Abstract
Purpose
Materials and Methods
Results
Figures and Tables
Table 2
Histopathological characteristics of gastric cancer according to study period

Values are presented as number (%). The sum of the percentages does not equal 100% because of rounding. WD = well differentiated; MD = moderately differentiated; PD = poorly differentiated. *Classification according to the Japanese guidelines.5 †Includes signet-ring cell carcinoma. ‡Display a mixture of discrete morphologically identifiable glandular (tubular/papillary) and signet-ring/poorly-cohesive cellular histological components.
Table 4
Operative methods and curability

Values are presented as number (%). The sum of the percentages does not equal 100% because of rounding. NE = not evaluated (the item was not included as a choice); DG = distal gastrectomy; TG = total gastrectomy; NTG = near total gastrectomy; PG = proximal gastrectomy; PPG = pylorus preserving gastrectomy. *Combined resection was initially evaluated in the 2014 survey.
Notes
The Information Committee: Bang Wool Eom (National Cancer Center), Hye Seong Ahn (SMG-SNU Boramae Medical Center), In Seob Lee (University of Ulsan College of Medicine), Jae-Seok Min (Dongnam Institute of Radiological & Medical Sciences), Young Gil Son (Keimyung Univerisity School of Medicine), Sang Eok Lee (College of Medicine, Konyang University), Ji Hoon Kim (Gangneung Asan Hospital), Se-Youl Lee (Chonbuk National University Medical School), Jie-Hyun Kim (Yonsei University College of Medicine), Sang-Hoon Ahn (Seoul National University College of Medicine), Hyung-Ho Kim (Seoul National University College of Medicine), Young-Woo Kim (National Cancer Center)
Participating Institutions The participating institutions are as follows: The Catholic University of Korea, Bucheon St. Mary's Hospital; The Catholic University of Korea, Seoul St. Mary's Hospital; The Catholic University of Korea, St. Vincent's Hospital; The Catholic University of Korea, Yeouido St. Mary's Hospital; The Catholic University of Korea, Uijeongbu St. Mary's Hospital; The Catholic University of Korea, Incheon St. Mary's Hospital; Gachon University Gil Medical Center; Gangneung Asan Hospital; Konkuk University Medical Center; Konyang University Hospital; Kyungpook National University Hospital; Kyungpook National University Medical Center; Gyeongsang National University Hospital; Kyunghee University Medical Center; Keimyung University Dongsan Medical Center; Korea University Guro Hospital; Korea University Ansan Hospital; Korea University Anam Hospital; Kosin University Gospel Hospital; National Police Hospital; National Cancer Center; National Medical Center; Daegu Catholic University Medical Center; Eulji University Hospital; Dongnam Institution of Radiological & Medical Sciences; Dong-A University Hospital; Myongji Hospital; Pusan National University Hospital; Pusan National University Yangsan Hospital; Bundang Jesaeng Hospital; CHA Bundang Medical Center, CHA University; Samsung Medical Center; Seoul National University Hospital; SMG-SNU Boramae Medical Center; Seoul National University Bundang Hospital; Asan Medical Center; Saegyaero Hospital; Soon Chun Hyang University Bucheon Hospital; Soon Chun Hyang University Seoul Hospital; Soon Chun Hyang University Cheonan Hospital; Ajou University Medical Center; Hansarang Hospital; Gangnam Severance Hospital; Severance Hospital; Wonju Severance Christian Hospital; Yeungnam University Medical Center; Presbyterian Medical Center; Ulsan University Hospital; Wonkang University Hospital; Korea Cancer Center Hospital; Ewha Womans University Mokdong Hospital; Inje University Busan Paik Hospital; Inje University Haeundae Paik Hospital; Inha University Hospital; Seoul Red Cross Hospital; Chonnam National University Hospital; Chonnam National University Hwasun Hospital; Chonbuk National University Hospital; Jeju National University Hospital; Chosun University Hospital; Chung-Ang University Hospital; Chinjujeil Hospital; Cheongju St. Mary's Hospital; Chungnam National University Hospital; Chungbuk National University Hospital; Gyeonggi-do Medical Center Paju Hospital; Hallym University Dongtan Sacred Heart Hostpial; Hallym University Chuncheon Sacred Heart Hospital; Hanyang University Seoul Hospital.
Appendix
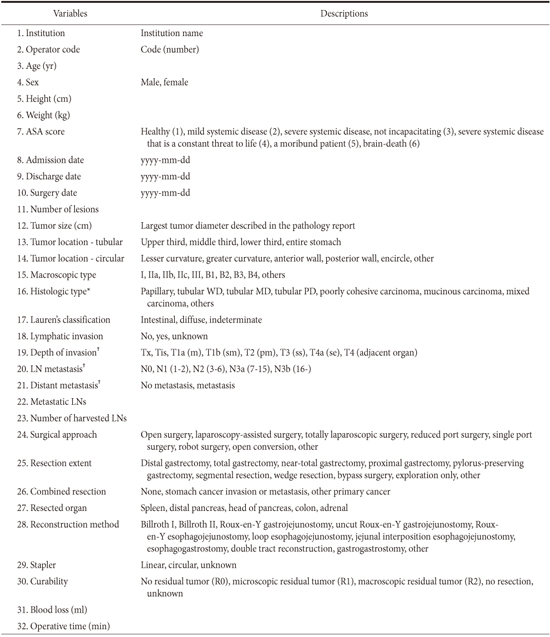
Appendix 1
Survey data




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download