Abstract
Purpose
Epstein-Barr virus (EBV) hepatitis is a usually asymptomatic and self-limiting disease in immunocompetent patients. However, the range of severity is wide, and the serological diagnosis is typically difficult until the convalescent phase. Thus, we examined the value of plasma EBV DNA real-time quantitative polymerase chain reaction (RT-qPCR) in EBV hepatitis for the timely diagnosis and the relationship between EBV viral load and clinical severity.
Methods
Sixty samples were confirmed as having EBV infection by RT-qPCR with the EBV BALF5 gene sequence. We examined the clinical characteristics of EBV hepatitis by reviewing medical records.
Results
The median total duration of fever was 8 days (range: 0-13 days). The mean peak value of aspartate aminotransferase (AST) was 241±214 U/L, and the mean peak value of alanine aminotransferase (ALT) was 298±312 U/L. There was no correlation between the serum levels of liver enzyme and plasma EBV DNA titer (p=0.1) or between median total duration of fever and EBV DNA titer (p=0.056). The median age of the EBV VCA IgM-negative group was lower compared with the EBV VCA IgM-positive group in EBV hepatitis (2 years vs. 6 years, p=0.0009).
Epstein-Barr virus (EBV) belongs to the family Herpesviridae and spreads by droplets and close contact, causing infectious mononucleosis and B cell-related malignancies [1]. Infectious mononucleosis presents as fever, lymphadenopathy, skin rash, hepatosplenomegaly, and elevated liver enzymes in 70% to 80% of patients [1,2].
EBV hepatitis that is due to primary infection of EBV is usually asymptomatic and self-limiting, but occasionally accompanies jaundice and hepatic failure and is rarely diagnosed serologically until the convalescent phase [3,4].
The diagnosis of EBV infection depends primarily on serological markers. Antibodies against viral capsid antigen (VCA), early antigen (EA), and EBV nuclear antigen (EBNA) are the main serological markers. VCA IgM is used as a serological marker to diagnose acute infections. However, the appearance of antibodies does not coincide with the onset of symptoms-instead, it typically occurs after the peak of the immune reaction. Thus, a patient with infectious mononucleosis can be VCA IgM-negative. This phenomenon is more common in infants and immunocompromised hosts who have low production of antibodies.
Generally, the clinical severity of EBV infection is not serious in children under 5 years of age, but Cheng et al. [5] reported contradictory results, observing that 76.8% of patients who developed typical infectious mononucleosis were under 7 years of age including young infants. Further, fulminant hepatitis could be present in EBV-associated hemophagocytic lymphohistiocytosis. Hence, more sensitive detection methods for EBV are required in infants, young children, and immunocompromised hosts [6].
Real time-quantitative polymerase chain reaction (RT-qPCR) is a compatible method that can satisfy this need and compensate for the drawbacks of serological tests [7]. The sensitivity of RT-qPCR is higher than that of serological tests, and early detection is possible, even when the viral load is not high. Baek et al. [8] recently reported the diagnosis of reactivated EBV infection by RT-qPCR in hepatitis A infection, suggesting that the unusual course of hepatitis A infection might be due to reactivated EBV infection, which can be underdiagnosed by serological testing. The detection of reactivated EBV infection is important in anticipating the prognosis of hepatitis, because reactivated EBV can recruit cytotoxic T cells to inflammatory sites and delay recovery of the liver.
The purpose of this study was to evaluate the clinical importance of EBV DNA RT-qPCR in the early diagnosis and anticipating the clinical course of EBV hepatitis when the patient shows VCA IgM-negative.
From January 2006 to December 2010, we collected plasma samples of admitted patients aged under 18 years with suspected EBV hepatitis at Wonju Christian Hospital, Yonsei University, South Korea. The inclusion criteria were as follows: 1) the patients who have at least one of symptoms among fever, cervical lymphadenopathy, or hepatosplenomegaly; 2) the patients who have atypical lymphocytosis which we defined the counts of atypical lymphocytes >5% to 10%; and 3) the patients who have elevated liver enzymes [aspartate aminotransferase (AST), alanine aminotransferase (ALT)] and EBV PCR positive.
On the day of admission, we measured serological markers for EBV and performed EBV DNA RT-qPCR. Sixty patients were included in this study with confirmed EBV hepatitis by plasma EBV DNA RT-qPCR. The approval of institutional review board was exempted, because this study is retrospective clinical review study and the samples were collected after routine diagnostic sampling for peripheral blood smears.
The definition of hepatosplenomegaly was established by the physical examination: palpation 2 cm below both costal margins. The duration of fever was defined as the total duration of fever, from preadmission to subsiding of the fever. The values of liver enzymes were recorded as the highest peak value in each patient.
Whole blood was centrifuged with Ficoll-Paque™ (STEMCELL Technologies Inc., Vancouver, Canada) to obtain plasma samples. DNA was extracted from the plasma using the QIAamp DNA Blood mini Kit (Qiagen, Düsseldorf, Germany) and stored at -70℃. PCR primers were designed using the BALF5 gene sequence, encoding EBV DNA polymerase: forward 5'-CCC TGT TTA TCC GAT GGA ATG-3' and reverse 5'-CGG AAG CCC TCT GGA CTT C-3'. The fluorogenic probe sequence was: 5'-TGT ACA CGC ACG AGA AAT GCG CC-3' [9].
As a positive control, a plasmid that contained the BALF5 gene was constructed, termed pGEM-BALF5. RT-qPCR was performed on a Rotorgene 3,000 (Corbett Research, Sydney, Australia), using the following program: 15 min at 95℃ and 45 cycles of 15 sec at 94℃, 20 sec at 60℃, and 20 sec at 72℃. A positive threshold cycle (Ct) was established at 32 for each sample, and the cutoff for EBV-associated disease was 5,000 copies/µg DNA.
The association of the peak liver enzyme value and EBV DNA concentration, the correlation between total fever duration and viral load, and the difference in serum levels of liver enzymes in case of EBV single infection and coinfection with other microorganisms were examined. In addition, the clinical differences between EBV VCA IgM-positive and EBV VCA IgM-negative patients were analyzed.
Statistical analysis was performed using SPSS 13.0 (SPSS Inc., Chicago, IL, USA) and GraphPad Prism 5.02 (GraphPad Software, San Diego, CA, USA). Student's t-test and Fisher's exact test were used. p<0.05 was considered significant.
A total of 60 patients were diagnosed as EBV hepatitis. The male to female ratio was 39:21 around 2:1. The range of ages was 2 months to 18 years, and the median age was 2.6 years of age. Thirteen patients were EBV VCA IgM-positive (21.6%); the median age of these patients was 6 years (range: 2-12), whereas the median age of EBV VCA IgM-negative patients was 2 years (range: 0.2-18) (p=0.0009) (Fig. 1).
The median total duration of fever in all EBV hepatitis patients was 8 days (range: 0-26 days). The median total duration of fever in the EBV VCA IgM-positive group was significantly higher than that of the EBV VCA-IgM negative group [10 days (range: 2-25 days) vs. 5 days (range: 0-26 days), p=0.0025].
With regard to reactivation of EBV infection (defined as EBNA IgG-positive and EBV RT-qPCR-positive), the rate of EBV reactivation was higher in EBV VCA IgM-negative patients than that in EBV VCA IgM-positive subjects (19/47, 40% vs. 1/13, 7%, p=0.04) (Table 1).
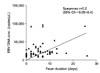
The mean peak level of AST was 241±214 U/L, and the mean peak level of ALT was 298±312 U/L. There was no significant association between peak levels of ALT and EBV VCA IgM positivity (p=0.84). The peak levels of ALT and plasma concentrations of EBV-DNA did not correlate significantly (p=0.1), nor did total duration of fever and plasma concentrations of EBV DNA (p=0.056, R=0.2) (Fig. 2).
There were 2 cases of IgM-positive hepatitis A, which showed EBV reactivation and their peak levels of ALT were 676 U/L and 1,235 U/L, respectively. Other viruses, such as cytomegalovirus and rotavirus, and bacteria, such as M. pneumoniae, were also detected (Table 2). In these co-infected cases, the levels of peak ALT were not higher than those in single infection. There were 1 case with EBV-associated hemophagocytic lymphohistiocytosis and 2 cases with Kawasaki disease, in which the serum levels of total bilirubin and direct bilirubin were elevated and prothrombin time was prolonged.
The rate of liver involvement in infectious mononucleosis by EBV reaches up to 80%, but EBV hepatitis is usually asymptomatic and only detected as elevated serum levels of liver enzymes [10]. Cholestasis is rarely observed, and elevated levels of alkaline phosphatase and total bilirubin are noted occasionally [2]. However, severe hepatitis or hepatic failure can develop by EBV. The main mechanism of liver injury due to EBV is the infiltrations of cytotoxic T cells into the periportal area and increased levels of proinflammatory cytokines not by direct cell invasion of viruses [3].
Primary EBV infection ends up as a latent infection in B cells, which can be reactivated when immune surveillance in the host is impaired. Reactivated EBV infection has somewhat different clinical characteristics compared with primary EBV infection. The production of EBV VCA IgM is lower, and only one or two typical manifestations of infectious mononucleosis were present in reactivated EBV infection [11]. However, with regard to liver injury, the recruitment of cytotoxic T cells can be more vigorous in reactivated EBV infection than in primary EBV infection [11]. In addition, the incidence of undetected chronic hepatitis by EBV might be underestimated [11]. Our data showed that there were significantly more reactivated cases in the EBV VCA IgM-negative group than in the EBV VCA IgM-positive group.
Recently, EBV DNA RT-qPCR has been performed by several institutes in South Korea [8,12], generating more data on EBV to detect the causes of hepatitis and increasing our understanding of EBV hepatitis.
There are several methods of detecting EBV, such as serological studies, viral cultures, DNA- and mRNA-based tests, and immunohistochemistry of biopsy samples [13]. Clinically, serological studies have been used most frequently, but this method has several drawbacks as a diagnostic tool for acute EBV infection-it is less sensitive in infants, young children and immunocompromised hosts, and because there is window period in which antibodies are not produced, false negative results are possible [14].
RT-qPCR is more sensitive than ELISA and can be used to diagnose acute EBV infection, compensating for the disadvantages of ELISA. Pitetti et al. [15] reported that patients with detectable viral loads have more prominent manifestations of infectious mononucleosis than those without detectable loads. They found that the period of plasma EBV positivity-ie, viremia-is not long [15]. Bauer et al. [16] reported that all patients with infectious mononucleosis were positive by EBV DNA RT-qPCR within 12 days after the onset of symptoms. Hence, compared with ELISA for EBV-VCA IgM, which shows a positive conversion within a maximum 4 wks after the initiation of symptoms, RT-qPCR is more sensitive method than serological tests in the acute phase. Similar results were reported by Cheng et al. [5]
Various samples can be used for the detection of EBV-DNA, such as whole blood, mononuclear cells, plasma and serum. We used plasma samples, because we wanted to exclude latent EBV infections and prove that the current EBV viremia caused hepatitis. Serum might contain EBV from cells that are destroyed while a blood clot is being formed [17,18].
Our data suggest that plasma EBV load may not be associated with the severity of hepatitis or total fever duration. Several reports support this result that the hepatotoxicity of EBV might be due to infiltrated cytotoxic T cells, not by viral invasion into hepatocytes [19-21]. Thus, the severity of hepatotoxicity depends on the intensity of immune reactions in individual host. Age, genetic susceptibility, and variations in inflammatory genes can affect the intensity of immune reactions. Suh et al. [22] reported 8 cases of EBV hepatitis in immunocompetent adults, their data also support that hepatic injury is caused by aggregating cytotoxic T cells in the periportal area, not by the ballooning of hepatocytes or granuloma.
Based on this mechanism of liver injury, we can treat severe EBV hepatitis with short-term corticosteroids instead of antiviral agents to block the migration and aggregation of cytotoxic T cells in the periportal area. This effect has been demonstrated by Yuge et al. [23] and Ma et al. [24]. Corticosteroid treatment in EBV infection is not unusual, because it is administered temporarily for serious infectious mononucleosis. Hence, the indication for corticosteroid might be extended to severe EBV hepatitis. Further multicenter collaborations would be required to validate its practical clinical application.
In conclusion, plasma EBV RT-qPCR is useful in diagnosing EBV hepatitis in infants and children during the acute phase, and the detection of EBV can affect the treatment strategy for serious cases.
Figures and Tables
Fig. 1
The age difference between Epstein-Barr virus (EBV) IgM positive group and EBV IgM negative group. The median age of EBV IgM negative group was significantly younger than that of EBV IgM positive group (2 years of age vs. 6 years of age, p=0.0009). *p<0.001.

Fig. 2
The association between total fever duration and Epstein-Barr virus (EBV) DNA concentration. The correlation was not statistically significant (p=0.056).
References
1. Odumade OA, Hogquist KA, Balfour HH. Progress and problems in understanding and managing primary Epstein-Barr virus infections. Clin Microbiol Rev. 2011. 24:193–209.

2. Kofteridis DP, Koulentaki M, Valachis A, Christofaki M, Mazokopakis E, Papazoglou G, et al. Epstein Barr virus hepatitis. Eur J Intern Med. 2011. 22:73–76.

3. Kimura H, Nagasaka T, Hoshino Y, Hayashi N, Tanaka N, Xu JL, et al. Severe hepatitis caused by Epstein-Barr virus without infection of hepatocytes. Hum Pathol. 2001. 32:757–762.

4. Palanduz A, Yildirmak Y, Telhan L, Arapoglu M, Urganci N, Tufekci S, et al. Fulminant hepatic failure and autoimmune hemolytic anemia associated with Epstein-Barr virus infection. J Infect. 2002. 45:96–98.

5. Cheng CC, Chang LY, Shao PL, Lee PI, Chen JM, Lu CY, et al. Clinical manifestations and quantitative analysis of virus load in Taiwanese children with Epstein-Barr virus-associated infectious mononucleosis. J Microbiol Immunol Infect. 2007. 40:216–221.
6. Teramura T, Tabata Y, Yagi T, Morimoto A, Hibi S, Imashuku S. Quantitative analysis of cell-free Epstein-Barr virus genome copy number in patients with EBV-associated hemophagocytic lymphohistiocytosis. Leuk Lymphoma. 2002. 43:173–179.

7. Kasztelewicz B, Jankowska I, Pawlowska J, Teisseyre J, Grenda R, Pronicki M, et al. Epstein-Barr virus DNA load in peripheral blood mononuclear cells and whole blood from pediatric transplant recipients. Transpl Infect Dis. 2011. 13:471–479.

8. Baek SH, Kim SY, Koh H. Effect of reactivation of latent Epstein-Barr virus using polymerase chain-reaction on acute hepatitis A in children. Korean J Pediatr Gastroenterol Nutr. 2011. 14:59–66.

9. Kimura H, Morita M, Yabuta Y, Kuzushima K, Kato K, Kojima S, et al. Quantitative analysis of Epstein-Barr virus load by using a real-time PCR assay. J Clin Microbiol. 1999. 37:132–136.

10. Markin RS. Manifestations of Epstein-Barr virus-associated disorders in liver. Liver. 1994. 14:1–13.

11. Petrova M, Kamburov V. Epstein-Barr virus: silent companion or causative agent of chronic liver disease? World J Gastroenterol. 2010. 16:4130–4134.

12. Jo DS, Han JH, Kim SY, Kim MS, Yi HK, Lee DY, et al. Changes in the expression of cytokines and apoptosis-related genes in children with infectious mononucleosis. Korean J Pediatr. 2009. 52:1348–1357.

13. Gulley ML, Tang W. Laboratory assays for Epstein-Barr virus-related disease. J Mol Diagn. 2008. 10:279–292.

14. Luderer R, Kok M, Niesters HG, Schuurman R, de Weerdt O, Thijsen SF. Real-time Epstein-Barr virus PCR for the diagnosis of primary EBV infections and EBV reactivation. Mol Diagn. 2005. 9:195–200.

15. Pitetti RD, Laus S, Wadowsky RM. Clinical evaluation of a quantitative real time polymerase chain reaction assay for diagnosis of primary Epstein-Barr virus infection in children. Pediatr Infect Dis J. 2003. 22:736–739.

16. Bauer CC, Aberle SW, Popow-Kraupp T, Kapitan M, Hofmann H, Puchhammer-Stockl E. Serum Epstein-Barr virus DNA load in primary Epstein-Barr virus infection. J Med Virol. 2005. 75:54–58.

17. Maurmann S, Fricke L, Wagner HJ, Schlenke P, Hennig H, Steinhoff J, et al. Molecular parameters for precise diagnosis of asymptomatic Epstein-Barr virus reactivation in healthy carriers. J Clin Microbiol. 2003. 41:5419–5428.

18. Liu Y, Fang Z, Liu L, Yang S, Zhang L. Detection of Epstein-Barr virus DNA in serum or plasma for nasopharyngeal cancer: a meta-analysis. Genet Test Mol Biomarkers. 2011. 15:495–502.

19. Hara S, Hoshino Y, Naitou T, Nagano K, Iwai M, Suzuki K, et al. Association of virus infected-t cell in severe hepatitis caused by primary Epstein-Barr virus infection. J Clin Virol. 2006. 35:250–256.

20. Drebber U, Kasper HU, Krupacz J, Haferkamp K, Kern MA, Steffen HM, et al. The role of Epstein-Barr virus in acute and chronic hepatitis. J Hepatol. 2006. 44:879–885.

21. Cameron B, Bharadwaj M, Burrows J, Fazou C, Wakefield D, Hickie I, et al. Prolonged illness after infectious mononucleosis is associated with altered immunity but not with increased viral load. J Infect Dis. 2006. 193:664–671.

22. Suh N, Liapis H, Misdraji J, Brunt EM, Wang HL. Epstein-Barr virus hepatitis: diagnostic value of in situ hybridization, polymerase chain reaction, and immunohistochemistry on liver biopsy from immunocompetent patients. Am J Surg Pathol. 2007. 31:1403–1409.

23. Yuge A, Kinoshita E, Moriuchi M, Ohno Y, Haga H, Moriuchi H. Persistent hepatitis associated with chronic active Epstein-Barr virus infection. Pediatr Infect Dis J. 2004. 23:74–76.

24. Ma C, Wong CK, Wong BC, Chan KC, Lun SW, Lee N, et al. Cytokine responses in a severe case of glandular fever treated successfully with foscarnet combined with prednisolone and intravenous immunoglobulin. J Med Virol. 2009. 81:99–105.

25. Ghosal R, Lewis KE, Chandramouli S. Infectious mononucleosis complicated by acute hepatitis and myocarditis: a response to corticosteroids. BMJ Case Rep. 2009. published on line 10.1136/bcr.10.2008.1083.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download