Abstract
No fault compensation in perinatal medicine has been established to provide aid to patients in the event of disability due to a medical accident during delivery and to strive to resolve disputes quickly that contributes to reduce medical malpractice suit in the field of perinatal medicine. Furthermore, this system is aimed to establish a mechanism that achieves higher quality of obstetric care by analyzing the causes of accidents. This system is operated by Japan Council for Quality Health Care and 99.9% of childbirth facilities in Japan registered with this compensation system. Compensation system has two major functions including compensation and cause analysis and recurrence prevention based on cases. Compensation eligibility is reviewed in the Review Committee at the organization in Japan Council for Quality Health Care and currently 1,717 cases are judged as eligible cases out of 2,250 since 2009. The cause of each eligible case is analyzed in the Cause Analysis Committee one by one. The Cause Analysis Committee has 7 independent subcommittee and each subcommittee members are consistent of obstetricians, neonatologists, pediatricians, midwives and lawyers. Original cause analysis report is sent to childbirth facility and patient's family. Questionnaire survey demonstrated that 73% of childbirth facilities and 65% of patient family were satisfied with the cause analysis report. The number of medical lawsuit in obstetrics and gynecology is significantly decreased compared to those in all medical departments since the compensation system was introduced suggesting that these cause analysis reports may contribute the decrease in medical lawsuits. The major purpose of the Recurrence Prevention Committee is striving to prevent future cases of cerebral palsy and to improve the quality of obstetric care. To accomplish the purpose, the committee routinely collect information from individual cases and analyze quantitatively and epidemiologically. Furthermore the committee choose subject from cases to discuss for future prevention and provide wide public disclosure of the information with recommendation. The committee issued 6 reports until now and these reports have been distributed to childbirth facilities, perinatal medicine-related scientific society and administrative agencies.
No fault compensation in perinatal medicine has been established to provide aid to patients in the event of disability due to a medical accident during delivery and to strive to resolve disputes quickly that contributes to reduce medical malpractice suit in the field of perinatal medicine. Furthermore, this system is aimed to establish a mechanism that achieves higher quality of obstetric care by analyzing the causes of accidents. In this review article, function and activities of compensation system for 8 years since establishment of this system are introduced.
There were many medical low suits in the field of department of obstetrics and gynecology that were protrudently frequent among other clinical departments and the majority cases were medical accident related to childbirth (Fig. 1). This has been one of cause of further reduction of the obstetrician. On the other hand, the winning rate of medical low suits in patient side has been decreasing year after year and the rate was approximately 20% at 2010 suggesting that majority of patients have to pay legal fee without compensation. Under these situation, compensation system was established.
Formal name of this compensation system is “the Japan Obstetric Compensation System for Cerebral Palsy” that is organized by Japan Council for Quality Health Care (JQ). Major function of the system are compensation and in-depth cause analysis and future prevention. Eligibility of compensation of each case is judged in the Review Committee in JQ and cause analysis and recurrence prevention is in charge in the Cause Analysis Committee and the Recurrence Prevention Committee, respectively. Through these activities, compensation system is intended to achieve four major purposes including providing aid to patients in the event of disability due to a medical accident during delivery, striving to resolve disputes quickly, establishing a mechanism that achieves higher quality of obstetric care by analyzing the causes of accidents and preventing the shortage in obstetricians by reducing malpractice suit.
Compensation is carried out by quickly providing compensation for the economic burden of the child and family in the event of delivery-related cerebral palsy to aid prevent disputes and/or early resolution. Compensation agreement is carried out between pregnant woman/her family and childbirth facility enrolled in compensation system in JQ. Almost all childbirth facilities enrolled in compensation system except 3 private clinics (Table 1). Each childbirth facility pays 24,000 yen to JQ for insurance premium and JQ signs a contract with the insurance company, and if the case is judged as eligible by JQ, the compensation money is paid from the indemnity insurance firm to the mother (Fig. 2). Japan has a policy of universal health insurance coverage. When someone gets pregnant and gives birth to a baby, the health care insurer of the mother pays lump-sum allowance of 420,000 yen to her.
The insurance premium of 24,000 yen per delivery is included in this lump-sum allowance. The payment and the amount of allowance are stipulated in the Health Insurance Law. The mother pays delivery fee including insurance premium to the childbirth facility, and the insurance premium is collected at JQ from the delivery facility and managed in the contracted indemnity insurance firm. Eligibility criteria for compensation that was revised in 2015 is infants with cerebral palsy related to brain injuries during delivery who were born after 32 gestational weeks with birth weight more than 1,400 grams. In addition, degree of severity should be certified as 1st or 2nd degree of severity according to the Japanese Social Welfare System. Infants with cerebral palsy delivered between 28 and 32 gestational weeks may be compensated on a “case-by-case review” based on the evidence of hypoxic conditions. When cerebral palsy is determined not to be caused by obstetric adverse events such as congenital or neonatal causes, the case is excluded from compensation. Number of reviewed cases by July, 2016 was more than 2,000, of which 1,717 cases were judged as eligible and 465 cases were judged as not eligible (Table 2).
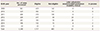
Total 30 million yen will be paid in each case in which 6 million yen is paid as “lump-sum” for expenses to build such a platform as housing renovation to raise a disabled child, purchasing assistive products, and paid 24 million yen (1.2 million yen per year for 20 times) as “installment” for expenses to provide nursing care. Among 1,501 eligible cases, only 63 cases (4.2%) claimed damage among which only 34 cases filed a lawsuit and the rest 29 cases preferred “out-of-court” settlement suggesting that compensation system is contributed to reducing medical lawsuits.
The cause of each eligible case is analyzed in the Cause Analysis Committee one by one. The Cause Analysis Committee has 7 independent subcommittee and each subcommittee is consistent of 14 members including nine obstetricians, one neonatologists, one pediatricians, one midwives and two lawyers. The basic attitude of the cause analysis is as follows. (1) The purpose of the cause analysis is not to look for someone to blame, but to identify the causes why it happened from an exclusively medical point of view. At the same time, the cause analysis is meant to provide suggestions that may contribute to prevention of future similar cases. (2) The cause analysis report should be written to be understandable and reliable for children and their families, citizens, and lawyers, etc. (3) The cause analysis explores possible causes after knowing the fact that cerebral palsy was developed (retrospective analysis), taking into account of clinical conditions during delivery, in past history, during pregnancy, and in neonatal period. (4) For medical evaluation of clinical course in the cause analysis, adequacy of medical procedures or treatment is analyzed only in the given conditions at the point of each intervention (prospective analysis), without taking account of events or results occurred afterwards including development of cerebral palsy.
Report draft that was created in each subcommittee based on medical records, midwife records, examination data, and information from the child/family is further shaped up at the entire committee to create the formal report. Contents of cause analysis report consist of summary of clinical course, cause(s) of cerebral palsy, medical evaluation of clinical course and suggestion for improvement. Summary of the causal analysis report is posted on the homepage of JQ and original report is sent to both the childbirth facility and the patient's family. Furthermore, the masked version is provides only to the researchers whose research is considered appropriate by the ethics committee in JQ.
Questionnaire survey demonstrated that 73% of childbirth facilities and 65% of patient family were satisfied with the cause analysis report. Out of 796 cases on which cause analysis reports were compiled, only 20 cases (2.5%) claimed damage after the day when the report was delivered and out of 20 cases above, 9 cases filed a lawsuit and the rest 11 cases preferred “out-of-court” settlement. The number of medical lawsuit in the department of obstetrics and gynecology is significantly decreased compared to those in all medical departments since the compensation system was introduced (Fig. 3) suggesting that these cause analysis reports may contribute the decrease in medical lawsuits as well as monetary compensation.
The major purpose of the Recurrence Prevention Committee is striving to prevent future cases of cerebral palsy and to improve the quality and enhance public confidence in obstetric care. To accomplish these purpose, the committee routinely collect information from individual cases based on reports from the Cause Analysis Committee and analyze quantitatively and epidemiologically [1]. Furthermore the committee choose subject from cases to discuss for future prevention and provide wide public disclosure of the information with recommendation. The relationship between the Cause Analysis Committee and the Prevention of Recurrence Committee is shown in Fig. 4. Contents of prevention of recurrence report consist of epidemiological and quantitative analysis and qualitative analysis on specific theme. In epidemiological and quantitative analysis, basic element of individual case such as current physical status and past history of pregnant woman, history of current pregnancy, progress and procedures of delivery and neonatal care and institutional resources prerequisite for childbirth care are collectively tabulated and presented.
In qualitative analysis on specific theme, individual theme which deserves further research is focused and the result of research including preventive measure is presented. At present, seven theme were selected in the report including neonatal resuscitation, fetal heart rate monitoring during delivery, administration of uterine contraction agent, management of umbilical prolapse, vacuum-assisted delivery, prophylactic maternal education on placental abruption, and medical recording worth to be on expert analysis as specific theme.
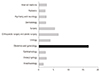
The committee issued 6 reports until now and these reports have been distributed to childbirth facilities, perinatal medicine-related scientific society and administrative agencies. In questionnaire survey, 72% of childbirth facilities have been using the recurrence prevention report for the quality improvement of obstetric care. Other than regular report, the committee has been publishing leaflet of educational statement to medical professionals in childbirth facilities, various alerting brochures and educational materials for cardiotocography learning and distributing to childbirth facilities, relevant academic societies and organizations (Fig. 5).
It is certain that the compensation system are contributing not only to reducing medical lawsuits in the department of obstetrics and gynecology but also contributing to establishing higher quality of perinatal medicine through above broad activities. Furthermore, it is noteworthy that the compensation system also serves as an educational system with built-in reportedly world largest database of medical recording or data of cerebral palsy. Accumulated data of cerebral palsy cases in this compensation system are considered a great help to the improvement of obstetric care.
Figures and Tables
Fig. 2
Outline of compensation system. JPY, Japan yen; KRW, Korean won; JQ, Japan Council for Quality Health Care.

Fig. 3
Number of lawsuit in department of obstetrics and gynecology and whole medical department (statistics of the committee on lawsuit related to health care, the supreme court of Japan).
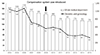
Fig. 5
Publications by recurrence prevention committee. (A) Recurrence Prevention Report, (B) brochure for recurrence prevention, and (C) analytical book cardiotocography of cerebral palsy cases. Available from: http://www.sanka-hp.jcqhc.or.jp/documents/prevention/index.html.

Table 1
Registration of childbirth facilities (as of July 2016)
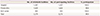
| No. of childbirth facilities | No. of participating facilities | % participation | |
|---|---|---|---|
| Hospital | 1,207 | 1,207 | 100.0 |
| Private clinic | 1,629 | 1,626 | 99.8 |
| Birth center | 443 | 443 | 100.0 |
| Total | 3,279 | 3,276 | 99.9 |
Table 2
Profile of reviewed cases (January 2009 to July 2016)




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download