Abstract
Objective
To report the various anatomic locations of surgically and pathologically proven endometriosis.
Methods
Pathologic reports (n=1,376) of women who underwent surgeries at a single center between April 2005 and March 2013 were retrieved from the electronic medical record system of the hospital. Pathologic reports were included after performing a search by using the key-words "endometrial cyst," "endometriotic cyst," "endometriosis," or "endometrioma." Only reports dealing with female patients were selected, and the pathologic reports of 1,350 women (1,374 surgery cases) were included in the analysis.
Results
The predominant location of endometriosis was the ovaries (96.4%), followed by the soft tissue (2.8%), gastrointestinal tract (0.3%) and urinary tract (0.2%). Laparoscopic surgery was the major surgical technique used for the pelvic endometriosis (89.2%). Adrenal gland endometriosis was found in a 55-year-old woman.
Endometriosis is a common gynecologic condition occurring in 10% to 15% of women of reproductive age and is associated with decreased fecundity [1]. The common sites of endometriosis are the ovaries, fallopian tubes, pelvic peritoneum, and uterosacral ligaments (USL) (alternatively called the "pelvic" site), whereas the atypical sites of endometriosis include the gastrointestinal tract, urinary tract, soft tissues, and chest (alternatively called the "extra-pelvic" site) [2]. Endometriosis lesions can be classified as ovarian, exclusively extra-ovarian or mixed.
Diagnosis of extra-pelvic endometriosis can be difficult. Depending on the involved site, women can present with various symptoms including bowel obstruction, melena, hematuria, dysuria, dyspnea, and swelling in soft tissues [2]. Precise diagnosis regarding the presence, location, and extent of endometriosis may be useful for the preoperative evaluation of and surgical planning for endometriosis. Since clinical information is essential for proper therapeutic management with complex surgeries, the anatomic distribution of lesions should be accurately examined.
This study presents our experience with different anatomic locations of endometriosis. Herein, we report the various anatomic locations of surgically and pathologically proven endometriosis in 1,350 women (1,374 surgery cases and 1,376 pathologic reports) presenting at a single center.
We retrieved the reports of 1,350 women who underwent 1,374 surgeries (1,376 pathologic reports) at the Seoul National University Bundang Hospital between April 2005 and March 2013. The pathologic reports were retrieved from the electronic medical record system of the hospital, and the searches were conducted using the key-words "endometrial cyst," "endometriotic cyst," "endometriosis," or "endometrioma." Only reports dealing with female patients were included in the analysis. Twenty-four women underwent repeated surgeries owing to the recurrence of endometriosis. Two women underwent two surgeries concurrently (e.g., appendectomy and ovarian surgery), which resulted in the addition of two pathologic reports to the analysis. The institutional review board of our hospital approved the use of the patients' medical records.
The anatomic distribution of endometriosis was investigated using the operative records. Clinico-pathologic variables including patient age, type of surgery, bilaterality of endometriosis (in the case of ovarian endometriosis), and symptoms (dysmenorrhea, chronic pelvic pain, deep dyspareunia, and dyschezia) were analyzed. Endometriosis was staged and scored according to the revised American Society for Reproductive Medicine classification. Cul-de-sac obliteration was defined as complete or partial adhesion, according to the surgical reports. Endometriotic lesions were classified as pelvic (with or without cul-de-sac obliteration), gastrointestinal, urinary, soft tissue, or other. SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis, and a value of P<0.05 was considered statistically significant.
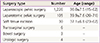
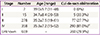
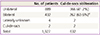
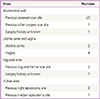
The mean age of the women was 36.3±7.5 years (range, 15 to 71 years). Laparoscopic surgery was the main surgical technique for pelvic endometriosis (89.2%, 1,226/1,374) (Table 1). According to the pathological reports, ovarian endometrioma was the predominant form of endometriosis (96.4%), followed by soft tissue endometriosis (2.8%), gastrointestinal endometriosis (0.3%), and urinary tract endometriosis (0.2%) (Table 2). The mean age of women was similar between those with stage III and those with stage IV endometriosis, but cul-de-sac obliteration was more prevalent in stage IV endometriosis patients (Table 3). Unilateral ovarian involvement was more common than bilateral ovarian involvement (Table 4). Cul-de-sac obliteration was more prevalent in patients with bilateral endometrioma.
Thirty-nine cases of pathologically proven endometriosis occurred in soft tissue (Table 5). The majority of the lesions were located near a previous operation scar. The most common site of soft tissue endometriosis was the abdominal wall, which was associated with a previous Cesarean section. Three women presented with vulvar endometriosis, and all of them had a history of vaginal birth. Three patients presented with inguinal endometriosis, and in 2 of the patients, endometriosis was associated with a previous hernia operation scar.
Three patients presented with appendiceal endometriosis, which was detected during appendectomy; in 1 patient, acute appendicitis was the presumptive diagnosis before surgery. In the other 2 women, appendiceal endometriosis was incidentally found during open gynecologic surgery.
Rectal endometriosis was found in a 36-year-old woman (parity 2-0-0-2). She complained of severe dysmenorrhea. During laparoscopic surgery, low anterior resection with lymphatic dissection was performed owing to severe colonic obstruction 10 cm from the anal verge. The pathologic report showed that multifocal endometriotic lesions extended from the muscularis propria to the mucosa. Interestingly, endometriosis affected 4 out of 45 lymph nodes (pericolic, 4/39; inferior mesenteric artery root, 0/6). The patient had a history of open gynecologic surgery at 19 years of age for a uterine mass of unknown origin.
Bladder endometriosis was found in 2 women. One woman (43 years old, parity 2-0-0-2, and prior vaginal delivery) experienced cyclic abdominal pain, and a protruding mass was detected in the inner bladder. This patient underwent transurethral resection of the mass. In the other woman (41 years old, parity 2-0-0-2, and prior cesarean delivery), a bladder wall mass was incidentally detected by using computed tomography (CT). This patient also underwent trans-urethral resection of the bladder wall mass, and endometriosis was diagnosed pathologically. The patient had a history of hysterectomy for ovarian endometriosis.
Ureter endometriosis was found in 1 patient (42 years old, parity 1-0-0-1, and prior vaginal delivery). In this case, recurrent hydronephrosis developed and a ureteral polyp and endometriosis were detected via ureteroscopy. Transvaginal ultrasonography showed no abnormal findings in both adnexa.
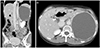
Adrenal gland endometriosis, which is extremely rare, was found in a 55-year-old woman. This patient experiended left upper quadrant abdominal discomfort; an approximately 13-cm hemorrhagic cyst in the left abdominal cavity was observed on a CT scan (Fig. 1). Laparotomic adrenalectomy was performed, and endometriosis was pathologically confirmed. The patient had a history of laparoscopic cholecystectomy performed 2 years ago.
As outlined in our literature review, several studies have reported the anatomical distribution of deeply infiltrating endometriosis (DIE), which is responsible for painful symptoms such as dysmenorrhea, chronic pelvic pain, deep dyspareunia, and dyschezia [3,4]. Dai et al. [4] analyzed 177 cases of laparoscopically proven DIE, which was located in the USL (67.1%), rectovaginal septum (12.7%), cul-de-sac (12.0%), ureter (3.8%), rectum and recto-sigmoid junction (2.8%), or bladder (1.6%); 60.7% of the nodules on the USL were bilateral, and 44.6% of the cul-de-sac were completely blocked. Another study analyzed the medical, operative and pathological reports of 241 consecutive patients with histologically proven DIE in order to investigate the anatomical distributions of DIE [3]. In that study, the most common site for endometriotic lesions was the USL (69.2%), followed by the vagina (14.5%), bladder (6.4%), and intestines (9.9%).
We found that the majority of the endometriotic lesions (96.4%) occurred in the pelvic cavity, which is consistent with the results of previous study [2]. Complete obliteration of the pouch of Douglas was found in 47.6% of the patients in a previous study. This incidence rate is consistent with that reported by other study [5].
Interestingly, in our study, soft tissue was the second most common site of endometriosis (2.8%), which is more common than that reported in other studies. In our study, abdominal wall endometriosis was relatively predominant in women with soft tissue endometriosis (51.9%, 27/52). In almost all cases, the endometriotic lesions were located at the site of previous operation scar from a Cesarean section or hysterectomy. Scar site endometriosis has been reported to occur in approximately 0.03% to 0.4% of women undergoing caesarean section [6]. A previous study reported the occurrence of endometriosis at the site of a previous operation scar in Korean women [7]. Fifteen of 30 women with extra-pelvic endometriosis showed endometriotic lesions at the site of a previous cesarean scar. The mean age (37.1 years) of the women with abdominal wall endometriosis in our study was quite higher than that reported by a previous study (32.3 years) [8]. Previous studies have reported that the patients usually present with a palpable erythematous skin nodule or mass associated with an incision scar and experience intermittent excruciating pain, tenderness, and enlargement of the mass during menstruation [2,9,10,11].
Three women presented with vulvar endometriosis, and all of them had a history of vaginal birth. This finding suggests that vulvar endometriosis can occur in a previous episiotomy site. Four patients presented with isolated vaginal endometriosis. However, it is unknown whether pelvic endometriosis coexisted in these patients because they did not undergo laparoscopic inspection. In a study, the proportion of isolated lesions in patients with vaginal DIE was 56.0%; this indicates that multifocal lesions simultaneously involving the USL, bladder, or intestine could exist in 44% of the patients with vaginal DIE [3]. In cases of vaginal DIE, dissection of the laterorectal fossae and exeresis of the upper part of the posterior vaginal wall are recommended because lesions developing in those areas commonly co-exist with vaginal DIE [12].
We found gastrointestinal endometriosis in 0.3% and urinary tract endometriosis in 0.2% of the patients; these rates are fairly lower than those reported in other studies [2]. Woodward et al. [13] reported that the recto-sigmoid colon is the most common gastrointestinal site for endometrial deposits (70% to 85%). This is followed by the terminal ileum (1% to 7%), appendix, cecum, and the rest of the small bowel. Terminal ileal involvement usually occurs within 10 cm of the ileocecal valve, and it can be observed even in the absence of recto-sigmoid implants [13]. Chapron et al. [3] also reported that the most common site for intestinal DIE is the rectum (58.9%), followed by the sigmoid colon (20.6%), colon (8.8%), ileocecum or terminal ileum (5.9%) and appendix (2.9%). We were unable to determine the specific site of intestinal DIE. Endometrial implants can be located along the anti-mesenteric border of the bowel wall, and growth occurs from the serosa inwards [3].
In the present study, bladder endometriosis was found in only 2 women. A previous literature review analysis showed that endometriosis involved the urinary tract in up to 20% of the cases [14]. In these cases, involvement of the urinary bladder was the most common, followed by involvement of the lower ureter. Urinary bladder implants commonly occur on the serosal surface near the dome; they can progressively invade the muscularis propria and protrude in the lumen as intramural or intraluminal masses [15]. Urinary tract endometriosis may arise from pre-existing foci of peritoneal endometriosis covering the bladder or from direct extension of an adenomyotic nodule, or it may develop from embryonic remnants [2,16,17,18,19]. In a study, the main symptom of bladder endometriosis was urinary frequency [20]. It was reported that 20% to 30% of the affected women presented with menstrual hematuria [21].
The most intriguing case of endometriosis in our study was that of a patient with adrenal gland endometriosis. Only 1 such case has been reported previously (reported in 2008) [22]. In that study, a 48-year-old woman experienced left flank pain, which is similarly to that observed in our case. The pain was intermittent and worsened with menstruation. A CT scan showed a 10-cm mass in the left upper quadrant of the abdomen, which is also similar to that observed in our case. The patient's medical history was unremarkable, except for an emergency cesarean section at 26 years of age. She was treated with laparoscopic adrenalectomy and pathologically diagnosed with endometriosis. Adrenal gland endometriosis is an extremely rare condition, and we believe that our case is the second reported case of this condition worldwide.
Endometriosis in extra-pelvic sites may result from vascular or lymphatic dissemination of endometrial cells to several gynecologic (vulva, vagina, or cervix) and non-gynecologic sites (bowel, appendix, hernia sacs, lungs, skin, or nerves). Because endometriosis could involve any system of the body, one of the major challenges in diagnosing women with suspected endometriosis is to assess the extent of the disease and its functional consequences for the pelvic or extra-pelvic organs. Many researchers have suggested classifications of endometriosis, but no validated system meets the clinical needs yet.
In our study, the incidence of extra-pelvic endometriosis was 3.4%. Although rare, soft tissue endometriosis showed a relatively high incidence rate in our study and was associated with previous surgical sites. Therefore, endometriosis should be considered when cutaneous nodules develop near surgical scars in women with cyclic soft tissue pain.
To our knowledge, our study is the first to report the various anatomic locations of surgically and pathologically proven endometriosis in Korean women. Although this study describes a single-center experience, it includes a larger sample size of women than has been reported previously. The most common site of endometriosis was the pelvic cavity, followed by soft tissues; this feature is slightly different from the results by the other studies.
Figures and Tables
Fig. 1
Representative computed tomography images showing an approximately 13-cm hemorrhagic cyst, which was proven to be an endometrioma, arising in the adrenal gland in a 55-year-old woman. (A) Coronal view and (B) axial view.
Acknowledgments
This work was supported by grant (no. A120043) from the Korea Health Care Technology R&D Project, Ministry of Health and Welfare, Korea.
References
1. Dmowski WP, Lesniewicz R, Rana N, Pepping P, Noursalehi M. Changing trends in the diagnosis of endometriosis: a comparative study of women with pelvic endometriosis presenting with chronic pelvic pain or infertility. Fertil Steril. 1997; 67:238–243.
2. Sonavane SK, Kantawala KP, Menias CO. Beyond the boundaries-endometriosis: typical and atypical locations. Curr Probl Diagn Radiol. 2011; 40:219–232.
3. Chapron C, Fauconnier A, Vieira M, Barakat H, Dousset B, Pansini V, et al. Anatomical distribution of deeply infiltrating endometriosis: surgical implications and proposition for a classification. Hum Reprod. 2003; 18:157–161.
4. Dai Y, Leng JH, Lang JH, Li XY, Zhang JJ. Anatomical distribution of pelvic deep infiltrating endometriosis and its relationship with pain symptoms. Chin Med J (Engl). 2012; 125:209–213.
5. Redwine DB, Wright JT. Laparoscopic treatment of complete obliteration of the cul-de-sac associated with endometriosis: long-term follow-up of en bloc resection. Fertil Steril. 2001; 76:358–365.
6. Singh KK, Lessells AM, Adam DJ, Jordan C, Miles WF, Macintyre IM, et al. Presentation of endometriosis to general surgeons: a 10-year experience. Br J Surg. 1995; 82:1349–1351.
7. Lee SE, Jeong JE, Joo JK, Lee KS. Clinicopathologic review of extrapelvic endometriosis. Korean J Obstet Gynecol. 2012; 55:83–88.
8. Bektas H, Bilsel Y, Sari YS, Ersoz F, Koc O, Deniz M, et al. Abdominal wall endometrioma: a 10-year experience and brief review of the literature. J Surg Res. 2010; 164:e77–e81.
9. Samal AG, Behera PK, Sahoo P. Abdominal scar endometriosis. Indian J Surg. 2013; 75:Suppl 1. 217–219.
10. Ecker AM, Donnellan NM, Shepherd JP, Lee TT. Abdominal wall endometriosis: 12 years of experience at a large academic institution. Am J Obstet Gynecol. 2014; 211:363.
11. Heller DS, Fitzhugh VA. Abdominal wall endometriosis: a rarely anticipated diagnosis: a 16-year experience and brief literature review. J Reprod Med. 2014; 59:110–112.
12. Chapron C, Jacob S, Dubuisson JB, Vieira M, Liaras E, Fauconnier A. Laparoscopically assisted vaginal management of deep endometriosis infiltrating the rectovaginal septum. Acta Obstet Gynecol Scand. 2001; 80:349–354.
13. Woodward PJ, Sohaey R, Mezzetti TP Jr. Endometriosis: radiologic-pathologic correlation. Radiographics. 2001; 21:193–216.
14. Markham SM, Carpenter SE, Rock JA. Extrapelvic endometriosis. Obstet Gynecol Clin North Am. 1989; 16:193–219.
15. Choudhary S, Fasih N, Papadatos D, Surabhi VR. Unusual imaging appearances of endometriosis. AJR Am J Roentgenol. 2009; 192:1632–1644.
16. Chapron C, Boucher E, Fauconnier A, Vieira M, Dubuisson JB, Vacher-Lavenu MC. Anatomopathological lesions of bladder endometriosis are heterogeneous. Fertil Steril. 2002; 78:740–742.
17. Donnez J, Spada F, Squifflet J, Nisolle M. Bladder endometriosis must be considered as bladder adenomyosis. Fertil Steril. 2000; 74:1175–1181.
18. Somigliana E, Vercellini P, Gattei U, Chopin N, Chiodo I, Chapron C. Bladder endometriosis: getting closer and closer to the unifying metastatic hypothesis. Fertil Steril. 2007; 87:1287–1290.
19. Vercellini P, Frontino G, Pisacreta A, De Giorgi O, Cattaneo M, Crosignani PG. The pathogenesis of bladder detrusor endometriosis. Am J Obstet Gynecol. 2002; 187:538–542.
20. Kjer JJ, Kristensen J, Hartwell D, Jensen MA. Full-thickness endometriosis of the bladder: report of 31 cases. Eur J Obstet Gynecol Reprod Biol. 2014; 176:31–33.
21. Schneider A, Touloupidis S, Papatsoris AG, Triantafyllidis A, Kollias A, Schweppe KW. Endometriosis of the urinary tract in women of reproductive age. Int J Urol. 2006; 13:902–904.
22. Rehman J, Yildirim G, Khan SA, Chughtai B, Nezhat F. A case of successful laparoscopic resection of adrenal gland endometriosis. Fertil Steril. 2008; 90:2015.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download