Abstract
Purpose
The International Organization for Standardization-5fluorouracil (FU) 10 trial found that bolus 5-FU and l-leucovorin was not inferior to S-1 in the treatment of gastric cancer (GC). Continuous 5-FU and the rapid injection of 5-FU have different anti-cancer effects. Thus, bolus 5-FU and l-leucovorin treatment might be useful for oral FU-resistant GC.
Materials and Methods
We retrospectively analyzed the medical records of all patients with S-1 or capecitabine-resistant, unresectable, or recurrent GC treated with bolus 5-FU and l-leucovorin between January 2010 and December 2015 at Hokkaido University Hospital. The bolus 5-FU and l-leucovorin regimen consisted of intravenous l-leucovorin (250 mg/m2/2 h) and bolus 5-FU (600 mg/m2) administered once weekly followed by a 2-week rest period; each cycle was repeated every 8 weeks.
Results
A total of 14 patients were identified. The disease control rate was 35.7%. The median progression-free survival was 1.6 months (95% confidence interval [CI], 1.3~2.0 months), and the median overall survival was 6.3 months (95% CI, 4.7~7.9 months). No patient died from treatment-related causes. The most common severe adverse event associated with bolus 5-FU and l-leucovorin was neutropenia, which occurred in 21.4% of patients.
Conclusions
Bolus 5-FU and l-leucovorin treatment might be useful for oral FU-resistant GC. We are planning a multi-center prospective phase II trial to evaluate the efficacy and safety of bolus 5-FU and l-leucovorin treatment for pre-treated unresectable or recurrent GC to confirm the results of this limited, retrospective study.
In Japan, the prevalence of gastric cancer (GC), the second most common malignancy nationwide, has continued to increase each year, and there were 125,730 active cases and 16,654 cases deaths in 2010. The SPIRITS trial1 showed that progression-free survival (PFS) and overall survival (OS) of patients treated with S-1+cisplatin combination therapy were significantly superior to those treated with S-1 monotherapy; thus, S-1+cisplatin combination therapy was established as the standard primary chemotherapy for unresectable or recurrent GC in Japan.
However, the REAL-22 and G-SOX3 studies found that oxaliplatin was non-inferior to cisplatin, and it can replace cisplatin for GC treatment. In addition, the ToGA trial45 reported that the addition of trastuzumab to 5-fluorouracil (FU)+cisplatin or capecitabine+cisplatin improved the OS of patients with GC that overexpressed human epidermal growth factor receptor 2, whereas the RAINBOW67 and REGARD8 trials demonstrated that ramucirumab, which is a humanized antibody against vascular endothelial growth factor, prolonged the OS of patients with GC who were treated both with and without paclitaxel. After the development of resistance to first-line chemotherapy, docetaxel or irinotecan as second-line chemotherapy can prolong OS as compared with best supportive care alone.9 However, there is a non-negligible number of patients with GC resistant to all of these chemotherapy regimens who require further chemotherapy.
The International Organization for Standardization-5FU10 study10 reported that the efficacy of weekly bolus 5-FU and l-leucovorin therapy was not inferior to that of S-1 monotherapy, which was the standard first-line chemotherapy for unresectable advanced GC in Japan during that time. There are two known mechanisms underlying the anti-cancer effects of 5-FU.1112 One is the inhibition of DNA synthesis through the inhibition of thymidylate synthase activity by fluorodeoxyuridine-5'-monophosphate, a metabolite of 5-FU, and the second is inhibition of RNA dysfunction by 5-fluorouridine triphosphate, another metabolite of 5-FU. Because inhibition of DNA synthesis by 5-FU is mainly time-dependent, continuous infusion of 5-FU or daily administration of oral fluoropyrimidine drugs, such as S-1 and capecitabine, has an anti-tumor effect. However, the anti-tumor effect caused by RNA dysfunction after rapid injection of 5-FU is concentration-dependent. Thus, bolus 5-FU and l-leucovorin therapy is expected to be effective against oral fluoropyrimidine-resistant GC.
The national health insurance program of Japan covers bolus 5-FU and l-leucovorin therapy for treatment of GC. The aim of this study was to retrospectively assess the efficacy of bolus 5-FU and l-leucovorin therapy for oral fluoropyrimidine-resistant unresectable GC.
We retrospectively analyzed the medical records of all patients with unresectable or recurrent GC and enrolled patients treated with bolus 5-FU and l-leucovorin after failure of S-1 or capecitabine between January 2010 and December 2015 at Hokkaido University Hospital.
This study was a retrospective cohort single-center analysis to evaluate the efficacy and safety of bolus 5-FU and l-leucovorin against oral fluoropyrimidine-resistant unresectable GC. The study protocol was approved by the Institutional Review Board of Hokkaido University Hospital and conducted in accordance with the tenants of the Declaration of Helsinki.
The bolus 5-FU and l-leucovorin regimen consisted of intravenous l-leucovorin (250 mg/m2/2 h) and bolus 5-FU (600 mg/m2) once weekly followed by a 2-week rest period along with best supportive care. Treatment cycles were repeated every 8 weeks until tumor progression or intolerable toxicity occurred.
PFS was calculated from the first day of treatment to the time of disease progression or last follow-up. OS was calculated from the first day of the treatment to the time of death or last follow-up. OS and PFS were calculated using the Kaplan-Meier method. Statistical analyses were performed using IBM SPSS Statistics ver. 23 (IBM Co., Armonk, NY, USA). Response was evaluated based on the revised Response Evaluation Criteria in Solid Tumors (RECIST ver. 1.1). Adverse events were classified according to the Common Terminology Criteria for Adverse Events (CTCAE ver. 4.0).
We identified 14 patients treated with bolus 5-FU and l-leucovorin at Hokkaido University Hospital between January 2010 and December 2015. Almost all patients had previously received more than three anti-GC chemotherapy regimens. Patient characteristics are listed in Table 1 and 2. The median number of rapid infusions of 5-FU and l-leucovorin was 7 (range, 5~54) and the median relative dose intensity of 5-FU was 97%.
No patient died from treatment-related causes. The most common treatment-related severe adverse event was neutropenia that occurred in 21.4% of patients treated with bolus 5-FU and l-leucovorin. Only 1 of 14 patients developed treatment-induced febrile neutropenia. All treatment-related adverse events are summarized in Table 3.
Bolus 5-FU and l-leucovorin is reportedly not inferior to S-1 monotherapy for treatment of unresectable GC or to continuous 5-FU monotherapy when administered as first-line chemotherapy.10 Although this regimen is covered by the national health insurance program of Japan, there is no indication for bolus 5-FU and l-leucovorin in the Japanese GC treatment guidelines. The mechanism underlying the anti-cancer effect of continuous 5-FU administration is reportedly different from that of rapid infusion of 5-FU,1112 and therefore, bolus 5-FU and l-leucovorin therapy may be sufficient to elicit an effect against oral fluoropyrimidine-resistant GC. In addition, some patients unable to eat or drink because of a gastrointestinal disorder caused by peritoneal dissemination can be treated with the bolus 5-FU and l-leucovorin regimen.
In our study, 5 of 14 patients achieved stable disease after this treatment and 6 patients survived for more than 6 months after the first treatment. Each of these patients had received S-1 or capecitabine for GC and almost all were heavily treated in the past, which was thought to have prolonged their survival.
Almost all of the patients' performance status was scored as 1 or 2; there was 1 patient whose performance status was scored as 3. Her poor performance status was due to bone-marrow invasion verified by bone-marrow puncture after heavy treatment; however, she strongly desired to be treated with another regimen. Therefore, we administered bolus 5-FU and l-leucovorin after obtaining informed consent.
In the REGARD8 trial, the PFS and OS of the placebo group of patients with unresectable GC were 1.3 months and 3.8 months, respectively, while the GRANITE-1 trial13 reported PFS and OS of the placebo group were 1.4 months and 4.3 months, respectively. The outcomes of the placebo groups of patients with unresectable GC were extremely poor and their PFS and OS were shorter than in our study.
The results of the present study indicate that bolus 5-FU and l-leucovorin treatment might be a viable treatment option for pre-treated unresectable GC. However, this study was limited by its small sample size, retrospective analysis, and being conducted in a single institution. Thus, we are planning a prospective phase II trial to evaluate the efficacy and safety of bolus 5-FU and l-leucovorin for pre-treated unresectable or recurrent GC. The planned trial is registered as UMIN000018882 in the University Hospital Medical Information Network Clinical Trial Registry and we are now recruiting patients from multiple institutions associated with the Hokkaido Gastric Cancer Study Group. The results of the present study will be further evaluated by this subsequent prospective trial.
Figures and Tables
Fig. 1
Progression-free survival (PFS). The median PFS was 1.6 months (95% confidence interval, 1.3~2.0 months).
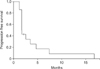
Fig. 2
Overall survival (OS). The median OS was 6.3 months (95% confidence interval, 4.7~7.9 months).

Acknowledgments
The authors would like to thank the patients, their families, and the staff members of the Cancer Center and Department of Gastroenterology and Hepatology of Hokkaido University Hospital. Additionally, they would like to thank Enago (www.enago.jp) for the English language review.
Notes
Conflicts of Interest Yoshito Komatsu received honoraria from Taiho Pharmaceutical Co. Ltd., Yakult Pharmaceutical Industry Co. Ltd., Daiichi-Sankyo Ltd., and Bristol-Myers Squibb. Naoya Sakamoto received honoraria from Bristol-Myers Squibb, MSD, Gilead Sciences, and Otsuka. The other authors have no conflicts of interest that are directly relevant to the content of this manuscript.
References
1. Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008; 9:215–221.
2. Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med. 2008; 358:36–46.
3. Yamada Y, Higuchi K, Nishikawa K, Gotoh M, Fuse N, Sugimoto N, et al. Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naïve patients with advanced gastric cancer. Ann Oncol. 2015; 26:141–148.
4. Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010; 376:687–697.
5. Sawaki A, Ohashi Y, Omuro Y, Satoh T, Hamamoto Y, Boku N, et al. Efficacy of trastuzumab in Japanese patients with HER2-positive advanced gastric or gastroesophageal junction cancer: a subgroup analysis of the Trastuzumab for Gastric Cancer (ToGA) study. Gastric Cancer. 2012; 15:313–322.
6. Wilke H, Muro K, Van Cutsem E, Oh SC, Bodoky G, Shimada Y, et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol. 2014; 15:1224–1235.
7. Shitara K, Muro K, Shimada Y, Hironaka S, Sugimoto N, Komatsu Y, et al. Subgroup analyses of the safety and efficacy of ramucirumab in Japanese and Western patients in RAINBOW: a randomized clinical trial in second-line treatment of gastric cancer. Gastric Cancer. 2016; 19:927–938.
8. Fuchs CS, Tomasek J, Yong CJ, Dumitru F, Passalacqua R, Goswami C, et al. Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet. 2014; 383:31–39.
9. Kang JH, Lee SI, Lim DH, Park KW, Oh SY, Kwon HC, et al. Salvage chemotherapy for pretreated gastric cancer: a randomized phase III trial comparing chemotherapy plus best supportive care with best supportive care alone. J Clin Oncol. 2012; 30:1513–1518.
10. Sawaki A, Yamaguchi K, Nabeya Y, Sakai Y, Osanai H, Denda T, et al. 5-FU/l-LV (RPMI) versus S-1 as first-line therapy in patients with advanced gastric cancer: a randomized phase III non-inferiority trial (ISO-5FU10 Study Group trial). Eur J Cancer Suppl. 2009; 7:364.
11. Parker WB, Cheng YC. Metabolism and mechanism of action of 5-fluorouracil. Pharmacol Ther. 1990; 48:381–395.
12. Longley DB, Harkin DP, Johnston PG. 5-fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer. 2003; 3:330–338.
13. Ohtsu A, Ajani JA, Bai YX, Bang YJ, Chung HC, Pan HM, et al. Everolimus for previously treated advanced gastric cancer: results of the randomized, double-blind, phase III GRANITE-1 study. J Clin Oncol. 2013; 31:3935–3943.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download