Abstract
The clinical importance of nontuberculous mycobacteria (NTM) has recently been increasing worldwide. In Korea, Mycobacterium avium complex and M. abscessus are the most commonly encoun-tered pathogens of NTM lung disease. When NTM lung disease occurs, it is likely to present in one of two prototypical forms: a fibrocavitary form often affecting older male smokers with chronic obstructive pulmonary disease and nodular bronchiectatic form classically occurring in middle-aged or older women who have never smoked. Since NTM are ubiquitous in the environment, the isolation and identification of causative organisms are mandatory for diagnosis, and some specific diagnostic criteria have been proposed. The decision on whether to treat a patient remains a matter of careful individual evaluation taking into account the NTM species, extent and form of the disease, and overall condition of the patient. Although treatment regimens that include the new macrolides such as clarithromycin or azithromycin are more effective than earlier regimens, treatment of these infections is time-consuming, complicated, and often ineffective. Surgery for localized NTM lung disease may be useful for selected patients. Observation without treatment may be appropriate for some patients with a slowly progressive form of the disease that is expected to be particularly difficult to treat.
Figures and Tables
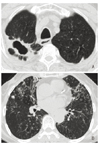
Figure 1
(A) A 72-year-old man with a previous history of pulmonary tuberculosis who presented with cough and sputum. His sputum specimens were positive for acid fast bacilli and grew Mycobacterium intracellulare. Chest computed tomography show right upper lobe cavity with surrounding subpleural consolidation. (B) A 76-year-old woman, a lifelong non-smoker, who presented with chronic cough and sputum. Her sputum grew M. intracellulare. Chest computed tomography shows extensive right middle lobe and lingular bronchiectasis and centrilobular nodules in both lungs.
References
1. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ Jr, Winthrop K. ATS Mycobacterial Diseases Subcommittee. American Thoracic Society. Infectious Disease Society of America. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.

2. Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous mycobacterial pulmonary diseases: a Korean perspective. J Korean Med Sci. 2005. 20:913–925.

3. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, Bai GH. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006. 129:341–348.

4. Park YS, Lee CH, Lee SM, Yang SC, Yoo CG, Kim YW, Han SK, Shim YS, Yim JJ. Rapid increase of non-tuberculous mycobacterial lung diseases at a tertiary referral hospital in South Korea. Int J Tuberc Lung Dis. 2010. 14:1069–1071.
5. Daley CL, Griffith DE. Pulmonary non-tuberculous mycobacterial infections. Int J Tuberc Lung Dis. 2010. 14:665–671.
26. Diagnosis and. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Medical Section of the American Lung Association. Am J Respir Crit Care Med. 1997. 156(2 Pt 2):S1–S25.
7. Lam PK, Griffith DE, Aksamit TR, Ruoss SJ, Garay SM, Daley CL, Catanzaro A. Factors related to response to intermittent treatment of Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2006. 173:1283–1289.

8. Griffith DE, Brown-Elliott BA, Shepherd S, McLarty J, Griffith L, Wallace RJ Jr. Ethambutol ocular toxicity in treatment regimens for Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2005. 172:250–253.

9. Hasegawa N, Nishimura T, Ohtani S, Takeshita K, Fukunaga K, Tasaka S, Urano T, Ishii K, Miyairi M, Ishizaka A. Therapeutic effects of various initial combinations of chemotherapy including clarithromycin against Mycobacterium avium complex pulmonary disease. Chest. 2009. 136:1569–1575.

10. Kim EY, Chi SY, Oh IJ, Kim KS, Kim YI, Lim SC, Kim YC, Kwon YS. Treatment outcome of combination therapy including clarithromycin for Mycobacterium avium complex pulmonary disease. Korean J Intern Med. 2011. 26:54–59.

11. Field SK, Fisher D, Cowie RL. Mycobacterium avium complex pulmonary disease in patients without HIV infection. Chest. 2004. 126:566–581.

12. Jeon K, Kwon OJ, Lee NY, Kim BJ, Kook YH, Lee SH, Park YK, Kim CK, Koh WJ. Antibiotic treatment of Mycobacterium abscessus lung disease: a retrospective analysis of 65 patients. Am J Respir Crit Care Med. 2009. 180:896–902.

13. Jarand J, Levin A, Zhang L, Huitt G, Mitchell JD, Daley CL. Clinical and microbiologic outcomes in patients receiving treatment for Mycobacterium abscessus pulmonary disease. Clin Infect Dis. 2011. 52:565–571.

14. Lyu J, Jang HJ, Song JW, Choi CM, Oh YM, Lee SD, Kim WS, Kim DS, Shim TS. Outcomes in patients with Mycobacterium abscessus pulmonary disease treated with long-term injectable drugs. Respir Med. 2011. 105:781–787.

15. Kim HY, Kook Y, Yun YJ, Park CG, Lee NY, Shim TS, Kim BJ, Kook YH. Proportions of Mycobacterium massiliense and Mycobacterium bolletii strains among Korean Mycobacterium chelonae-Mycobacterium abscessus group isolates. J Clin Microbiol. 2008. 46:3384–3390.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download