Abstract
Background/Aims
The past decades have seen increasing incidence and prevalence of inflammatory bowel disease (IBD) in China. This article aimed to summarize the current status and characteristics of surgical management for IBD in China.
Methods
We searched PubMed, Embase, and Chinese databases from January 1, 1990 to July 1, 2014 for all relevant studies on the surgical treatment IBD in China. Eligible studies with sufficient defined variables were further reviewed for primary and secondary outcome measures.
Results
A total of 74 studies comprising 2,007 subjects with Crohn's disease (CD) and 1,085 subjects with ulcerative colitis (UC) were included. The percentage of CD patients misdiagnosed before surgery, including misdiagnosis as appendicitis or UC, was 50.8%±30.9% (578/1,268). The overall postoperative complication rate was 22.3%±13.0% (267/1,501). For studies of UC, the overall postoperative complication rate was 22.2%±27.9% (176/725). In large research centers (n>50 surgical cases), the rates of emergency operations for CD (P=0.032) and in-hospital mortalities resulting from both CD and UC were much lower than those in smaller research centers (n≤50 surgical cases) (P=0.026 and P <0.001, respectively). Regarding the changes in CD and UC surgery over time, postoperative complications (P=0.045 for CD; P=0.020 for UC) and postoperative in-hospital mortality (P=0.0002 for CD; P=0.0160 for UC) both significantly improved after the year 2010.
Conclusions
The surgical management of IBD in China has improved over time. However, the rates of misdiagnosis and postoperative complications over the past two decades have remained high. Large research centers were found to have relatively better capacity for surgical management than the smaller ones. Higher quality prospective studies are needed in China.
Inflammatory bowel diseases (IBD) including CD and UC, are an important health problem with various incidence rates in different countries and populations.12 The incidence of IBD in Asia including China (1.37 per 100,000) has been increasing in recent decades, indicating its emergence as a global disease. In a recent population-based study across nine countries in the Asia-Pacific region, the incidence of IBD was found to be highest in mainland China.34 It was reported to be 3.14 per 100,000 in Southern China and 1.96 per 100,000 in Central China.56
It is estimated that 70% of patients with CD and 10% to 30% of patients with UC will receive surgical intervention at least once in their lifetime.78 The risk of intestinal surgery among IBD patients has decreased over the past six decades, according to population-based studies.9 However, data on the surgical rates in China are lacking. Over the past two decades, a growing number of retrospective studies on IBD surgery in China have been published, and these have shown large variations in the timing of the operation and the types of surgical procedures performed. In a retrospective study of 43 operations in 168 patients with CD in Changsha, the surgical rate was 25.6%.10 In another retrospective study of 167 patients with CD in Guangzhou, 85 patients (50.9%) underwent operations, but only 20 of 85 patients (23.5%) had the correct preoperative diagnosis of CD.11 In addition, only 3% to 17.9% of patients with UC underwent surgery.1213
Biologic agents for IBD therapy became available in China in 2007, accompanied by the increasing use of immunosuppressants. The impact of these agents on IBD surgery remains unknown.1415 A thorough understanding of the status of IBD surgery in China is important, as this knowledge will allow surgeons to explore disparities in practice patterns across regions in order to achieve better surgical outcomes. The aim of this systematic review was to evaluate the current status and characteristics of surgical management for IBD in China.
We searched PubMed, Embase, MEDLINE, the VIP Chinese Journal Database, China National Knowledge Infrastructure, and Wanfang Database from January 1, 1990 to July 1, 2014 for medical subheadings and key words related to IBD and intestinal surgery. The following were the medical subject heading terms combined with free-text search terms: surgery, resection, bowel resection, small intestine resection, colorectal surgery, ileal pouch-anal anastomosis, colectomy, colon resection, proctectomy, rectal resection, ostomy, ileostomy, and colostomy. We limited the language of the studies to Chinese or English. Additional studies were identified through bibliographies of original articles or review articles.
The standard protocol for article inclusion was based on 61 predefined variables regarding the basic clinical characteristics and in-hospital, procedural, and follow-up data mentioned in a previous review on IBD surgery (Supplementary Table 1).16
Studies that fulfilled the following criteria were included: (1) studies that reported information relevant to the surgical rates or outcomes for CD or UC (open colorectal surgery or laparoscopic surgery); (2) studies that included adult IBD subjects (≥16 years old); (3) population- or hospital-based original research (≥10 patients who underwent surgery); and (4) studies with sufficient data (≥50% of predefined variables). Surgery was defined as either open or laparoscopic bowel resection, with or without formation of a stoma. We excluded studies if they were reviews, conference abstracts or presentations, non-peer-reviewed government reports, or master or doctoral theses. Interventional treatments such as radiological drainage of abscesses or incision and drainage of perianal abscesses were also excluded. When the reports had an overlap (e.g., same authors or institutions), only the most recent or the most complete study was included.
The severity of UC in included studies was defined by the Truelove and Witts score.17 Success of the surgery was defined as achieving smooth process of operation without death or severe complications within 24 hours. Emergency operation was defined as surgery for complications requiring urgent surgical intervention (e.g., acute perforation, sudden hemorrhage, and severe abdominal pain). Misdiagnosis of CD was defined as cases in which subjects underwent surgery for what were presumed to be other conditions/illnesses (e.g., appendicitis, UC, and so forth), but were subsequently confirmed to be CD based on surgical findings and histology. The indications for surgery for CD were bowel obstruction or stricture, perforation, abdominal abscess, internal or external fistula, and recurrent or persistent bleeding with medical intractability. Internal fistula referred to gastric fluid leaks from one part of the intestine to the other where the folds touch. In an external fistula, gastric fluid leaks through the skin.14
The indications for surgery for UC included perforation, toxic megacolon, and bowel obstruction. Studies performed in large centers referred to those with a sample size greater than 50 patients, whereas studies performed in small centers referred to those with sample sizes of equal to or fewer than 50 patients.
Infliximab (IFX) became available in China in 2007 but was not approved for CD treatment until 2008.18 Numerous reports regarding the efficacy of IFX in IBD treatment were published in China after 2010,121920212223 and the use of immunosuppressants has also been increasing. Therefore, the studies were categorized into two groups: studies published before 2010 and those published after 2010.
Three reviewers (Q.Y., Y.Y.Z., and Y.Q.) independently completed data extractions from each study using standard data extraction forms. In addition, the study authors were contacted for missing data. A decision was made by a senior reviewer when disagreements occurred. Predefined criteria were used to determine eligibility for inclusion.
The primary outcome measure was surgical rate. Secondary outcome measures included indications for and success rates of operations, reoperation within 30 days, postoperative complications, and in-hospital mortality.
The available sample size was identified only in studies with required data. The results for each variable were reported as frequencies and percentages, and percentages are presented as means±SD using SPSS 17.0 software (SPSS Inc., Chicago, IL, USA). Medians and interquartile ranges (IQR, 25%–75%) were used when the variables were not normally distributed or skewed. Geographic maps were conducted to evaluate nationwide differences in China. Independent sample t-tests were used for statistical analysis in large versus small centers, and a P-value less than 0.05 was considered statistically significant.
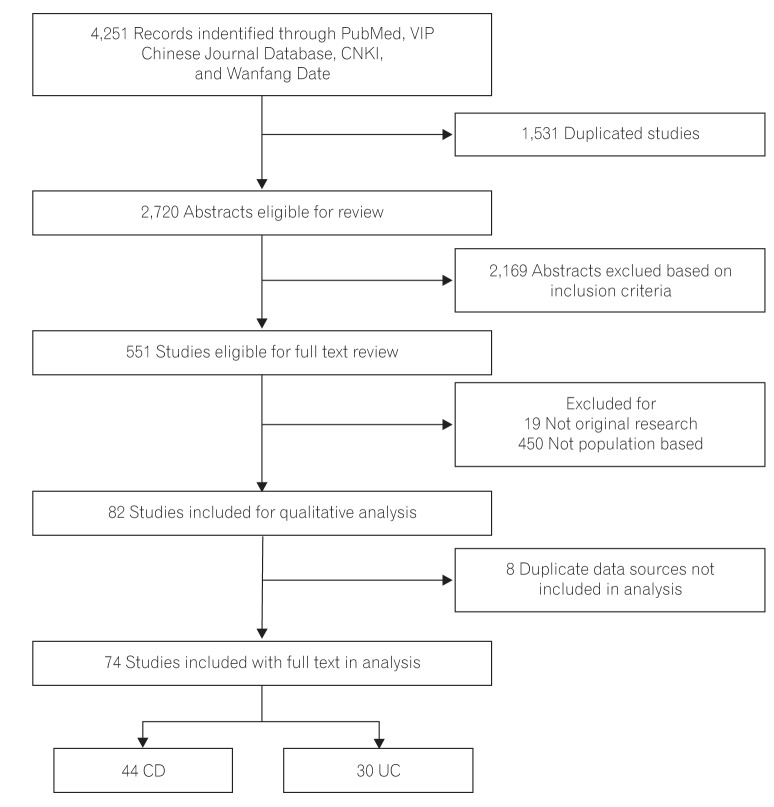
Out of the 4,251 articles identified by the search strategy shown in Fig. 1, 74 studies met our inclusion criteria. Forty-four studies involving 2,007 patients with CD (774 women and 1,233 men), and 30 studies involving 1,085 patients with UC (476 women and 609 men) were included in this study. The average number of subjects across studies examining CD operations was 46 (range, 13–150) and it was 34 for UC operations (range, 11–115). The age of the patients in included studies varied from 16 to 75 years, with average age as 38.8 years for CD patients and 38.4 years for UC patients. The follow-up periods ranged from 30 days to 18 years. The details of these studies are presented in Supplementary Tables 2 and 3. The geographic distributions of the studies are shown in Fig. 2. For CD (n=44), most studies were conducted in South Central China (n=15) and East China (n=21), whereas for UC (n=30), most reported studies were from North (n=7) and East China (n=10).
Overall, 50.8%±30.9% (578/1,268) of patients with CD were diagnosed with uncertainty or misdiagnosed prior to surgery. Among these, 7.5%±8.5% (69/1,268) of the patients with CD were diagnosed with appendicitis before surgery, and 4.3%±7.7% (35/1,268) of the patients were diagnosed with UC before surgery. Other patients were diagnosed with bowel obstruction (19.2%±23.0%), abdominal mass (8.8%±12.2%), or other diseases (11.0%±12.1%), which were also deemed to be indications for surgery. In contrast, misdiagnosis was not reported in cases of UC in included studies (Table 1).
The surgical rate for IBD in China is still unclear. In our analysis, eight studies reported the rate of patients undergoing surgery for CD in their centers, and only three reported the rate for UC; in these studies, the average surgical rates for CD and UC were 56.4%±30.0% (394/756) and 16.4%±5.0% (79/552), respectively. Emergency operations were required in 42.1%±28.7% (235/732) of operations for CD and in 34.5%±23.8% (85/226) for UC. The median number of reoperations within 30 days for CD and UC were 1 and 1, respectively (IQR, 1 and 3.25).
The surgical indications were reported in 36 studies of CD. The three most common indications were bowel obstruction/stricture (40.0%±20.7%), intestinal perforation/fistula (22.7%±20.7%), and abdominal abscess (5.6%±7.1%) (Table 1, Fig. 3A). Other reasons for surgery included intestinal adhesion (4.9%±3.2%), perianal disease (5.5%±1.2%), and dysplasia/cancer (3.9%±1.9%). The surgical indications were reported in 21 studies of UC. The most common indications were failure of medical treatment (52.1%±29.1%), perforation (15.1%±16.9%), massive bleeding (10.3%±13.6%), and toxic megacolon (9.1%±10.8%) (Table 1, Fig. 3B). Other surgical indications included abdominal abscess/sepsis (8.1%±2.2%), colonic dilation (7.9%±2.5%), and dysplasia/cancer (4.3%±3.1%).
The overall in-hospital mortality of surgery for CD was 2.6%±3.4% (26/1,534), while it was 4.0%±6.2% (28/896) for UC (Table 1). The main causes of mortality were severe abdominal infection and multiple organ failure.
As shown in Fig. 4A, the most common operation for CD was partial bowel resection, received by 78.8%±31.3% of patients, followed by colostomy (7.0%±18.2%), ileostomy (3.1%±5.2%), and perforation repair (1.1%±2.5%). Anastomosis and complete examination of the small bowel for additional areas of disease were performed subsequently. The main resection sites were the small bowel (23.4%±22.8%), colon (15.0%±17.0%), and ileocecum (13.0%±19.8%). However, the rate of strictureplasty was low (0.6%±3.3%).
For UC (Fig. 4B), 47.2%±2.5% of patients received total proctocolectomy and ileal pouch-anal anastomosis (TPC-IPAA), followed by TPC and ileoanal anastomosis (24.8%±3.32%), TPC and ileorectal anastomosis (17.7%±23.2%), and pure ileostomy or colostomy (3.6%±0.8%).
Postoperative complications occurred in 22.3%±13.0% of CD patients (267/1,501). Intestinal fistula was the most common complication (6.8%±5.5%), followed by anastomotic leak (5.0%±7.3%) and abdominal infection (3.1%±5.7%) (Fig. 5A). For UC, 22.2%±27.9% of patients (176/725) experienced postoperative complications, among which wound infection (9.2%±1.8%) was the most common, followed by bowel obstruction (3.9%±8.2%) and anastomotic leak (2.6%±4.4%) following pure ileostomy/colostomy or IPAA as a result of infection (Fig. 5B).
The sample size ranged from 12 to 150, with 10 CD studies and six UC studies including more than 50 participants. For CD surgery, the rates of emergency operation (18.6%±13.3% vs. 50.6%±28.3%, P=0.032), reoperation with 30 days (21.1%±2.6% vs. 9.0%±6.3%, P=0.006), and in-hospital mortality (0.7±1.0 vs. 3.1±2.7, P=0.026) were significantly lower in large centers compared with small centers (Table 2). For UC surgery, the rates of postoperative complications (19.4±15.6 vs. 33.7±31.5, P=0.010) and in-hospital mortality within 30 days (0.75±1.5 vs. 4.4±0.1, P <0.001) were much lower in large centers than those in small centers (Table 3). However, there were no significant differences in the success of surgery, surgical rate, rate of disease misdiagnosis, or follow-up mortality between CD and UC.
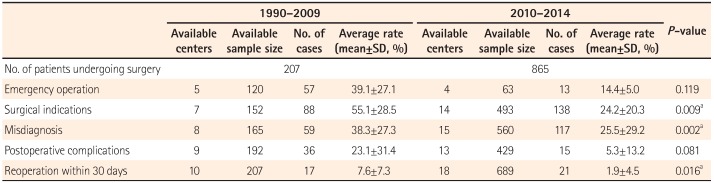
The study periods of the included studies ranged from 1998 to 2014. We divided the time range into studies occurring before and those occurring after 2010, the point at which IFX became available in China, to test whether the availability of IFX and the increasing use of immunosuppressants altered the rate of or complications from surgery. Details regarding the comparison of these two periods are shown in Tables 4 and 5. Seventeen studies including 741 patients undergoing surgery for CD were conducted before 2010, versus 27 studies including 1,266 patients conducted after 2010. Ten studies including 207 patients undergoing surgery for UC were conducted before 2010, whereas 20 studies including 878 patients were performed after 2010. The average sample size of UC significantly increased after 2010 (43.9±32.7 vs. 20.7±7.7, P=0.037). Both the number of studies focusing on patients with IBD undergoing surgery (47 vs. 27) and the number of included patients (2,144 vs. 948) were found to have significantly increased after 2010 compared to the earlier period. Studies reporting surgical data for both surgery for CD and for UC performed after 2010 reported significantly lower in-hospital mortality (P=0.0002 for CD; P=0.016 for UC) than those performed before 2010. After 2010, postoperative complications significantly decreased for both CD (P=0.045) and for UC (P=0.020). However, the rate of misdiagnosis remained high and the surgical rate did not significantly improve after 2010.
An increasing incidence of IBD has been observed in China in recent years, and there are more and more IBD patients receiving operations as an effective treatment.1024 Thus, a large number of clinical reports on IBD surgery have been published in Chinese journals. However, the characteristics of Chinese IBD surgery are not well defined. It remains unclear whether surgical rates and complications differ from those in the West.
The results of the current study showed that more male than female IBD patients received operations. This male sex dominance is in accordance with the prevalence of IBD in the population of China.25 However in Western countries, there is an overall greater prevalence of CD among women compared to men, while there is no sex-based difference in UC.2627 This skewed distribution varies between geographic regions, and it might also reflect the demographic deficit of women as well as different levels of access to healthcare in China. In addition, the average ages of CD patients (38.8 years old) and UC patients (38.4 years old) were very similar, reflecting the fact that most patients in China underwent surgery around the time of middle age. However, these data need to be interpreted cautiously because most included studies only provided age ranges but not detailed information on the ages of the patients, which may increase their heterogeneity.
The collected geographic distribution of IBD operations was partly consistent with previous studies. Our analyses found that more studies on CD surgery were performed in South Central and East China, whereas more studies on UC surgery were performed in North and East China. There are many differences between Northern and Southern China including periods of sunshine, climate, diet (Northern, wheat based food; Southern, rice based food), lifestyle, economic status, and affordable medical service. Ng et al.28 reviewed the geographical variations between countries regarding the etiology of IBD. In Nordic European countries and North American studies, the incidence of UC was higher than that of CD. In France, Norway, and the United States, higher incidence and prevalence of CD were found in the North compared to those in the South.293031 Despite the lack of published studies comparing the incidence and prevalence of CD and UC among different regions of China, a North-South disease gradient might also exist due to differences in environment, genetic predispositions, and socioeconomic factors.
Although IBD is currently a hot topic in China, Chinese clinicians have only begun to become familiar with IBD in the past 5 to 10 years. However, most retrospective studies included in our review were performed in the 1990s, during which time CD patients presenting with acute abdominal pain were easily confused with those suffering from appendicitis, and subsequently underwent operations. The latest epidemiological studies conducted in China also reflected this fact, finding that most CD patients (60%–70%) had ileocolonic disease, but 9% of CD patients had undergone a previous appendectomy.5632 The possible causes of misdiagnosis included low awareness of the differential diagnosis, inadequate radiological and pathological examinations, and a relatively high rate of infections such as intestinal tuberculosis. Moreover, we found that large centers (n>50) and studies performed after 2010 had relatively lower rates of misdiagnosis of CD and lower postoperative complications following surgery for UC, indicating that the diagnostic ability was better in large research centers and improved with time. These findings might be attributed to the development of equipment for diagnosis and the effective coordination of teams from multiple disciplines in large research centers.33 However, the fact that the differences were without significance, implied variation in the included studies. Confirmation of the conclusion will require additional high-quality studies.
Benefiting from the rapid medical technological development in China, Chinese guidelines for the use of IFX for CD therapy were published in 2008 and 2010. Current knowledge has proven that IFX therapy could reduce the need for surgery in patients with IBD.3435 We therefore divided the studies around the initial application of IFX in China; thus the number of studies was balanced for analysis (before/after the year 2010: CD, 17/27; UC, 10/20). However, as there were not sufficient data regarding the use of biologics in the included studies, we did not report the trend.
Based on the results of our analysis, the operation rates for CD and UC were 56.4% and 16.4%, respectively, which were much lower than those reported in the data from Western countries.83637 Some patients in remission did not consent to surgery until complications occurred. Delay optimal timing for surgery and disparities in patients' compliance could explain the low surgical rate in China. Furthermore, only a few of the included studies reported the surgical rate, which would lead to a significant amount of variation and bias.
As described above, the delayed knowledge regarding IBD in China led to a situation in which some patients did not receive prompt medical and surgical treatments. For CD patients, disease complications are varied and occur easily in the form of indications for surgery; that is, patients do not present for surgery until acute and severe complications appear. Thus, cases of medical therapeutic failure are overlapped with the cases of those who had indications for surgery. This is the main reason for the apparently low medical failure rate. Additionally, intestinal stenosis implying bowel obstruction is a major indication for local bowel resection.38 Our data were consistent with that observation, showing that the top three indications for surgery for CD were bowel obstruction/stricture, perforation/fistula, and peritoneal abscess. In the case of UC, perforation, massive bleeding, and toxic megacolon were the top three indications for surgery. However, these findings were not consistent with the conclusion of Han et al.39 in Shanghai, China, that medication resistance and the risk of malignancy were the most frequent indications for surgery for UC in Chinese individuals.
Choosing the correct surgical procedure is of vital importance for disease prognosis. Partial intestinal resection is a traditional type of operational treatment for CD. Our results showed that 79% of patients received partial intestinal resection. However, the extensive resection and reoperation are accompanied by the risk of short gut syndrome. Strictureplasty is an alternative type of surgery in Western countries, used as a more conservative surgical management,40 often for patients with multiple intestinal fibrotic strictures and previous bowel resection.41 The results of our study showed that the rate of strictureplasty in China (0.6%) is less than that in Western countries, the reason may lie in the fact that the timing for operations of patients with IBD in China was relatively late, and there is relatively poor knowledge regarding the surgery technique. IPAA has gradually been accepted as a safe and effective treatment for UC.42 In our study, more than one third of operations were IPAA, but the rate of IPAA differed from 0% to 78% in included studies, with only 20 out of 44 studies reporting it. The large variation implies different competence regarding IPAA in different centers in China. Ileostomy is indicated for UC patients who are at high risk for pouch failure.43
Postoperative complications of IBD are divided into longterm and short-term ones. As the included studies were retrospective without long-term follow-up, the major postoperative complications (CD, 22.3%±13.0%; UC, 22.2%±27.9%) in our results were short-term postoperative complications including wound infection, anastomosis leak, and obstruction. The high rate of complications may in part be accounted for by the low rate of stoma formation. However, the rates are still lower than those of Western countries. In the reports of Western countries, pelvic sepsis is the most serious early complication of UC surgery (20%), followed by bowel obstruction (30% at 10 years) and anastomotic strictures (8%–14% at 10 years).444546 With improvement in medical treatment, the risk of surgery for IBD has decreased.9 Indications for IFX have increased in the United States, and the response to IFX could reduce the rates of colectomy.47 A large number of publications reporting the efficacy of IFX in IBD have been published in China since 2010. However, the impact of IFX on surgery remains unclear. Our data showed that the sample size of studies after 2010 was significant larger than that of studies before 2010. Postoperative complications and mortality decreased significantly for both CD and UC after 2010. However, there were no significant differences in surgical rate, emergency rate, or reoperation rate. These improvements may benefit from advances in medicine and technique, as well as increased knowledge of the IBD disease process on the part of physicians.
Our study has certain limitations. First, patients were selected from retrospective observational studies rather than population-based studies, which may have increased the heterogeneity and underestimated the measures of outcomes. We performed subgroup analysis to reduce this heterogeneity. Second, as most of the studies we selected were from developed regions within urban areas in China, the conclusions may not represent the incidence and prevalence of IBD outside urban areas of China. Third, some of the included studies did not provide disease duration and longterm follow-up data. Therefore, further prospective studies with long-term follow-up are urgently needed.
In conclusion, the surgical management of IBD in China has improved over time. However, the rate of operations was lower than that in Western countries, and the rates of misdiagnosis and postoperative complications over the past two decades have remained high, especially in CD patients. Higher quality prospective studies are needed in China to provide information on the surgical rate and guidance regarding surgical indications for and approaches to IBD.
Notes
References
2. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54.e42. PMID: 22001864.

3. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn's and colitis epidemiology study. Gastroenterology. 2013; 145:158–165.e2. PMID: 23583432.

4. Ouyang Q, Wang YF, Hu RW. Epidemiology of inflammatory bowel disease in China. Chung Hua Hsiao Hua Tsa Chih. 2008; 28:814–818.

5. Zeng Z, Zhu Z, Yang Y, et al. Incidence and clinical characteristics of inflammatory bowel disease in a developed region of Guangdong province, China: a prospective population-based study. J Gastroenterol Hepatol. 2013; 28:1148–1153. PMID: 23432198.

6. Zhao J, Ng SC, Lei Y, et al. First prospective, population-based inflammatory bowel disease incidence study in mainland of China: the emergence of "Western" disease. Inflamm Bowel Dis. 2013; 19:1839–1845. PMID: 23669403.
7. Dignass A, Lindsay JO, Sturm A, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 2: current management. J Crohns Colitis. 2012; 6:991–1030. PMID: 23040451.

8. Rutgeerts P, Geboes K, Vantrappen G, Kerremans R, Coenegrachts JL, Coremans G. Natural history of recurrent Crohn's disease at the ileocolonic anastomosis after curative surgery. Gut. 1984; 25:665–672. PMID: 6735250.

9. Frolkis AD, Dykeman J, Negrón ME, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013; 145:996–1006. PMID: 23896172.

10. Li XF, Lu FG, Zou YY, Ouyang CH, Ye LJ, Wang ZG. Analysis of clinical characteristics of 43 surgical patients with Crohn disease using the Montreal classification. Zhonghua Wei Chang Wai Ke Za Zhi. 2010; 13:210–212. PMID: 20336541.
11. Zhou J, Wang JP, Wang J, et al. Analysis of surgical treatment of Crohn's disease: a report of 85 cases. Chin J Pract Surg. 2007; 27:211–213.
12. Pan Y, Ouyang Q, Hu RW. Analysis of surgical treatment for severe ulcerative colitis. Zhonghua Wei Chang Wai Ke Za Zhi. 2010; 13:430–432. PMID: 20577922.
13. Inflammatory Bowel Disease Cooperation Group of China. Wang YF, Ouyang Q. A retrospective study of 3100 inpatients with ulcerative colitis in China. Chung Hua Hsiao Hua Tsa Chih. 2006; 26:368–372.
14. Bernstein CN, Loftus EV Jr, Ng SC, Lakatos PL, Moum B. Epidemiology and Natural History Task Force of the International Organization for the Study of Inflammatory Bowel Disease (IOIBD). Hospitalisations and surgery in Crohn's disease. Gut. 2012; 61:622–629. PMID: 22267595.

15. Gao X, Yang RP, Chen MH, et al. Risk factors for surgery and postoperative recurrence: analysis of a south China cohort with Crohn's disease. Scand J Gastroenterol. 2012; 47:1181–1191. PMID: 22845663.

16. Peyrin-Biroulet L, Harmsen WS, Tremaine WJ, Zinsmeister AR, Sandborn WJ, Loftus EV Jr. Surgery in a population-based cohort of Crohn's disease from Olmsted County, Minnesota (1970-2004). Am J Gastroenterol. 2012; 107:1693–1701. PMID: 22945286.

17. Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955; 2:1041–1048. PMID: 13260656.
18. Inflammatory Bowel Disease Cooperation Group of China. Recommendation of inflixmab treatment for Crohn's disease. Chung Hua Hsiao Hua Tsa Chih. 2008; 28:847–849.
19. Li SR, Lu XJ, Sheng JQ, Fan J, Li S, Zhao X. Comparison of the treating effects of infliximab in Crohn's disease and ulcerative colitis. Weichangbingxue He Ganbingxue Zazhi. 2010; 19:644–647.
20. Sun YY, Wu YF, Xu C, et al. Efficacy of infliximab in treatment of patients with Crohn's disease. Acad J Second Mil Med Univ. 2010; 31:338–339.

21. Wang YJ, Li ZY, Sun L, Peng Q, Liu L. Clinical observation for the combination of intestinal probiotics and infliximab in treatment of refractory Crohn's disease. China Mod Dr. 2010; (22):119.
22. Wu DP, Zheng P. Efficacy infliximab of treatment in 11 patients with Crohn's disease. Int J Dig Dis. 2010; 30:314–318.
23. Zhou AC, Jin HY. Application of infliximab in treating Crohn's disease. Med Recapitulate. 2010; 16:3786–3788.
24. Leong RW, Lau JY, Sung JJ. The epidemiology and phenotype of Crohn's disease in the Chinese population. Inflamm Bowel Dis. 2004; 10:646–651. PMID: 15472528.

25. Jiang L, Xia B, Li J, et al. Retrospective survey of 452 patients with inflammatory bowel disease in Wuhan city, central China. Inflamm Bowel Dis. 2006; 12:212–217. PMID: 16534423.

26. Brant SR, Nguyen GC. Is there a gender difference in the prevalence of Crohn's disease or ulcerative colitis? Inflamm Bowel Dis. 2008; 14(Suppl 2):S2–S3. PMID: 18816735.

27. Bernstein CN, Blanchard JF, Rawsthorne P, Wajda A. Epidemiology of Crohn's disease and ulcerative colitis in a central Canadian province: a population-based study. Am J Epidemiol. 1999; 149:916–924. PMID: 10342800.

28. Ng SC, Bernstein CN, Vatn MH, et al. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013; 62:630–649. PMID: 23335431.

29. Vind I, Riis L, Jess T, et al. Increasing incidences of inflammatory bowel disease and decreasing surgery rates in Copenhagen City and County, 2003-2005: a population-based study from the Danish Crohn colitis database. Am J Gastroenterol. 2006; 101:1274–1282. PMID: 16771949.

30. Moum B, Vatn MH, Ekbom A, et al. Incidence of ulcerative colitis and indeterminate colitis in four counties of southeastern Norway, 1990-93: a prospective population-based study: the Inflammatory Bowel South-Eastern Norway (IBSEN) Study Group of gastroenterologists. Scand J Gastroenterol. 1996; 31:362–366. PMID: 8726304.

31. Lehtinen P, Ashorn M, Iltanen S, et al. Incidence trends of pediatric inflammatory bowel disease in Finland, 1987-2003, a nationwide study. Inflamm Bowel Dis. 2011; 17:1778–1783. PMID: 21744433.

32. Yang H, Li Y, Wu W, et al. The incidence of inflammatory bowel disease in Northern China: a prospective population-based study. PLoS One. 2014; 9:e101296. DOI: 10.1371/journal.pone.0101296. PMID: 25029440.

33. Infections Bowel. The consensus on diagnosis and management of inflammatory bowel disease (2012 Guangzhou). Chin J Gastroenterol. 2012; (12):763–781.
34. Rungoe C, Langholz E, Andersson M, et al. Changes in medical treatment and surgery rates in inflammatory bowel disease: a nationwide cohort study 1979-2011. Gut. 2014; 63:1607–1616. PMID: 24056767.

35. Clemente V, Aratari A, Papi C, Vernia P. Short term colectomy rate and mortality for severe ulcerative colitis in the last 40 years: has something changed? Dig Liver Dis. 2016; 48:371–375. PMID: 26854257.

36. Caprilli R, Viscido A, Latella G. Current management of severe ulcerative colitis. Nat Clin Pract Gastroenterol Hepatol. 2007; 4:92–101. PMID: 17268544.

37. Bernell O, Lapidus A, Hellers G. Risk factors for surgery and recurrence in 907 patients with primary ileocaecal Crohn's disease. Br J Surg. 2000; 87:1697–1701. PMID: 11122187.

38. Michelassi F, Melis M, Rubin M, Hurst RD. Surgical treatment of anorectal complications in Crohn's disease. Surgery. 2000; 128:597–603. PMID: 11015093.

39. Han Y, Lin MB, He YG, et al. Laparoscopic surgery for inflammmatory bowel disease: the experience in China. J Invest Surg. 2013; 26:180–185. PMID: 23514051.

40. Fazio VW, Marchetti F. Recurrent Crohn's disease and resection margins: bigger is not better. Adv Surg. 1999; 32:135–168. PMID: 9891742.
41. Dietz DW, Laureti S, Strong SA, et al. Safety and longterm efficacy of strictureplasty in 314 patients with obstructing small bowel Crohn's disease. J Am Coll Surg. 2001; 192:330–337. PMID: 11245375.

42. Cohen JL, Strong SA, Hyman NH, et al. Practice parameters for the surgical treatment of ulcerative colitis. Dis Colon Rectum. 2005; 48:1997–2009. PMID: 16258712.

43. Camilleri-Brennan J, Munro A, Steele RJ. Does an ileoanal pouch offer a better quality of life than a permanent ileostomy for patients with ulcerative colitis? J Gastrointest Surg. 2003; 7:814–819. PMID: 13129563.

44. MacLean AR, Cohen Z, MacRae HM, et al. Risk of small bowel obstruction after the ileal pouch-anal anastomosis. Ann Surg. 2002; 235:200–206. PMID: 11807359.

45. Heuschen UA, Hinz U, Allemeyer EH, et al. Risk factors for ileoanal J pouch-related septic complications in ulcerative colitis and familial adenomatous polyposis. Ann Surg. 2002; 235:207–216. PMID: 11807360.

46. Galandiuk S, Scott NA, Dozois RR, et al. Ileal pouch-anal anastomosis: reoperation for pouch-related complications. Ann Surg. 1990; 212:446–452. PMID: 2171442.
47. Oussalah A, Evesque L, Laharie D, et al. A multicenter experience with infliximab for ulcerative colitis: outcomes and predictors of response, optimization, colectomy, and hospitalization. Am J Gastroenterol. 2010; 105:2617–2625. PMID: 20736936.

Fig. 2
Geographic distribution of studies. All 74 studies were independently performed between 1998 and 2014. One red dot stands for one CD study (n=44 in total), and one blue dot stands for one UC study (n=30 in total).
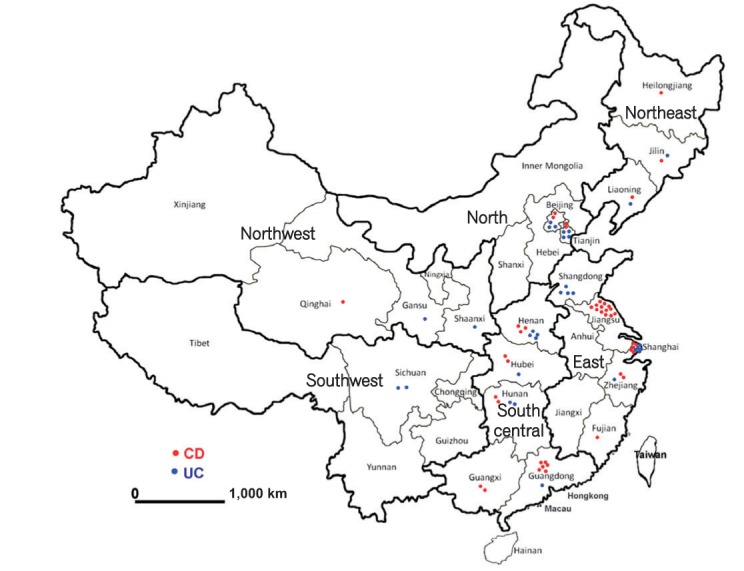
Fig. 3
Surgical indications for IBD in China. (A) Surgical indications for CD. Bowel obstruction/stricture, perforation/fistula, and abdominal abscess were the three most common indications. (B) Surgical indications for UC. Failure of medical therapy, perforation, massive bleeding, and toxic megacolon were the most common indications.
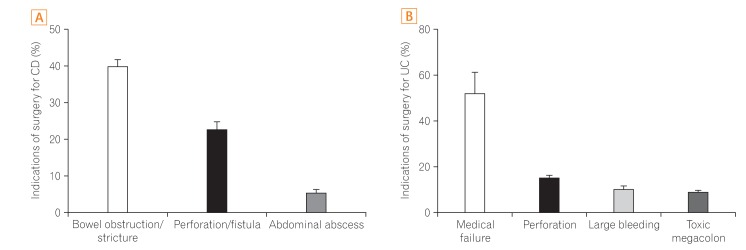
Fig. 4
Type of operation for IBD. (A) Type of operation for CD. (B) Type of operation for UC. TPC, total proctocolectomy; IPAA, ileal pouch-anal anastomosis; IAA, ileoanal anastomosis; IRA, ileorectal anastomosis; IL, ileostomy; CL, colostomy.
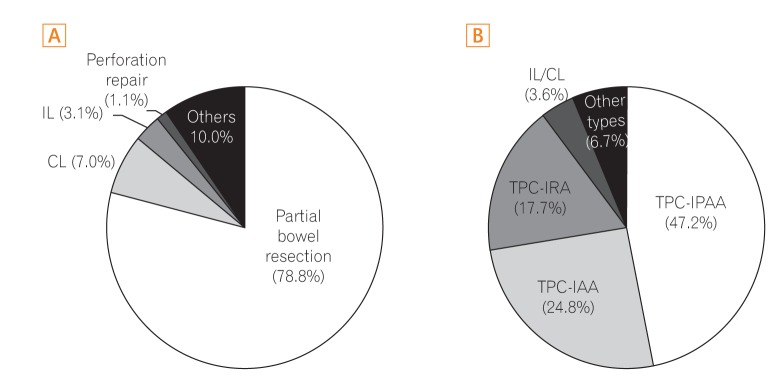
Fig. 5
Postoperative complications of IBD in China. (A) Postoperative complications of CD. Abdominal infection, anastomotic leak, and intestinal fistula were the most common complications. (B) Postoperative complications of UC. Wound infection, anastomotic leak, and bowel obstruction were the most common complication.
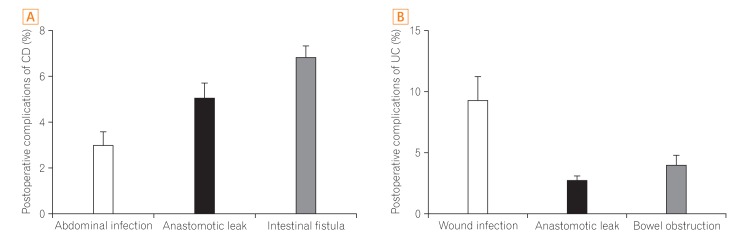
Table 1
In-Hospital Data for CD and UC Operations
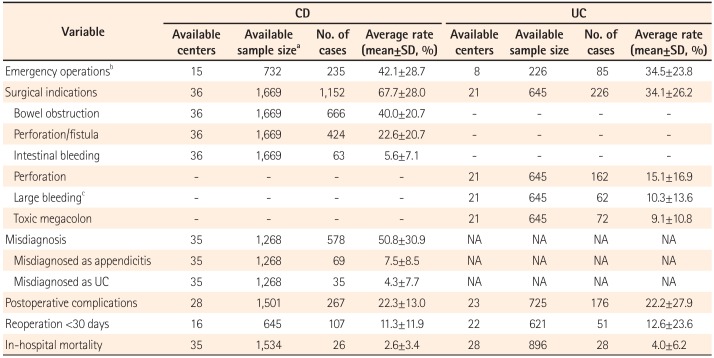
aThe number of available centers and available sample size refers to the studies that have reported required variables.
bEmergency operations were defined as surgeries performed because of urgent situations or severe complications of IBD.
cMassive bleeding was defined as blood loss exceeding 1,000 mL.
NA, not applicable.
Table 2
Comparison between Large and Small Centers Performing CD Operations
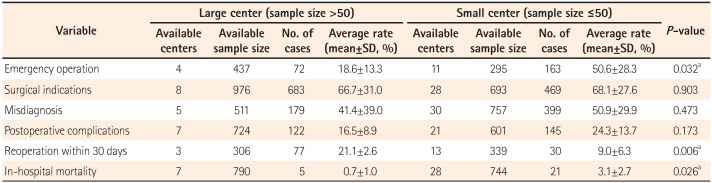
Table 3
Comparison between Large and Small Centers Performing UC Operations
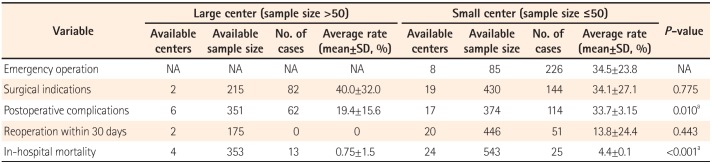
Table 4
Comparison of CD Operations in China before and after the Year 2010
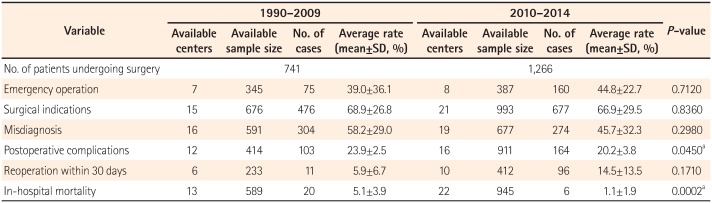
Table 5
Comparison of UC Operations in China before and after the Year 2010




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download