angle as much as 3.4° after treatment for 13 months [16]. In this study, participants showed increased TMA more than 20° after treatment. This result implies that TCR influences mainly on capsule and ligament than tibial growth plate itself. In addition, above-mentioned change was prominent especially during first one month of treatment. Therefore, we suppose that the improvement of TMA was due to the change of soft tissues rather than that of tibial bone. The tibia correction devices are used nowadays due to their benefits of comfort compared with the other night orthosis, including a Denis-Browne splint which is totally bounded [7,21]. Patients in whom the device treatment was applied could have freedom of comfortable movement of hip joint. In addition, patients with a unilateral tibial internal torsion can be treated with a single orthosis to the affected extremity without application of orthosis to the other leg. In addition, we used a unit equipped in the device to accommodate foot plate angle quantitatively. However, too rapid correction of tibial internal torsion angle could cause pronation of the subtalar and midtarsal joints; therefore, application of the device has to be applied cautiously and to check participants' compliance [7,16]. In the current study, we checked participants' compliance as well as TMA monthly. There were none of the participants who dropped out during this study or who reported side effects, such as pain.
There were various measures for tibial internal torsion, such as conventional CT, three-dimensional CT, TMA, and thigh foot angle [5,6,8,18,22,23,24,25]. A previous study by Abel et al. [23] reported an accuracy of three-dimensional CT upon the femoral neck-shaft angle over 99% and of conventional CT over 96%. However, due to its lower cost and ease, TMA using a gravity goniometer has frequently been used in the field of rehabilitation [5,6,8,18,22,24,25]. Lang and Volpe [22], who compared CT with TMA, reported a good correlation between these two measurements. Also, another study by Lee et al. [18] reported that TMA and thigh foot angle are reliable and valid measurement tools, compared with two-dimensional CT. Further, another study conducted by Lee et al. [26] reported a significant correlation between CT and clinical measurement data of thigh foot angle and femoral internal torsion angle. The reliability and validity of the VICON motion analysis system have been well-established [13,19]. Therefore, we compared the TCR and GP groups with the GP only group using gait analysis as well as TMA and determined its therapeutic effect for correction of intoeing gait.
In conclusion, we found that TCR with GP could be an effective therapeutic modality in pediatric patients who showed intoeing gait due to tibial internal torsion. To the best of our knowledge, no study has been reported yet on the therapeutic effect of TCR with GP using gait analysis. However, the current study has its limitations, including a small number of participants and a short study period. It would be recommended to conduct further complementary studies involving larger case numbers with long-term follow-up.
ACKNOWLEDGMENTS
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Korea (No. A084177).
References
1. Song DH, Lee Y, Eun BL, Lee KJ, Kang SK, Vaq SG, et al. Usefulness of tibia counter rotator (TCR) for treatment of tibial internal torsion in children. Korean J Pediatr. 2007; 50:79–84.

2. Staheli LT, Corbett M, Wyss C, King H. Lower-extremity rotational problems in children: normal values to guide management. J Bone Joint Surg Am. 1985; 67:39–47. PMID: 3968103.

3. Thackeray C, Beeson P. In-toeing gait in children: a review of the literature. Foot. 1996; 6:1–4.

4. Jacquemier M, Glard Y, Pomero V, Viehweger E, Jouve JL, Bollini G. Rotational profile of the lower limb in 1319 healthy children. Gait Posture. 2008; 28:187–193. PMID: 18201887.

5. Valmassy R, Stanton B. Tibial torsion: normal values in children. J Am Podiatr Med Assoc. 1989; 79:432–435. PMID: 2778678.
6. Valmassy RL. Biomechanical evaluation of the child. Clin Podiatry. 1984; 1:563–579. PMID: 6536409.
8. McDonough MW. Angular and axial deformities of the legs of children. Clin Podiatry. 1984; 1:601–620. PMID: 6536411.
9. Song DH, Eun BL, Park SH, Lee JY, Tockgo YC. Tibial torsion in children of the Jeju area. Korean J Pediatr. 2005; 48:75–80.
10. Turner MS. The association between tibial torsion and knee joint pathology. Clin Orthop Relat Res. 1994; (302):47–51. PMID: 8168321.

11. Turner MS, Smillie IS. The effect of tibial torsion of the pathology of the knee. J Bone Joint Surg Br. 1981; 63B:396–398. PMID: 7263753.

12. Yagi T. Tibial torsion in patients with medial-type osteoarthrotic knees. Clin Orthop Relat Res. 1994; (302):52–56. PMID: 8168322.

13. Mabuchi A, Kitoh H, Inoue M, Hayashi M, Ishiguro N, Suzuki N. The biomechanical effect of the sensomotor insole on a pediatric intoeing gait. ISRN Orthop. 2012; 2012:1–5.

14. Redmond AC. An evaluation of the use of gait plate inlays in the short-term management of the intoeing child. Foot Ankle Int. 1998; 19:144–148. PMID: 9542984.

15. Bresnahan PJ, Lubert MA. The tibial torsion transformer. J Am Podiatr Med Assoc. 1992; 82:42–44. PMID: 1545370.

16. Lee SY, Jung YT, Lee SM. Effect of the tibia counter rotator orthosis for tibial internal torsion children: a preliminary study. J Korean Acad Rehabil Med. 2009; 33:470–476.
17. Vanderwilde R, Staheli LT, Chew DE, Malagon V. Measurements on radiographs of the foot in normal infants and children. J Bone Joint Surg Am. 1988; 70:407–415. PMID: 3346265.

18. Lee SH, Chung CY, Park MS, Choi IH, Cho TJ. Tibial torsion in cerebral palsy: validity and reliability of measurement. Clin Orthop Relat Res. 2009; 467:2098–2104. PMID: 19159112.

19. Chambers C, Goode B. Variability in gait measurements across multiple sites. Gait Posture. 1996; 4:167.

20. Westhoff B, Hirsch MA, Hefter H, Wild A, Krauspe R. Wie reliable sind informationen aus der 3D-ganganalyse? Sportverletz Sportschaden. 2004; 18:76–79. PMID: 15164292.
21. Weseley MS, Barenfeld PA, Eisenstein AL. Thoughts on in-toeing and out-toeing: twenty years' experience with over 5000 cases and a review of the literature. Foot Ankle. 1981; 2:49–57. PMID: 7030890.

22. Lang LM, Volpe RG. Measurement of tibial torsion. J Am Podiatr Med Assoc. 1998; 88:160–165. PMID: 9581433.

23. Abel MF, Sutherland DH, Wenger DR, Mubarak SJ. Evaluation of CT scans and 3-D reformatted images for quantitative assessment of the hip. J Pediatr Orthop. 1994; 14:48–53. PMID: 8113372.

24. Stuberg W, Temme J, Kaplan P, Clarke A, Fuchs R. Measurement of tibial torsion and thigh-foot angle using goniometry and computed tomography. Clin Orthop Relat Res. 1991; (272):208–212. PMID: 1934735.

25. Liu X, Kim W, Drerup B, Mahadev A. Tibial torsion measurement by surface curvature. Clin Biomech (Bristol, Avon). 2005; 20:443–450.

26. Lee S, Choi KS, Jeung IS, Lee JE, Yang SM, Lee SM. Physical examination and computed tomography in children with toe in gait. J Korean Acad Rehabil Med. 2011; 35:61–66.
Fig. 1
Flowchart of subject selection. Fifty-one participants diagnosed as tibial internal torsion. Of 51 participants were 16 participants excluded who did not meet the age criterion: 12 participants were diagnosed as developmental delay and 3 participants had traumatic events on lower extremities during the study period. Finally, 20 participants were included in the study. A clinical coordinator unaware of the clinical data of participants randomized the subjects into two groups. Among 20 participants, 10 participants were included into group A with Tibial Counter Rotator (TCR) and toe-out gait plate (GP). The remaining 10 participants were included into group B with GP application only.
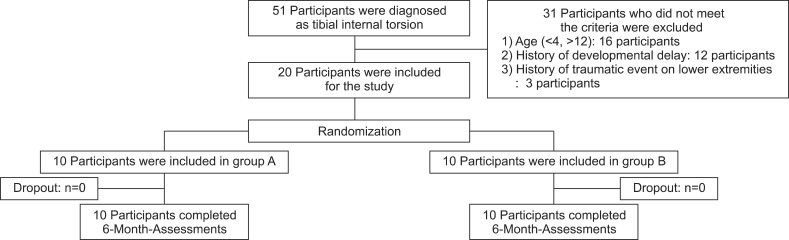
Fig. 2
Tibial Counter Rotator (TCR). (A) Anterior view, (B) oblique view, and (C) inferior view. TCR consisted of well-padded straps (Velcro), foot plate and metal brace (A, B). The initial setting angle was the end point of leg lateral motion with a flexed knee position. Foot plate angle was increased using units of 5° as the patients visited the foot clinic monthly (C). All participants were instructed to apply TCR with a flexed knee position during sleep for at least 3 hours a day.
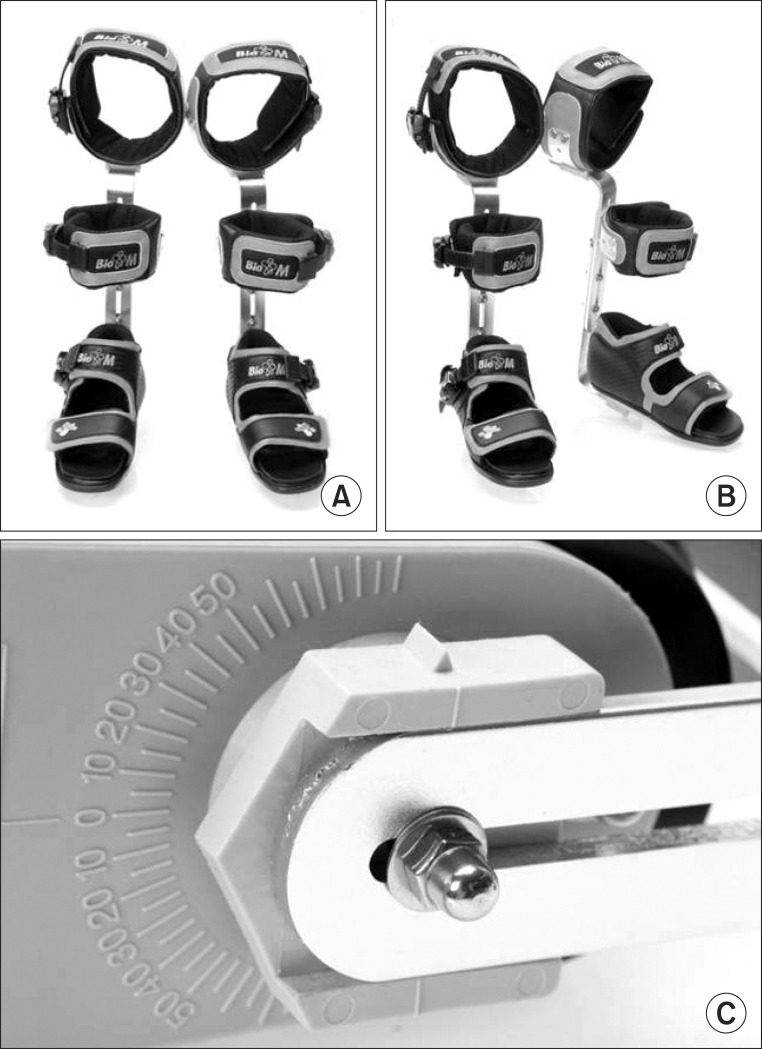
Fig. 3
Measurement of transmalleolar angle (TMA). TMA was measured using a gravity goniometer in the supine position after marking the medial malleolus of the tibia and lateral malleolus of the fibula while extending the knee to the coronal plane [5,6,8,9,18]. The negative value refers to the internal rotation of the tibia, whereas the positive value refers to the external rotation.
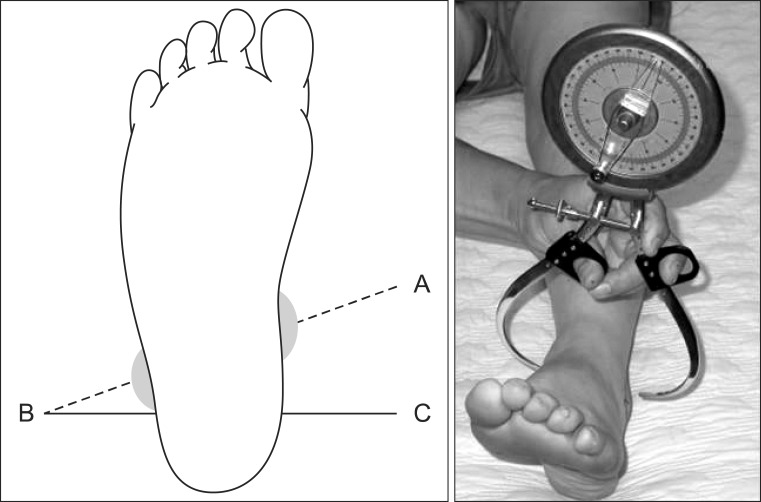
Fig. 4
Comparative results of transmalleolar angle within both groups. TCR, Tibial Counter Rotator; GP, toe-out gait plate. *p<0.05.
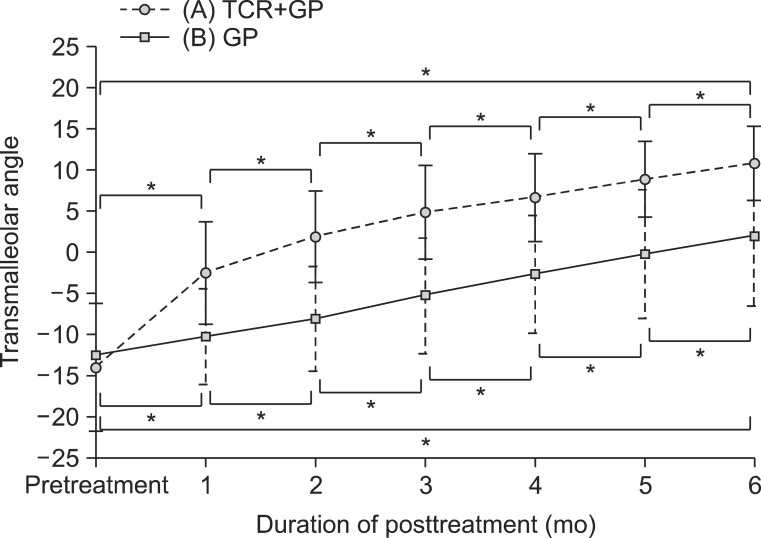
Fig. 5
Comparative results of mean foot ankle adduction angle in both groups. TCR, Tibial Counter Rotator; GP, toe-out gait plate. *p<0.05.
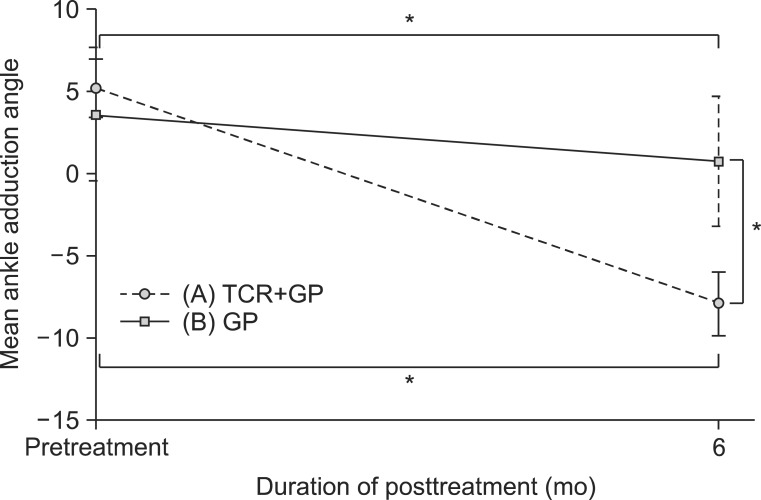
Table 2
Change in variables from pretreatment to six months after treatment
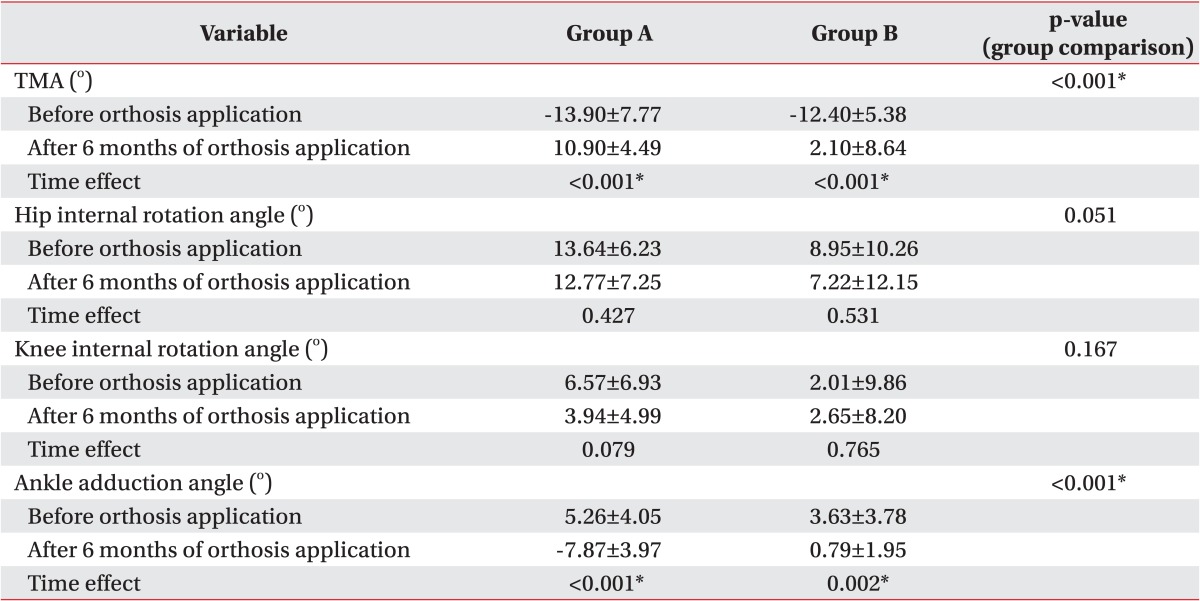
Values are presented as number or mean±standard deviation.
Group A was defined as the TCR with GP group and group B was defined as the GP alone group.
TMA, transmalleolar angle; TCR, Tibial Counter Rotator; GP, toe-out gait plate; time effect, temporal changes of therapeutic effect of orthosis in each group after treatment.
*p<0.05.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download