Abstract
We report our experience using Onyx for embolization of dural arteriovenous fistula (DAVF) under dual lumen balloon catheter flow arrest. Transfemoral cerebral angiography revealed a superior sagittal sinus (SSS) DAVF that was supplied via multiple branches of the external carotid arteries, the right anterior cerebral arteries, and the meningeal branches of the internal carotid artery. There was no anterograde venous drainage through the SSS, and venous drainage was almost retrograde through the medullary and cortical veins. Under general anesthesia, a transvenous approach was utilized to place the microcatheter close to the fistula site. After intravenous embolization with various coils, DAVF was partially occluded; Balloon catheter gained access to the DAVF via the right middle meningeal artery. We injected Onyx through the Scepter C catheter, after which DAVF was nearly completely occluded. Balloon-assisted Onyx embolization is a feasible and effective approach for the management of DAVF.
Endovascular intervention has quickly evolved to become the first treatment option for most dural arteriovenous fistulas (DAVFs) [1]. Agents used for DAVF embolization include, Onyx, polyvinyl alcohol particles, coils, and N-butyl cyanoacrylate. Among them, Onyx has many advantages for use in endovascular treatment. Its slow solidification allows for a more prolonged and controlled injection that enables a larger number of feeding vessels to be penetrated. For this reason, treatment of DAVFs with cortical venous reflux (CVR) now includes transarterial Onyx-based embolizations [2].
Since it is considered a relatively controllable agent, Onyx is now considered a primary option. Regarding Onyx embolization of DAVF, optimal wedging of the microcatheter and flow control technique is important. Proper penetration of Onyx depends on wedging the microcatheter and generating a sufficient plug around the distal end of the catheter. For safe reflux and proper penetration of Onyx, various devices such as balloons have been used. Herein, we report the case of a 77-year-old man with DAVF who underwent Onyx embolization using a new dual lumen balloon catheter (Scepter C; Microvention, Tustin, California, USA) to control blood flow.
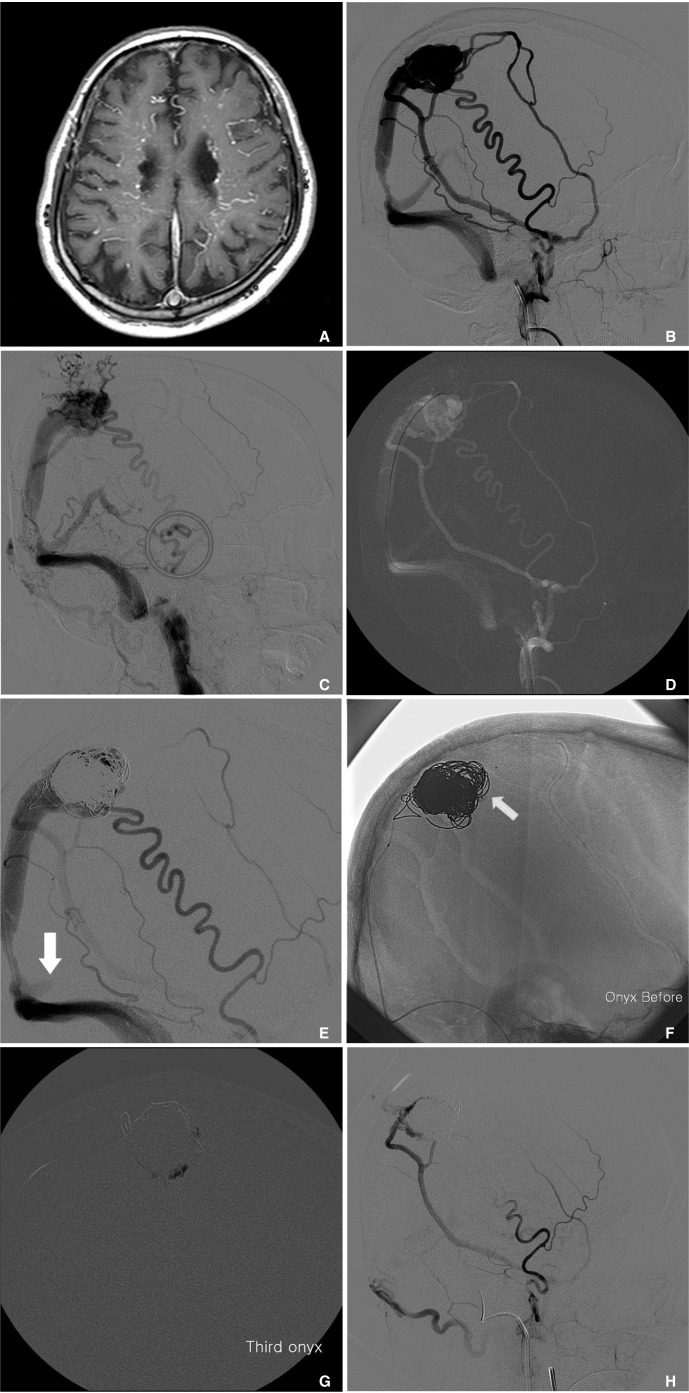
A 77-year-old man presented with gait disturbance that had persisted for 1 month. He had a history of dementia and depression for which he had received medication. Brain magnetic resonance imaging (MRI) revealed atrophy and venous congestion. Computed tomography (CT) angiography revealed DAVF of the superior sagittal sinus (SSS) (Fig. 1A). Transfemoral cerebral angiography (TFCA) showed that the SSS DAVF was supplied via multiple branches of the external carotid artery (ECA), the right anterior cerebral arteries, and the meningeal branches of the internal carotid artery (ICA) and vertebral artery (Fig. 1B). Anterograde drainage was not observed through the SSS, while drainage through the vein of Labbe and sphenoparietal sinus was main. TFCA revealed venous hypertension and galenic venous drainage. Furthermore, TFCA showed CVR (Fig. 1C). The DAVF was large and complex. According to Borden classification, the DAVF was type 2.
Embolization of DAVF was performed under general anesthesia using a biplanar fluoroscopic unit. Right femoral artery and left femoral vein were punctured with an angiography needle (18 gauge). A 6Fr Envoy guiding catheter (Codman, Miami Lakes, Florida, USA) was then introduced to the right ECA. Another Envoy catheter was introduced to the right internal jugular vein through the venous root. Heparin was administered in order to achieve a targeted activated coagulation time of 250-300s throughout the procedure. Using a transvenous approach, a microcatheter (Echelon 10) was placed at the fistulous sac of the SSS (Fig. 1D). Eleven coils (GDC 360 Standard 24 mm × 40 cm (×7), 22 mm × 40 cm (×3), 20 mm × 33 cm (×1)) were inserted through the microcatheter (Echelon 10). Another microcatheter (Prowler Select 18) was subsequently used to insert non-detachable coils; this was placed using Synchro 14 microwire. Other coils (Interlock Coil 14 mm × 30 cm (×2), 14 mm × 20 cm (×1), 12 mm × 30 cm (×1), 12mm × 20 cm (×1), Nester Coil 10 mm × 14 cm (×2), 6 mm × 14 cm (×3), 4 mm × 14 cm (×3)) were inserted through this microcatheter. Following intravenous coil embolization using various coils, DAVF was occluded partially. Angiography revealed that retrograde drainage through the fistula remained (Fig. 1E). A Scepter C balloon catheter (4×15 mm) was placed at the most distal segment of the middle meningeal artery (MMA). The tip of the balloon microcatheter was positioned at the DAVF. After that, balloon inflation and deflation was successfully carried out. (Fig. 1F) In order to occlude any residual fistula, Onyx18 was then injected through the dual lumen balloon catheter positioned in the MMA. Over a period of 22 minutes, a total of 4.5 cc of Onyx18 was injected, after which the DAVF was almost completely occluded (Fig. 1G). Following embolization, angiography revealed no arteriovenous shunting or CVR (Fig. 1H). The balloon was deflated by syringe suction without difficulty. The catheter was then immediately removed without any noticeable adherence to the Onyx cast. Procedure related complications were not observed. The patient symptoms were unchanged during hospitalization.
Arteriovenous fistulas (cerebral or spinal, pial, or dural) are characterized by direct communication between 1 or more arterial feeders into a single draining vein without an intervening tangle of vessels (nidus) [3]. Progressive thrombosis of the sinuses may lead to venous congestion of cortical veins, causing global deficits such as dementia, seizures, Parkinsonism, and cerebellar symptoms. Despite the stable clinical behaviors ascribed to benign DAVF, these patients need to be monitored continuously for any changes in symptoms [1].
Regarding angiographic findings, the venous drainage pattern is the most important predictor of clinical behavior, whereby DAVF with CVR exhibits a much higher incidence of hemorrhage and venous infarction. Furthermore, variceal or aneurysmal venous dilatations, thrombosis of venous outflow, leptomeningeal drainage, and galenic venous drainage are related to poor natural history, more aggressive clinical symptoms, and poor long-term clinical outcome [1, 4-6]. SSS DAVF can exhibit symptoms of venous congestion, such as seizures, hydrocephalus, papilledema, and dementia.
Regarding treatment, endovascular intervention has quickly evolved to become the first treatment option for most DAVFs [1]. Treatment of DAVF with CVR now includes transarterial Onyx-based embolizations [2]. This treatment approach is now considered as a primary option. However, transvenous coil embolization is still preferred for the management of DAVFs involving arterial branches that supply cranial nerves, predominant internal carotid artery feeders and potential extracranial-intracranial collateral anastomosis [5]. Onyx is a permanent non-adhesive liquid polymer embolic agent that has shown favorable results compared to N-butyl cyanoacrylate. This is due to its non-adhesive properties and low precipitation rates, which provide longer and more controlled injections. The ability to stop Onyx infusion and analyze its progression can minimize complications from unwanted infusion, thus preventing unwanted vessel occlusion through dangerous anastomoses [1, 7, 8]. Using reflux as a plug, operator creates a forward flow of Onyx. This is called the "Plug and push technique." However, Onyx requires a learning curve in order to avoid unwanted reflux and to control flow. Furthermore, Onyx has several disadvantages. To create a proximal plug, Onyx requires time; this can lead to excessive fluoroscopy times and radiation exposure. Alopecia, radiation burns, and delayed health risks can follow [1, 8, 9]. The cost of an Onyx procedure is also significantly greater than procedures performed with NBCA. Onyx can adhere to the microcatheter and cause breakage. Migration of Onyx can create a pulmonary embolism.
In complex intracranial DAVF, the DAVF may require retreatment or multimodal treatment (surgery, radiosurgery etc.). In these cases, a combination of transvenous and transarterial approaches results in higher obliteration rates [1, 5, 7]. The template is made of coil. After that, adding Onyx onto the template is the usual method [5, 10]. It is similar to the Reinforced Concrete Method. Proximal reflux of Onyx can compromise the normal vasculature and cause retention of the microcatheter. Balloons have been successfully used to modulate flow through high-flow AVFs and malformations. If the balloon actually occludes the feeding artery, risk of the Onyx plug migrating should be minimal [7, 9].
Onyx embolization via a dual lumen balloon catheter allows for great penetration without the necessity of creating the long plug process that is required for the usual "plug and push technique," or the use of detachable tip microcatheters. Inflation of a proximal balloon creates a "plug," allowing for the immediate forward flow of Onyx. Additionally, the balloon increases the proximal resistance in the feeder, resulting in better control of the reflux and enhanced distal penetration [5, 7, 8].
Scepter C is a dual lumen polyurethane balloon catheter, which allows for balloon inflation and Onyx injection via 2 different lumens. Compared with the use of an over-the-wire-type single lumen balloon in tandem with another Onyx delivering microcatheter, the Scepter C has some advantages. First, navigation of another device is not required. Second, it completely eliminates the risk of Onyx reflux. Third, because it utilizes a 0.014" wire, it navigates better than a single lumen balloon that uses 0.010" wire [10]. Furthermore, the short distance between the catheter tip and the distal tip marker relatively presents the real position of the distal tip.
In this case, the patient with SSS DAVF presented with hydrocephalus and dementia was treated by endovascular intervention. A combination of the transvenous and transarterial approaches was performed. The coils that were inserted through the venous root worked as a template. The Scepter C balloon catheter was introduced through the arterial root, after which Onyx was injected through the root during balloon inflation. The patient's condition did not change. DAVF was effectively treated.
It is appropriate to select a combination of transarterial and transvenous embolization for complex dural arteriovenous fistulas. Using a Scepter C balloon catheter during onyx embolization of DAVFs helps prevent onyx reflux and improves its penetration; thus, this is a feasible and effective alternative approach for the management of DAVFs.
References
1. Hu YC, Newman CB, Dashti SR, Albuquerque FC, McDougall CG. Cranial dural arteriovenous fistula: transarterial onyx embolization experience and technical nuances. J Neurointerv Surg. 2011; 3:5–13. PMID: 21990779.

2. Cognard C, Januel AC, Silva NA Jr, Tall P. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: new management using onyx. AJNR Am J Neuroradiol. 2008; 29:235–241. PMID: 17989374.

3. Hoh BL, Putman CM, Budzik RF, Ogilvy CS. Surgical and endovascular flow disconnection of intracranial pial single-channel arteriovenous fistulae. Neurosurgery. 2001; 49:1351–1363. PMID: 11846934.

4. van Dijk JM, ter Brugge KG, Willinsky RA, Wallace MC. Clinical course of cranial dural arteriovenous fistulas with longterm persistent cortical venous reflux. Stroke. 2002; 33:1233–1236. PMID: 11988596.

5. Natarajan SK, Ghodke B, Kim LJ, Hallam DK, Britz GW, Sekhar LN. Multimodality treatment of intracranial dural arteriovenous fistulas in the onyx era: a single center experience. World Neurosurg. 2010; 73:365–379. PMID: 20849795.

6. Awad IA, Little JR, Akarawi WP, Ahl J. Intracranial dural arteriovenous malformations: factors predisposing to an aggressive neurological course. J Neurosurg. 1990; 72:839–850. PMID: 2140125.

7. Shi ZS, Loh Y, Duckwiler GR, Jahan R, Vinuela F. Balloon-assisted transarterial embolization of intracranial dural arteriovenous fistulas. J Neurosurg. 2009; 110:921–928. PMID: 19284242.

8. Fifi J, Niimi Y, Berenstein A. Onyx embolization of an extensive mandibular arteriovenous malformation via a dual lumen balloon catheter: a technical case report. J Neurointerv Surg. 2013; 5:e5. PMID: 22248630.

9. Newman CB, Hu YC, McDougall CG, Albuquerque FC. Balloon-assisted onyx embolization of cerebral single-channel pial arteriovenous fistulas. J Neurosurg Pediatr. 2011; 7:637–642. PMID: 21631202.

10. Spiotta AM, Sivapatham T, Teng Q, Moskowitz SI, Hui FK. Balloon-augmented carotid artery sacrifice with onyx: a proof of concept study in a swine model. J Neurointerv Surg. 2011; 3:390–394. PMID: 21990466.

Fig. 1
A. Brain atrophy and venous congestion was observed by MRI.
B. Transfemoral cerebral angiography showed the SSS DAVF was supplied via multiple branches of the external carotid artery (ECA), the right anterior cerebral arteries, and the meningeal branches of the internal carotid artery (ICA) and vertebral artery.
C. Drainage through the SSS was not observed, while drainage through the vein of Labbe and sphenoparietal sinus was main (not shown). Transfemoral cerebral angiography (TFCA) revealed venous hypertension and galenic venous drainage. Furthermore, TFCA showed CVR (The hallow indicates CVR).
D. Using the transvenous approach, a microcatheter (Echelon 10) was placed at the fistulous sac of the SSS.
E. After intravenous coil embolization using various coils, retrograde drainage through the fistula remained (arrow).
F. Scepter C balloon catheter (4×15 mm) was placed at the most distal segment of the middle meningeal artery. Tip of the balloon microcatheter was positioned at DAVF, and balloon was successfully performed (arrow).
G. Over a period of 22 minutes, a total of 4.5 cc of Onyx18 was injected, and DAVF was almost completely occluded.
H. After embolization, angiography revealed that no arteriovenous shunting and no cortical venous reflux occurred. Right ECA angiography.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download