Abstract
Purpose
This study was to identify factors influencing burden among family caregivers of elderly cancer patients.
Methods
The participants were 217 family caregivers who visited inpatient & outpatient clinics for elderly cancer patients at two general hospitals. Data were collected utilizing the Perceived Health Status Scale, Herth Hope Index Scale, Medical Outcome Study-Social Support Scale, and Caregiver Reaction Assessment Scale.
Results
The level of burden in the participants was moderate to high. There were significant correlations among perceived health status, hope, social support and burden. In multiple regression analyses, the most powerful predictor of burden in family caregivers was hope (36.0%). Overall, other caregivers, perceived economic status, caring time, gender, patients' confusion, tangible support, and perceived health status explained 61.0% of the variance of burden among the participants.
Figures and Tables
Table 1
Burden of Family Caregivers by General Characteristics (N=217)

Table 2
Burden of Family Caregivers by General Characteristics of Patients (N=217)

Table 3
cores of Perceived Health Status, Hope, Social Support and Burden (N=217)
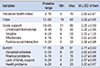
Table 4
Correlations among Perceived Health Status, Hope, Social Support and Burden (N=217)
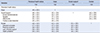
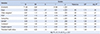
Table 5
Factors Influencing Burden among Family Caregivers (N=217)
References
1. Korean Statistical Information Service. Accessed September 1, 2015. http://kosis.kr/wnsearch/total-Search.jsp.
2. Hsu T, Loscalzo M, Ramani R, Forman S, Popplewell L, Clark K, et al. Factors associated with high burden in caregivers of older adults with cancer. Cancer. 2014; 120(18):2927–2935.

3. Loerzel WV. Symptom experience in older adults undergoing treatment for cancer. Oncol Nurs Forum. 2015; 42(3):E269–E278.
4. Kim NS. A Study of woman's caring as a phenomena of gender [dissertation]. Seoul: Ewha Womans Univ.;1993.
5. Rha SY, Park YH, Song SK, Lee CE, Lee JY. Caregiving burden and the quality of life of family caregivers of cancer patients: the relationship and correlates. Eur J Oncol Nurs. 2015; 19(4):376–382.

6. Utne I, Miaskowski C, Paul SM, Rustoen T. Association between hope and burden reported by family caregivers of patients with advanced cancer. Support Care Cancer. 2013; 21(9):2527–2535.

7. Govina O, Kotronoulas G, Mystakidou K, Katsaragakis S, Vlachou E, Patiraki E. Effects of patient and personal demographic, clinical and psychosocial characteristics on the burden of family members caring for patients with advanced cancer in Greece. Eur J Oncol Nurs. 2015; 19(1):81–88.

8. Yoon SJ, Kim JS, Jung JG, Kim SS, Kim SY. Modifiable factors associated with caregiver burden among family caregivers of terminally ill Korean cancer patients. Support Care Cancer. 2014; 22(5):1243–1250.

9. Shieh SC, Tung HS, Liang SY. Social support as influencing primary family caregiver burden in Taiwanese patients with colorectal cancer. J Nurs Scholarsh. 2012; 44(3):223–231.

10. Hong MJ, Tae YS, Noh MY. Relationships between stress, ways of coping and burnout of family caregivers of cancer patients. Asian Oncol Nurs. 2012; 12(1):92–99.

11. Thomas K, Hudson P, Oldham L, Kelly B, Trauer T. Meeting the needs of family carers: an evaluation of three home-based palliative care services in Australia. Palliat Med. 2010; 24(2):183–191.

12. Lee YS. A study of effect on quality of life of cancer patient's caregiver : focusing on the mediating effect of feeling of burden and growth. Korean J Soc Welf. 2009; 61(2):325–348.
13. Woo YJ. Caregiver burden, coping and quality of life according to gender among spouses of cancer patients undergoing chemotherapy [master's thesis]. Seoul: Seoul National Univ.;2015.
14. Park MY. The relationship between burden, spiritual well-being, and quality of life in family of terminal cancer inpatients in Korea hospice palliative care institutions [master's thesis]. Busan: Kosin Univ.;2015.
15. Lohne V, Miaskowski C, Rustoen T. The relationship between hope and caregiver strain in family caregivers of patients with advanced cancer. Cancer Nurs. 2012; 35(2):99–105.

16. Duggleby W, Bally J, Cooper D, Doell H, Thomas R. Engaging hope: the experiences of male spouses of woman with breast cancer. Oncol Nurs Forum. 2012; 39(4):400–406.

17. Kim SY, Kim JM, Kim SW, Kang HJ, Shin IS, Shim HJ, et al. Determinants of a hopeful attitude among family caregivers in a palliative care setting. Gen Hosp Psychiatry. 2014; 36(2):165–171.

18. Hong MJ. Structural relationships between burnout and related variables among family caregivers of cancer patients [dissertation]. Busan: Kosin Univ.;2013.
19. Lee HJ, Lee JW, Lee JY. Family caregiver's burden for elderly with dementia: moderating effects of social support. J Soc Sci. 2015; 26(1):345–367.

20. Taylor SE. Health Psychology. New York: McGraw Hill.;2012.
21. Speake DL, Cowart ME, Pellet K. Health perceptions and lifestyles of the elderly. Res Nurs Health. 1989; 12(2):93–100.

23. Kim YO. Effects of home care services on discomfort in patients with cancer and on caregiver burden [master's thesis]. Seoul: Yonsei Univ.;2002.
24. Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health. 1992; 15(4):271–283.

25. Hwang MH. Structural model of the elderly self-care and well-being [dissertation]. Daegu: Kyungpook National Univ;2000.
26. Herth K. Hope in the family caregiver of terminally ill people. J Adv Nurs. 1993; 18(4):538–548.

27. Youn SJ. The effects of forgiveness nursing intervention program on forgiveness and mental health in patients with advanced women cancer [dissertation]. Busan: Kosin Univ.;2005.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download