Abstract
Purpose
The aim of this study was to assess and compare the efficacies of proton pump inhibitor-based triple therapy and bismuth-based quadruple therapy as first-line treatments for Helicobacter pylori eradication in Korean children.
Methods
We retrospectively reviewed the data of children who had been diagnosed with H. pylori infection at the Seoul National University Bundang Hospital from March 2004 to August 2012. The patients were randomly assigned to receive either triple therapy consisting of omeprazole, amoxicillin, and clarithromycin for 2 weeks (OAC group) or quadruple therapy comprising omeprazole, amoxicillin, metronidazole, and bismuth salts for 1 week (OAMB group). The patients were evaluated for eradication of H. pylori infection at 4 weeks after the completion of the treatment.
Results
Of the 129 children enrolled in this study, 118 (91.5%) were included in the final analysis. The eradication rates in OAC and OAMB groups were 67.7% (42/62) and 83.9% (47/56), respectively, which were significantly different between the 2 treatment groups (p=0.041). The eradication rates in the OAMB group during the periods 2004-2006, 2007-2009, and 2010-2012 were superior to those in the OAC group.
Helicobacter pylori is a gram-negative, spiral-shaped bacterium which colonizes in the gastric mucosa and often causes gastritis or peptic ulcer disease in both adults and children [1]. As chronic H. pylori infection, which probably begins in childhood, is thought to be a strong risk factor for gastric adenocarcinoma and gastric lymphoma, its elimination has been regarded as the most important strategy for reducing mortality in adulthood [2].
Since the introduction of the initial published guidelines, the first-line treatment option for H. pylori infection has been triple therapies, which consist of a proton pump inhibitor (PPI) and 2 antibiotics [3]. However, recent studies have indicated declining rates of H. pylori eradication with the standard triple therapies worldwide [4,5]. It is considered to be related to the increasing prevalence of H. pylori resistance to antibiotics, particularly clarithromycin [6]. As a result, bismuth-containing treatments have been suggested as the first-line treatment in regions with high clarithromycin resistance [2].
Since clarithromycin is widely used for the treatment of respiratory infections in the Korean pediatric population, H. pylori resistance to clarithromycin could be expected to increase over time. Moreover, clarithromycin resistance has been known to adversely affect the eradication rates of H. pylori infection in children [7]. Therefore, alternative treatment options should be suggested as an initial therapy for the eradication of H. pylori infection in Korean children.
We aimed to determine the efficacy of PPI-based triple therapy over the last decade in Korea. Further, we attempted to evaluate the effectiveness of bismuth-based quadruple therapy and to compare it with that of the standard 2-week triple therapy as the first-line treatment for H. pylori eradication in Korean children.
We retrospectively reviewed the data of children who had presented with gastrointestinal symptoms and who had been diagnosed with H. pylori infection at the Seoul National University Bundang Hospital from March 2004 to August 2012. The diagnosis of H. pylori infection was confirmed by endoscopic biopsy-based methods: histopathology and a rapid urease test. We excluded patients who had received antibiotics or acid-suppressive agents 4 weeks before the tests. This study was conducted with approval from the Ethics Committee of the Seoul National University Bundang Hospital.
The patients were randomly assigned to receive one of the 2 eradication regimens for H. pylori infection: triple therapy regimen (omeprazole, amoxicillin, clarithromycin, OAC group) and quadruple regimen (omeprazole, amoxicillin, metronidazole, bismuth salts, OAMB group). The triple therapy regimen consisted of omeprazole (1 mg/kg per day; up to 20 mg twice daily), clarithromycin (15 mg/kg per day; up to 500 mg twice daily), and amoxicillin (50 mg/kg per day; up to 1 g twice daily) for 14 days. The quadruple regimen consisted of omperazole (1 mg/kg per day; up to 20 mg twice daily), amoxicillin (50 mg/kg per day; up to 1 g twice daily), metronidazole (20 mg/kg per day), and bismuth citrate (8 mg/kg per day) for 7 days.
Eradication of H. pylori infection was evaluated in all patients at 4 weeks after the completion of treatment by the 13C-urea breath test (UBT) or endoscopic biopsy-based methods. A UBT was performed with 75 mg 13C-urea without a test meal, as previously described [8]. A delta over baseline value exceeding 4 ‰ indicated a positive result.
Compliance with the drugs was assessed by questionnaires at the follow-up visit. Patients were also asked about any side-effects of the treatments.
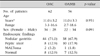
Of the 129 patients enrolled in this study, 11 (4 in the OAC group and 7 in the OAMB group) did not return for the follow-up evaluation. Among 118 (91.5%) children who were included in the final analysis, 62 were assigned to the OAC group and 56 were allocated to the OAMB group. There were no significant differences in demographics or dropout rates between the 2 treatment groups (Table 1).
The compliance with the 2 regimens was excellent in all patients who completed their treatments. Moreover, no side-effects were seen during the period of the treatments.
The eradication rate was 67.7% (42/62) in the OAC group and 83.9% (47/56) in the OAMB group. A significant difference was obtained between the 2 treatment groups in the H. pylori eradication rates (p=0.041, Fig. 1).
The eradication rates during the following 3 periods were also compared: 2004-2006, 2007-2009, and 2010-2012. The eradication rates during the periods in the OAC group were 69.6% (16/23), 75.9% (22/29), and 40% (4/10), respectively. In the OAMB group, the eradication rates for the abovementioned periods were 79.2% (19/24), 88.9% (8/9), and 87% (20/23), respectively (Fig. 2). The eradication rates in the OAMB group during each period were all superior to those in the OAC group, especially during 2010-2012 (p=0.01).
To our knowledge, this is the first report that compares the efficacies of the triple and quadruple therapy therapies as the first-line treatment for H. pylori eradication in a pediatric population in Korea. We also observed the trend of eradication success with the standard triple therapy in Korean children over the last decade.
Based on this study, the H. pylori eradication rate of the standard 2-week triple therapy was only 67.7%, which is less than the 85-90% threshold that most consensus guidelines recommend [2,9]. Moreover, our results revealed that the effectiveness of the triple therapy has decreased over time, corresponding with the findings of several previous studies [4]. According to other studies that included Korean children, the rate of H. pylori eradication with the 2-week triple therapy comprising PPI, amoxicillin, and clarithromycin was 84.6% in 1998-2000 and 74% in 1999-2004 [10,11]. The European pediatric treatment registry recently reported the results from the use of 27 different regimens in 518 children, where the eradication rate by the standard 2-week triple therapy, i.e., the same regimen as ours, was 60.5% [12].
The success of H. pylori eradication is closely associated with clarithromycin resistance of H. pylori, which has been reported to develop variably according to geographic regions. The clarithromycin resistance rate in Europe had increased from 9% in 1998 to 17.6% in 2008-2009 [2]. A multicenter study that included children living in Europe revealed a clarithromycin resistance rate of 24% [13]. In a study on 222 Korean adults, clarithromycin resistance was reported to have increased from 16.7% in 2003-2005 to 38.5% in 2007-2009 [14]. A study carried out in a small number of Korean children revealed a clarithromycin resistance rate of 25% over 7 years, from 2003 to 2009 [15].
Evidence-based guidelines from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition have recently suggested that clarithromycin-based triple therapy can only be recommended as first-line therapy if the clarithromycin resistance rate in the area is known to be low (<20%) [9]. It is also recommended that the test for antibiotic susceptibility to clarithromycin should be performed before the initial clarithromycinbased triple therapy in areas/populations where the known resistance rate of H. pylori to clarithromycin is high (>20%). Additionally, a recent review has outlined general rules for treating patients with H. pylori infection; clarithromycin-based regimen should not be recommended if prescription of clarithromycin is locally common or if the patient has been administrated clarithromycin in the past, for any indication [6].
There have been several efforts to improve the eradication rates of H. pylori infection by the combination of multiple drugs or by increasing the dose of medication or duration of treatment, which could suggest alternative first-line therapies for H. pylori infection. Bismuth salts are known to inhibit H. pylori growth and are effective in eradicating the bacterium. The bismuth-based regimens have been reported not to cause more adverse events than the standard clarithromycin-containing triple therapy [2,16]. In a recent report, bismuth-containing triple therapies were found to be more efficacious than PPI-based ones as the first-line treatment for children (77% vs. 64%) [12]. As a result, bismuth salts have been included as the first-line treatment in the latest guidelines for H. pylori infection in children [9,17]. Furthermore, the Maastricht IV Consensus Report recommended bismuth-containing quadruple therapies as the first choice in regions with high clarithromycin resistance [2].
In regard to metronidazole, which is an important antibiotics in bismuth-based quadruple therapy, the frequencies of resistance to the antibiotics in Korea have been reported to be variable in a range of 27.6% to 66.2% according to the study populations [14,18]. A limited study has recently reported a metronidazole resistance rate of 17.8% in Korean children [15]. Despite a high rate of metronidazole resistance, the outcome with quadruple therapy has not shown a significant difference between metronidazole-sensitive strain and metronidazole-resistant ones [19]. Moreover, based on the results from a European register, the eradication rate of a regimen, where the clarithromycin was substituted with metronidazole in standard PPI-based triple therapy, was 66.7%, which showed no significant difference between the two regimens [12]. However, the addition of PPI to bismuth triple therapy has been known to improve the efficacy and to overcome the metronidazole resistance [20].
In 2009, the Korean College of Helicobacter and Upper Gastrointestinal Research group for H. pylori produced guidelines for the diagnosis and treatment of H. pylori infection. Based on the guidelines, bismuth-containing therapy is recommended only in the case of treatment failure of first-line regimens [21]. In adults, there have been studies comparing the standard triple and quadruple therapies, yielding controversial results for the eradication rates of the 2 regimens [22,23].
Few reports have compared the efficacies of the standard triple therapy and bismuth-based quadruple therapy in pediatric populations. Only 1 randomized clinical trial was performed during 2003-2004, where the regimens were applied to Iranian children for 10 days. In that study, the H. pylori eradication rates were not significantly different between the 2 groups [24]. Another comparison study, also performed in Iran, revealed a 91.9% H. pylori eradication rate with bismuth-based quadruple therapy, as compared with the 82.1% success rate of the 2-week standard triple therapy [25].
There have been no suggested recommendations for children and adolescents with H. pylori infection in Korea. Therefore, adequate treatment regimens for H. pylori infection should be determined for Korean pediatric population because of the increasing resistance to clarithromycin in Korea. In our study, the eradication rate of bismuth-based quadruple therapy (83.9%) was sigsignificantly higher than that of clarithromycin-based 2-week triple therapy (67.7%), indicating that the bismuth-based 1-week quadruple therapy should be recommended as the initial treatment regimen for H. pylori infection in children.
In conclusion, bismuth-based quadruple therapy can be suggested as an alternative first-line treatment, especially for Korean children. Further trials in other settings, particularly in pediatric populations, are required to enable the application of such practical guidelines to the Korean pediatric patients.
Figures and Tables
Fig. 1
Comparison of the Helicobacter pylori eradication rates of 2 different regimens. The eradication rate in the OAMB group was significantly higher than that in the OAC group (p=0.041). OAC: omeprazole, amoxicillin, clarithromycin, OAMB: omeprazole, amoxicillin, metronidazole, bismuth salts.

Fig. 2
Serial eradication rates of the Helicobacter pylori infection during 3 periods of time. The eradication rates in the OAMB group during each period were all superior to those in the OAC group, especially during 2010-2012 (p=0.01). OAC: omeprazole, amoxicillin, clarithromycin, OAMB: omeprazole, amoxicillin, metronidazole, bismuth salts.

References
1. Suerbaum S, Michetti P. Helicobacter pylori infection. N Engl J Med. 2002. 347:1175–1186.
2. Malfertheiner P, Megraud F, O'Morain CA, Atherton J, Axon AT, Bazzoli F, et al. European Helicobacter Study Group. Management of Helicobacter pylori infection--the Maastricht IV/Florence Consensus Report. Gut. 2012. 61:646–664.

3. Gold BD, Colletti RB, Abbott M, Czinn SJ, Elitsur Y, Hassall E, et al. North American Society for Pediatric Gastroenterology and Nutrition. Helicobacter pylori infection in children: recommendations for diagnosis and treatment. J Pediatr Gastroenterol Nutr. 2000. 31:490–497.

4. Kim SY, Jung SW. Helicobacter pylori eradication therapy in Korea. Korean J Gastroenterol. 2011. 58:67–73.
5. Zullo A, Hassan C, Ridola L, De Francesco V, Vaira D. Standard triple and sequential therapies for Helicobacter pylori eradication: An update. Eur J Intern Med. 2012. [Epub ahead of print].
6. Graham DY, Fischbach L. Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut. 2010. 59:1143–1153.

7. Kalach N, Benhamou PH, Campeotto F, Bergeret M, Dupont C, Raymond J. Clarithromycin resistance and eradication of Helicobacter pylori in children. Antimicrob Agents Chemother. 2001. 45:2134–2135.

8. Yang HR, Seo JK. Diagnostic accuracy of the C-urea breath test in children: adjustment of the cut-off value according to age. J Gastroenterol Hepatol. 2005. 20:264–269.

9. Koletzko S, Jones NL, Goodman KJ, Gold B, Rowland M, Cadranel S, et al. H pylori Working Groups of ESPGHAN and NASPGHAN. Evidence-based guidelines from ESPGHAN and NASPGHAN for Helicobacter pylori infection in children. J Pediatr Gastroenterol Nutr. 2011. 53:230–243.

10. Choi IK, Lee SY, Chung KS. Effect of one- or two-week triple therapy with omeprazole, amoxicillin, and clarithromycin on eradication of Helicobacter pylori infection in children. Korean J Pediatr Gastroenterol Nutr. 2002. 5:19–25.

11. Choi J, Jang JY, Kim JS, Park HY, Choe YH, Kim KM. Efficacy of two triple eradication regimens in children with Helicobacter pylori infection. J Korean Med Sci. 2006. 21:1037–1040.

12. Oderda G, Shcherbakov P, Bontems P, Urruzuno P, Romano C, Gottrand F, et al. European Pediatric Task Force on Helicobacter pylori. Results from the pediatric European register for treatment of Helicobacter pylori (PERTH). Helicobacter. 2007. 12:150–156.

13. Koletzko S, Richy F, Bontems P, Crone J, Kalach N, Monteiro ML, et al. Prospective multicentre study on antibiotic resistance of Helicobacter pylori strains obtained from children living in Europe. Gut. 2006. 55:1711–1716.

14. Hwang TJ, Kim N, Kim HB, Lee BH, Nam RH, Park JH, et al. Change in antibiotic resistance of Helicobacter pylori strains and the effect of A2143G point mutation of 23S rRNA on the eradication of H. pylori in a single center of Korea. J Clin Gastroenterol. 2010. 44:536–543.

15. Kim YM, Lee YJ, Oh SH, Sung H, Kim MN, Kim KM. Antimicrobial resistance of Helicobacter pylori isolated from Korean children. Korean J Pediatr Gastroenterol Nutr. 2011. 14:45–51.

16. Ford AC, Malfertheiner P, Giguere M, Santana J, Khan M, Moayyedi P. Adverse events with bismuth salts for Helicobacter pylori eradication: systematic review and meta-analysis. World J Gastroenterol. 2008. 14:7361–7370.

17. Ertem D. Clinical practice: Helicobacter pylori infection in childhood. Eur J Pediatr. 2012. [Epub ahead of print].
18. Kim JM. Antibiotic resistance of Helicobacter pylori isolated from Korean patients. Korean J Gastroenterol. 2006. 47:337–349.
19. Laine L, Hunt R, El-Zimaity H, Nguyen B, Osato M, Spénard J. Bismuth-based quadruple therapy using a single capsule of bismuth biskalcitrate, metronidazole, and tetracycline given with omeprazole versus omeprazole, amoxicillin, and clarithromycin for eradication of Helicobacter pylori in duodenal ulcer patients: a prospective, randomized, multicenter, North American trial. Am J Gastroenterol. 2003. 98:562–567.

20. Katelaris PH, Forbes GM, Talley NJ, Crotty B. A randomized comparison of quadruple and triple therapies for Helicobacter pylori eradication: The QUADRATE Study. Gastroenterology. 2002. 123:1763–1769.

21. Kim N, Kim JJ, Choe YH, Kim HS, Kim JI, Chung IS. Korean College of Helicobacter and Upper Gastrointestinal Research. Korean Association of Gastroenterology. Diagnosis and treatment guidelines for Helicobacter pylori infection in Korea. Korean J Gastroenterol. 2009. 54:269–278.

22. Jang HJ, Choi MH, Kim YS, Seo YA, Baik KH, Baik IH, et al. Effectiveness of triple therapy and quadruple therapy for Helicobacter pylori eradication. Korean J Gastroenterol. 2005. 46:368–372.
23. Jo HJ, Lee DH, Kang SJ, Kim MN, Kim SH, Park JM, et al. Comparison of the efficacy of bismuth containing PPI-based quadruple therapy with PPI-based triple therapy only as first-line treatment for Helicobacter pylori infection. Korean J Gastrointest Endosc. 2008. 37:259–264.
24. Bahremand S, Nematollahi LR, Fourutan H, Tirgari F, Nouripour S, Mir E, et al. Evaluation of triple and quadruple Helicobacter pylori eradication therapies in Iranian children: a randomized clinical trial. Eur J Gastroenterol Hepatol. 2006. 18:511–514.

25. Dehghani SM, Erjaee A, Imanieh MH, Haghighat M. Efficacy of the standard quadruple therapy versus triple therapies containing proton pump inhibitor plus amoxicillin and clarithromycin or amoxicillin-clavulanic acid and metronidazole for Helicobacter pylori eradication in children. Dig Dis Sci. 2009. 54:1720–1724.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download