Introduction
Although gastroduodenal intussusception is a rare condition itself among gastrointestinal obstructive disease, some documented cases were reported previously.(1-8) However, most cases have less typical images of gastroduodenal intussusception with the size less than 5 cm. Herein this article describe the gastroduodenal intussusception resulted by a 10 cm-sized hyperplastic polyp treated by laparoscopic wedge resection with valuable diagnostic images.
Case Report
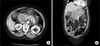
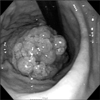
A 76-year-old female presented to our emergency department with a 3-day history of nausea and vomiting. She experienced a cerebral vascular stroke 30 years beforehand and has taken medication for diabetes and hypertension for 10 years. Two years beforehand a 5 cm-sized hyperplastic polyp was found with a gastrofiberscope (GFS), but she declinedpolypectomy because of the possible complications such as bleeding and perforation. Mild tenderness was found on the epigastrium during physical examination. Laboratory examination revealed a leukocytosis (white blood cell: 15,980/mm3, normal range: 4,600~10,000/mm3), elevated erythrocyte sedimentation rate (55 mm/hr, normal range: 0~20 mm/hr), elevated C-reactive protein (77.41 mg/L, normal range: 0~10 mg/L) and mild hyperamylasemia (161 IU/L, normal range: 37~160 IU/L). Computed tomography (CT) revealed gastroduodenal intussusception with herniation of a large intraluminal mass into the 1st and 2nd portions of the duodenum and peripancreatic fat infiltration without a fluid collection (Fig. 1). Endoscopic examination with a GFS showed that the intussusception had already been resolved and that the intussusceptions was due to a 10 cm-sized pedunculated masson the gastric lower body anterior wall (Fig. 2). Biopsy was performed, which confirmed the diagnosis of hyperplastic polyp. Because of the increased size of the hyperplastic polyp and the event of gastroduodenal intussusception, the patient and her family agreed to surgical treatment. With a laparoscopic approach, we made a gastrostomy at the anterior wall with the Harmonic Scalpel (Ethicon Endo-surgery, Cincinnati, OH, USA) and exposed the mass to perform secure wedge resection because of its size. We performed resection with Endo-GIA 60 mm (Ethicon Endo-surgery) (Fig. 3). Gastrotomy site was closed with Endo-GIA 60 mm (Ethicon Endo-surgery). The operation took 20 minutes, and it was a proper and safe procedure for the elderly patient with several comorbidities. The patient recovered and resumed an oral diet on the 2nd postoperative day.
Histopathologic examination of the surgically resected tumor revealed a 10×6 cm-sized hyperplastic polyp with a 0.3×0.3 cm carcinoma in situ lesion (Fig. 4). During the subsequent 2 years of follow-up, there has been no recurrence of gastric cancer or gastroduodenal intussusception.
Discussion
Gastroduodenal intussusception is a condition in which the full thickness of the gastric wall invaginates into the duodenum. In nearly all cases, a gastric tumor is present at the apex of the intussusception.(1) Although gastroduodenal intussusception is a very rare condition in adults, there have been documented cases with specific identified lead points.(1-8) Benign neoplasms, gastrointestinal stromal tumors (GISTs) and polypoid gastric adenocarcinomas that are usually located in the antrum and 5 cm or less in size have been reported to be the cause of gastroduodenal intussusception.
The symptoms of gastroduodenal intussusception canvary according to the reducibility of the cause of the intussusception. If the cause of the intussusception is easily reducible, symptoms canbe more intermittently developed with mild degree.(5) Otherwise, if the lesion is too large to be reduced by itself, prolonged symptoms of upper gastrointestinal obstruction and even pancreatitis may develop.(1) Our patient presented a 3-day history of symptoms and pancreatitis. However, when we performed endoscopy, we saw that the intussusception had already been resolved. We presumed that airflow during endoscopic examination with the GFS assisted the reduction of the intussusception.
Diagnosis was usually confirmed by CT or sonography in other reports, and CT was the more commonly performed and reliable method.(4,8,9) However, there were few figures that showed the typical image of a gastroduodenal intussusceptions with transpyloric prolapse of a mass. Otherwise, we obtained the typical and unique CT images of the gastroduodenal intussusception, especially in the coronal plane.
Treatment for gastroduodenal intussusception should be focused on removal of its cause. There was one report in which a laparoscopic distal gastrectomy with Billroth-II anastomosis was performed for anantral GIST, which served as the lead point for agastroduodenal intussusception.(5) In our case laparoscopic wedge resection with eversion method was performed.
Kang et al.(10) reported the neoplastic transformation of gastric hyperplastic polyps, including a 1.1% transformation rate to adenocarcinoma among 274 gastric hyperplastic polyps, and showed that neoplastic transformation had a significant relationship with hyperplastic polyps greater than 1 cm with a pedunculated shape. Because our patient had a 0.3×0.3 cm carcinoma in situ lesion in the polyp, cancer cell spillage during wedge resection with the eversion method was a concern in this patient. However, during 2 years of follow-up, there has been no evidence of recurrence of cancer or gastroduodenal intussusception.
We presented the unique case and images of gastroduodenal intussusception caused by a large hyperplastic polyp. We could successfully resect the large hyperplastic polyp laparoscopically, but cautions must be taken to prevent cancer cell spillage when performing laparoscopic resection with an eversion method.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download