Abstract
Background/Aims
The quality of care in inflammatory bowel disease (IBD) has not been systematically estimated. The aim of this study was to investigate the current status of quality of IBD care in Asian countries.
Methods
A questionnaire-based survey was conducted between March 2014 and May 2014. The questionnaire was adopted from "An adult inflammatory bowel disease physician performance measure set" developed by the American Gastroenterological Association. If the respondent executed the performance measure in more than 70% of patients, the measure was regarded as well performed.
Results
A total of 353 medical doctors from Asia completed the survey (116 from Korea, 114 from China, 88 from Japan, 17 from Taiwan, 8 from Hong-Kong, 4 from India, 3 from Singapore, and 1 each from the Philippines, Malaysia and Indonesia). The delivery of performance measures, however, varied among countries. The documentation of IBD and tuberculosis screening before anti-tumor necrosis factor therapy were consistently performed well, while pneumococcal immunization and prophylaxis of venous thromboembolisms in hospitalized patients were performed less frequently in all countries. Physician awareness was positively associated with the delivery of performance measures. Variations were also noted in reasons for non-performance or low performance of quality measures, and the two primary reasons cited were consideration of the measure to be unimportant and lack of time.
Inflammatory bowel diseases (IBD) are a chronic gastrointestinal disease with a significant burden of illness.12 In addition to significant economic and health costs, treatments for IBD are variable, and it is of increasing concern that many patients continue to receive sub-optimal care.34 Associative pathologies, such as CD and UC, can also have variable courses of disease progression. This heterogeneity makes it difficult to implement generally effective strategies, and consequently contributes to considerable variation in IBD care.5 However, standardized processes for care are essential to improve quality of care.6 In 2011, the American Gastroenterological Association (AGA) developed "An adult inflammatory bowel disease physician performance measures set" that comprised 10 specific measures. Eight of these measures were subsequently included in the Centers for Medicare and Medicaid Physician Quality Reporting System in 2012.7 As the incidence and prevalence of IBD has increased rapidly in Asia, quality of care is emerging as an important aspect of IBD care in Asia.8910 The current quality of care status for IBD has, however, not been systematically investigated in Asia. In this study, we performed a questionnaire-based survey to evaluate the delivery of performance measures for IBD care in the current Asian practice.
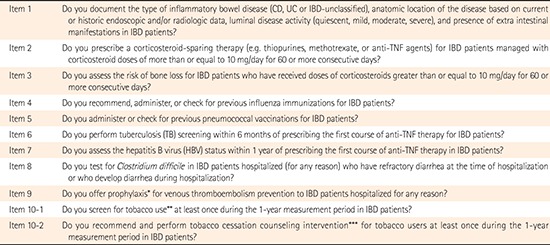
The questionnaire-based survey was designed by the organizing committee of the Asian Organization of Crohn's and Colitis (AOCC) and reviewed by staff officer members of the organization. The questionnaire comprised 11 questions, adopted from "An adult inflammatory bowel disease physician performance measure set" developed by the AGA. Details of the questionnaire are provided in the Appendix. A multinational web-based survey was conducted between March 2014 and May 2014 by the IBD study group of the Korean Association for the Study of Intestinal Diseases (KASID). Physicians involved with IBD treatment at major institutions in Asian countries were invited by e-mail to participate in the survey. The delivery of each performance measure was assessed based on a five–point Likert scale: always (responder performed the measure in 90%–100% of patients), usually (70%–90% of patients), sometimes (30%–70% of patients), rarely (10%–30% of patients) and never (0%–10% of patients), and a descriptive analysis of responses was conducted. The respondent was regarded to deliver a performance measure well if it was performed in more than 70% of patients. Categorical variables were analyzed by the χ2 or Fisher's exact test. P-values <0.05 were considered significant and based on two-sided tests.
A total of 353 Asian doctors (28.9% women) from various countries (Korea 116, China 114, Japan 88, Taiwan 17, Hong-Kong 8, India 4, and Singapore 3, the Philippines 1, Malaysia 1 and Indonesia 1) completed the survey. Of these respondents, 54% (n=190) were IBD specialists and a majority of the respondents served at academic teaching hospitals (n=336, 95.2%). About the number of years of experience with IBD treatment, 43.3% (n=153) indicated having more than 10 years of experience. Considering country-specific characteristics, 61.4% (n=54, P<0.001) of Japanese respondents indicated more than 10 years of experience in IBD treatment, and 56.1% (n=64, P<0.001) of the Chinese respondents were women.
Seven of the 11 performance measures were executed well by more than 70% of respondents in Asian Countries. Tuberculosis (TB) screening before anti-tumor necrosis factor (TNF) therapy and documentation of IBD were consistently among the highest ranked measures, whereas pneumococcal immunization and prophylaxis of venous thromboembolisms (VTEs) in hospitalized patients were repetitively the lowest ranked in all countries. However, the delivery of performance measures varied among countries (Fig. 1).
In comparison to other countries, a higher proportion of Chinese respondents performed well considering tobacco cessation interventions (89.4%) and prophylaxis for VTEs in hospitalized patients (36.8%), while a lower proportion of respondents performed well considering testing for Clostridium difficile in hospitalized patients with diarrhea (71.1%). In Korea, a higher proportion of respondents performed well in administering corticosteroid sparing therapy (94.8%), testing for C. difficile in hospitalized patients with diarrhea (92.2%), influenza immunizations (75.9%), and pneumococcal immunizations (64.7%), while a lower proportion performed well considering HBV screening before anti-TNF therapy (84.5%), bone loss assessment in patients with high dose corticosteroid (63.8%), and prophylaxis for VTEs in hospitalized patients (19.0%).
A higher proportion of Japanese respondents performed well in HBV screening before anti-TNF therapy (97.7%), and bone loss assessment in patients with high dose corticosteroids (86.4%), while a lower proportion performed well considering tobacco cessation interventions (63.6%) and pneumococcal immunizations (17.0%). Among the other Asian countries, the lowest proportion of respondents performed well in influenza vaccination (42.9%). Overall, the performance of pneumococcal and influenza immunization showed profound variations among Asian countries (China 36.1%, Korea 64.7%, Japan 17.0%, others 28.6%, P=0.00). For the screening of latent TB, interferon-γ release assay was commonly used in China (47.4%), Japan (65.9%), and the other Asian countries (48.6%), while the combination of a tuberculin skin test and interferon-γ release assay was preferred in Korea (51.3%). When the tuberculin skin test was used, a majority of respondents regarded it as positive if the diameter of induration was greater than 10 mm in IBD patients with or without risk factors.
Seven of the 11 performance measures were recognized as performance measures by more than 70% of respondents in Asian Countries. Awareness of prophylaxis of VTEs in hospitalized patients belonged to the lowest ranks in all countries. Pneumococcal and influenza immunization were the second and third lowest ranked in Asian countries, except Korea. Awareness of performance measures was diverse between countries (Fig. 1). Overall, respondents from Japan showed lower awareness than respondents from other countries did. Awareness of pneumococcal immunization had the biggest difference between countries (Korea 72.4% vs. Japan 39.8%). On the other hand, awareness of influenza immunization presented the smallest difference (Korea 60% vs. Japan 48.9%).
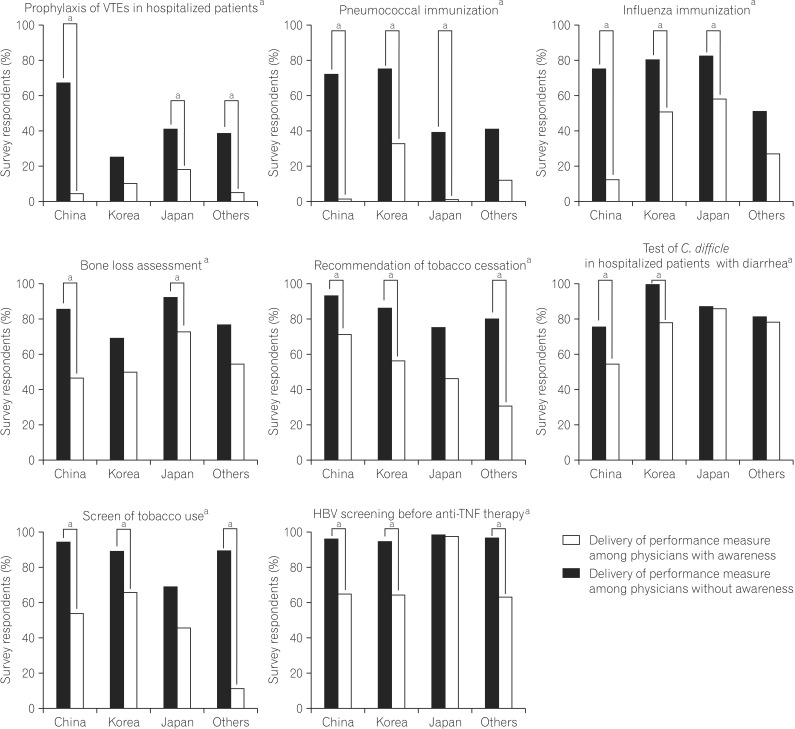
The delivery of performance measures was better than awareness among performance measures with higher ranks. Japanese respondents showed lower awareness than the other countries did, although the overall performance was not low. Awareness was better about prophylaxis of VTEs and pneumococcal immunization in all Asian countries (Fig. 1). In addition, awareness had a positive association with the delivery of performance measures, especially in performance measures with lower delivery. However, the association between the awareness and delivery of performance measures varied among countries (Fig. 2). Delivery of performance measures according to awareness was not statically different in TB screening before anti-TNF therapy, documentation of IBD, and corticosteroid sparing therapy.
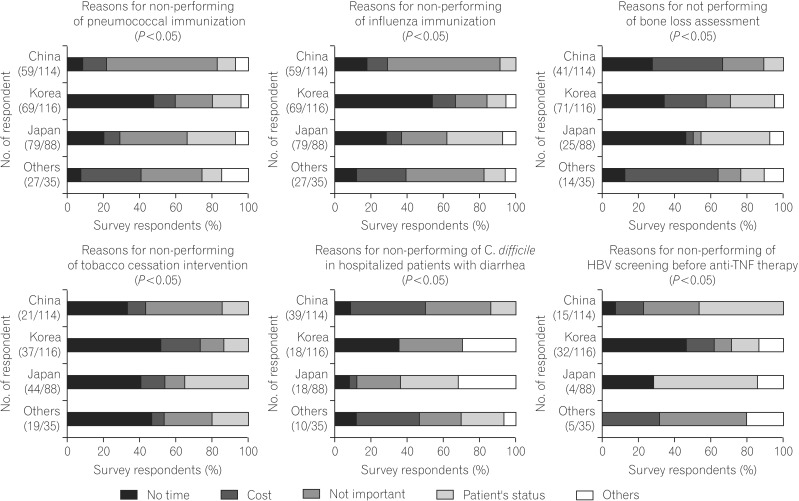
In prophylaxis of VTEs, the main reason for non-performance was the consideration that this form of treatment was unimportant, and did not differ among Asian countries. Reasons for non-performance considering lower ranked performance measures varied among Asian countries (Fig. 3). About pneumococcal and influenza vaccination, considering this to be unimportant was the main reason in most countries, while lack of time was the main reason in Korea. Regarding bone loss assessment with high dose corticosteroids and the C. difficile test in hospitalized patients with diarrhea, cost was the main reason in China and other Asian Countries. A significant variation was also found in reasons cited for non-performance of HBV screening before anti-TNF therapy, although overall this measure was performed well. The main reason in China and Japan was cited as the status of patients (complications, contraindications, among others), lack of time in Korea, and cost and considering it as unimportant in other Asian countries. A notable variation was not found among countries for the reasons for non-performance considering performance measures with higher ranks. The main reason was lack of time in screening use of tobacco and documentation of IBD, while it was the status of patient in corticosteroid sparing therapy and cost in TB screening.
To the best of our knowledge, this study is the first to assess the delivery of performance measures for IBD treatment in Asian countries. The study population was gastroenterologists with significant expertise in IBD treatment in Asian countries.
We found considerable variation in the delivery of performance measures among Asian countries. Measures with a consistently high rank in delivery among all countries included testing for latent TB before the initiation of anti-TNF therapy, and the documentation of IBD. Currently, there is limited data about the delivery of performance measures in Western countries. In a recent study from a tertiary care center in the USA,11 compliance of testing for latent TB was 67%, ranked fifth among 8 measures for outpatient care, and compliance of documentation of IBD was 70%, and ranked fourth. A recent European study demonstrated a marked increase in TB screening before initiating anti-TNF therapy from 30% in 2003 to 97% in 2010. A similar adherence with these measures in Asian countries was not unexpected in this study as many of the countries included in the survey (China, Korea, India, the Philippines, Malaysia, and Indonesia) are TB endemic areas, and TB screening is an elementary component in the management of IBD.12 Lower ranked performance measures among Asian countries, including prophylaxis of VTEs, and pneumococcal and influenza vaccination were comparable to a similarly lower compliance in Western contries.11131415
Recent Western survey data suggests that the rates of pharmacologic prophylaxis of VTEs in hospitalized patients with IBD is less than 40%.1316 Despite reasonable awareness of the increased risk of thrombosis in hospitalized IBD patients, many physicians do not follow clinical practice guidelines, and prophylaxis for VTEs are underutilized.16 In this study, only 24% of respondents from Asian countries performed well considering prophylaxis for VTEs. A recent systematic review explained the reason for lower delivery of this measure in Asian countries as a lower demonstrated risk of VTE in Asian general surgery patients, even in patients at high risk.17 However, there is limited data about risk of VTEs in Asian IBD patients,18 and there is currently a need for consensus among Asian countries about prophylaxis for VTEs based on clinical data from Asian IBD patients.
The awareness of quality measures has been regarded as an important factor in performance,11121319202122 and in the present study, there was a positive association between awareness and delivery of performance measures among Asian countries. However, performance measures such as IBD documentation and TB screening before anti-TNF therapy were not affected significantly, as respondents implemented these measures without awareness. This result indicates that the dissemination, transfer of knowledge, and change of attitude towards documentation of IBD, and TB screening before anti-TNF therapy may have already occurred among Asian doctors.15 Nevertheless, further education regarding the impact of performance measures in IBD patients is needed among Asian countries.
Reasons for non-performance varied among countries especially for lower ranked performance measures. The Asian countries included in our study differ markedly in their demography, country income classification, and economic resources allocated for healthcare.23 These factors could influence the differences observed in the delivery of performance measures. For example, respondents from other Asian countries indicated that cost was the main barrier for bone loss assessment in patients on high doses of corticosteroids. Dual-energy x-ray absorptiometry (DXA) is the gold standard for bone loss assessment. However, it is relatively expensive and not widely available in most developing countries. In areas without reimbursement, the cost of DXA is often prohibitively high for the average wage earner. On the other hand, Asian countries like Japan, Singapore, and Korea have better developed systems easily available for DXA.24
The majority of respondents indicated a lack of time or that they did not consider vaccination to be important in IBD care. Studies have shown that knowledge about available vaccinations that could be recommend for IBD patients is poor.202225 A lack in the availability of incidence data may also influence unawareness and knowledge deficiency among physicians in Asia. For example, limited data are available regarding the burden and epidemiology of pneumococcal disease in adults, particularly in Asia.26 There are also, to the best of our knowledge, no English-language articles published on the incidence of pneumococcal disease in adults in China, India, Indonesia, Japan, the Philippines, and Korea. Five countries (Indonesia, Malaysia, Singapore, Thailand, and Vietnam) have guidelines for influenza vaccination but only two are consistent with global guidelines,23 and the rate of vaccination in Asian countries continues to remain low. Educational programs on vaccinations, tailored towards gastroenterologists who care for patients with IBD, are therefore still needed.
The present study, however, also has several limitations that must be considered. The survey investigated the delivery of performance measures in each country by relying on the physician's memory recall, and therefore, this does not accurately reflect the performance of each country. While several studies have examined the magnitude of parental recall or patient's recall bias for immunization status,27 few studies have looked at the validity of recall in physicians. The self-reporting of influenza and pneumococcal vaccines was highly sensitive and moderately specific in elderly adults when compared with medical records. Even if we might assume that physicians would have better recall than patients would, further study based on medical records is still needed.
Another aspect for consideration is the differing characteristics of the study respondents between countries. Japanese respondents collectively had more respondents with a significant number of years of experience with IBD care and the Chinese respondent sample had more women respondents. The delivery of a few performance measures indicated significant differences that were dependent on these characteristics. It is however difficult to ascertain whether these differences could be attributed to the characteristics of the respondents surveyed or a sampling bias, as the characteristics of the total population of physicians who treat IBD in each country is not known.
Respondents from Korea had a tendency to select "lack of time" as the reason for non-performance while respondents from Japan frequently selected "the status of patients". Culture is a consistently significant factor in predicting an individual's social question-and-answer behavior.28 Because the study questionnaire was composed of exclusive choice questions, other possible reasons for non-performance could be masked by answer selection based on cultural influences. In addition, the response rate of questions for reasons for non-performance was very low in performance measures with high adherence. Therefore, the validity of those values is also contestable.
In conclusion, a notable variation was found in the delivery of performance measures among Asian countries. To reach a consensus in physician performance measures reflecting differences in Asian IBD patients, we must understand and decrease this variation among Asian countries. Local data on disease burden, cost effectiveness, acceptability, coverage, and delivery strategies are needed to inform the development and implementation of performance measures. The AOCC needs to play an important role to ensure consistency in the level of care across different national settings.
References
1. Kappelman MD, Rifas-Shiman SL, Porter CQ, et al. Direct health care costs of Crohn’s disease and ulcerative colitis in US children and adults. Gastroenterology. 2008; 135:1907–1913. PMID: 18854185.

2. Longobardi T, Jacobs P, Bernstein CN. Utilization of health care resources by individuals with inflammatory bowel disease in the United States: a profile of time since diagnosis. Am J Gastroenterol. 2004; 99:650–655. PMID: 15089897.

3. Bodger K. Cost effectiveness of treatments for inflammatory bowel disease. Pharmacoeconomics. 2011; 29:387–401. PMID: 21271748.

4. David G, Gunnarsson C, Lofland JH. Variations in care: a retrospective database analysis of healthcare utilization patterns for patients with inflammatory bowel disease. J Med Econ. 2015; 18:137–144. PMID: 25335098.

5. Kappelman MD, Palmer L, Boyle BM, Rubin DT. Quality of care in inflammatory bowel disease: a review and discussion. Inflamm Bowel Dis. 2010; 16:125–133. PMID: 19572335.

6. Crandall WV, Boyle BM, Colletti RB, Margolis PA, Kappelman MD. Development of process and outcome measures for improvement: lessons learned in a quality improvement collaborative for pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2011; 17:2184–2191. PMID: 21456033.

7. Melmed GY, Siegel CA. Quality improvement in inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2013; 9:286–292. PMID: 23943663.
8. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54. PMID: 22001864.

9. Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280. PMID: 22497584.

10. Ahuja V, Tandon RK. Inflammatory bowel disease in the Asia-Pacific area: a comparison with developed countries and regional differences. J Dig Dis. 2010; 11:134–147. PMID: 20579217.

11. Feuerstein JD, Lewandowski JJ, Martinez-Vazquez M, Leffler DA, Cheifetz AS. Documented compliance with inflammatory bowel disease quality measures is poor. Dig Dis Sci. 2015; 60:339–344. PMID: 25311583.

12. Stille CJ, Jerant A, Bell D, Meltzer D, Elmore JG. Coordinating care across diseases, settings, and clinicians: a key role for the generalist in practice. Ann Intern Med. 2005; 142:700–708. PMID: 15838089.

13. Tinsley A, Naymagon S, Trindade AJ, Sachar DB, Sands BE, Ullman TA. A survey of current practice of venous thromboembolism prophylaxis in hospitalized inflammatory bowel disease patients in the United States. J Clin Gastroenterol. 2013; 47:e1–e6. PMID: 22476043.

14. Wasan SK, Calderwood AH, Long MD, Kappelman MD, Sandler RS, Farraye FA. Immunization rates and vaccine beliefs among patients with inflammatory bowel disease: an opportunity for improvement. Inflamm Bowel Dis. 2014; 20:246–250. PMID: 24374881.

15. Walsh AJ, Weltman M, Burger D, et al. Implementing guidelines on the prevention of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2013; 7:e449–e456. PMID: 23601754.

16. Sam JJ, Bernstein CN, Razik R, Thanabalan R, Nguyen GC. Physicians’ perceptions of risks and practices in venous thromboembolism prophylaxis in inflammatory bowel disease. Dig Dis Sci. 2013; 58:46–52. PMID: 23053902.

17. Yeo DX, Junnarkar S, Balasubramaniam S, et al. Incidence of venous thromboembolism and its pharmacological prophylaxis in Asian general surgery patients: a systematic review. World J Surg. 2015; 39:150–157. PMID: 25189450.

18. Sonoda K, Ikeda S, Mizuta Y, Miyahara Y, Kohno S. Evaluation of venous thromboembolism and coagulation-fibrinolysis markers in Japanese patients with inflammatory bowel disease. J Gastroenterol. 2004; 39:948–954. PMID: 15549447.

19. Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005; 142:260–273. PMID: 15710959.

20. Yeung JH, Goodman KJ, Fedorak RN. Inadequate knowledge of immunization guidelines: a missed opportunity for preventing infection in immunocompromised IBD patients. Inflamm Bowel Dis. 2012; 18:34–40. PMID: 21337671.

21. Wagnon JH, Leiman DA, Ayers GD, Schwartz DA. Survey of gastroenterologists’ awareness and implementation of AGA guidelines on osteoporosis in inflammatory bowel disease patients: are the guidelines being used and what are the barriers to their use? Inflamm Bowel Dis. 2009; 15:1082–1089. PMID: 19137605.

22. Jung YS, Park JH, Kim HJ, et al. Insufficient knowledge of korean gastroenterologists regarding the vaccination of patients with inflammatory bowel disease. Gut Liver. 2014; 8:242–247. PMID: 24827619.

23. Gupta V, Dawood FS, Muangchana C, et al. Influenza vaccination guidelines and vaccine sales in southeast Asia: 2008-2011. PLoS One. 2012; 7:e52842. PMID: 23285200.

24. Mithal A, Kaur P. Osteoporosis in Asia: a call to action. Curr Osteoporos Rep. 2012; 10:245–247. PMID: 22898971.

25. Wasan SK, Coukos JA, Farraye FA. Vaccinating the inflammatory bowel disease patient: deficiencies in gastroenterologists knowledge. Inflamm Bowel Dis. 2011; 17:2536–2540. PMID: 21538710.

26. Hung IF, Tantawichien T, Tsai YH, Patil S, Zotomayor R. Regional epidemiology of invasive pneumococcal disease in Asian adults: epidemiology, disease burden, serotype distribution, and antimicrobial resistance patterns and prevention. Int J Infect Dis. 2013; 17:e364–e373. PMID: 23416209.

27. Mangtani P, Shah A, Roberts JA. Validation of influenza and pneumococcal vaccine status in adults based on self-report. Epidemiol Infect. 2007; 135:139–143. PMID: 16740194.

Fig. 1
Delivery and awareness of performance measures in Asian countries. Delivery of performance measures varied significantly among Asian countries. Other Asian countries include Taiwan, Hong-Kong, India, Singapore, the Philippines, Malaysia, and Indonesia. Performance measures were arranged in order that well delivered. C. difficile, Clostridium difficile; VTEs, venous thromboembolisms.
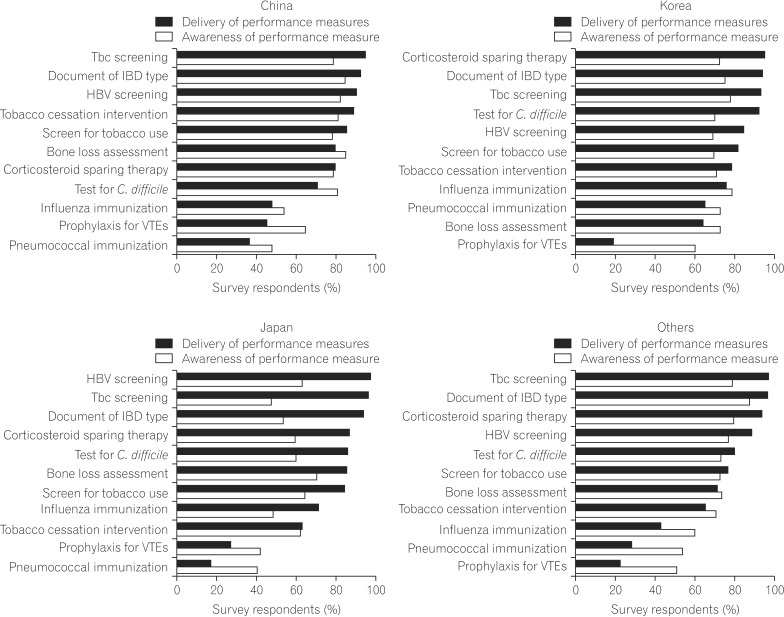
Fig. 2
The association between awareness and delivery of performance measures. The association between the delivery and awareness of performance measures varied among Asian countries. Other Asian countries include Taiwan, Hong-Kong, India, Singapore, the Philippines, Malaysia, and Indonesia. The awareness had positive association to the delivery of performance measures. aPerformance measure that had a significant relationship between awareness and performance (P<0.05). VTEs, venous thromboembolisms; TNF, tumor necrosis factor.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download