1. Javed F, Romanos GE. Impact of diabetes mellitus and glycemic control on the osseointegration of dental implants: a systematic literature review. J Periodontol. 2009; 80:1719–1730.

2. Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010; 38:612–620.

3. Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998; 11:491–501.
4. Sakka S, Coulthard P. Bone quality: a reality for the process of osseointegration. Implant Dent. 2009; 18:480–485.

5. Song YD, Jun SH, Kwon JJ. Correlation between bone quality evaluated by cone-beam computerized tomography and implant primary stability. Int J Oral Maxillofac Implants. 2009; 24:59–64.
6. Felsenberg D, Boonen S. The bone quality framework: determinants of bone strength and their interrelationships, and implications for osteoporosis management. Clin Ther. 2005; 27:1–11.

7. Bouxsein ML. Bone quality: where do we go from here? Osteoporos Int. 2003; 14:Suppl 5. S118–27.

8. Friberg B, Sennerby L, Linden B, Gröndahl K, Lekholm U. Stability measurements of one-stage Brånemark implants during healing in mandibles. A clinical resonance frequency analysis study. Int J Oral Maxillofac Surg. 1999; 28:266–272.

9. van Steenberghe D, Quirynen M, Molly L, Jacobs R. Impact of systemic diseases and medication on osseointegration. Periodontol 2000. 2003; 33:163–171.

10. Kaneko T. Pulsed oscillation technique for assessing the mechanical state of the dental implant-bone interface. Biomaterials. 1991; 12:555–560.

11. Kaneko T, Nagai Y, Ogino M, Futami T, Ichimura T. Acoustoelectric technique for assessing the mechanical state of the dental implant-bone interface. J Biomed Mater Res. 1986; 20:169–176.

12. Noyes DH, Solt CW. Measurement of mechanical mobility of human incisors with sinusoidal forces. J Biomech. 1973; 6:439–442.

13. Turkyilmaz I, McGlumphy EA. Influence of bone density on implant stability parameters and implant success: a retrospective clinical study. BMC Oral Health. 2008; 8:32.

14. Isoda K, Ayukawa Y, Tsukiyama Y, Sogo M, Matsushita Y, Koyano K. Relationship between the bone density estimated by cone-beam computed tomography and the primary stability of dental implants. Clin Oral Implants Res. 2012; 23:832–836.

15. Rozé J, Babu S, Saffarzadeh A, Gayet-Delacroix M, Hoornaert A, Layrolle P. Correlating implant stability to bone structure. Clin Oral Implants Res. 2009; 20:1140–1145.

16. Hsu JT, Huang HL, Tsai MT, Wu AY, Tu MG, Fuh LJ. Effects of the 3D bone-to-implant contact and bone stiffness on the initial stability of a dental implant: micro-CT and resonance frequency analyses. Int J Oral Maxillofac Surg. 2013; 42:276–280.

17. Kabel J, Odgaard A, van Rietbergen B, Huiskes R. Connectivity and the elastic properties of cancellous bone. Bone. 1999; 24:115–120.

18. Pothuaud L, Van Rietbergen B, Mosekilde L, Beuf O, Levitz P, Benhamou CL, et al. Combination of topological parameters and bone volume fraction better predicts the mechanical properties of trabecular bone. J Biomech. 2002; 35:1091–1099.

19. Rüegsegger P, Koller B, Müller R. A microtomographic system for the nondestructive evaluation of bone architecture. Calcif Tissue Int. 1996; 58:24–29.

20. Uchiyama T, Tanizawa T, Muramatsu H, Endo N, Takahashi HE, Hara T. A morphometric comparison of trabecular structure of human ilium between microcomputed tomography and conventional histomorphometry. Calcif Tissue Int. 1997; 61:493–498.

21. Ho JT, Wu J, Huang HL, Chen MY, Fuh LJ, Hsu JT. Trabecular bone structural parameters evaluated using dental cone-beam computed tomography: cellular synthetic bones. Biomed Eng Online. 2013; 12:115.

22. Panmekiate S, Ngonphloy N, Charoenkarn T, Faruangsaeng T, Pauwels R. Comparison of mandibular bone microarchitecture between micro-CT and CBCT images. Dentomaxillofac Radiol. 2015; 44:20140322.

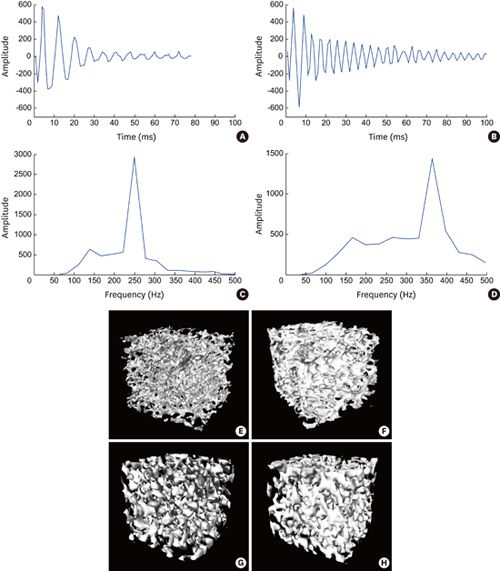
23. Kim DS, Lee WJ, Choi SC, Lee SS, Heo MS, Huh KH, et al. A new method for the evaluation of dental implant stability using an inductive sensor. Med Eng Phys. 2012; 34:1247–1252.

24. Kim DS, Lee WJ, Choi SC, Lee SS, Heo MS, Huh KH, et al. Comparison of dental implant stabilities by impact response and resonance frequencies using artificial bone. Med Eng Phys. 2014; 36:715–720.

25. Greenstein G, Cavallaro J, Romanos G, Tarnow D. Clinical recommendations for avoiding and managing surgical complications associated with implant dentistry: a review. J Periodontol. 2008; 79:1317–1329.

26. Natali AN, Carniel EL, Pavan PG. Investigation of viscoelastoplastic response of bone tissue in oral implants press fit process. J Biomed Mater Res B Appl Biomater. 2009; 91:868–875.

27. Bischof M, Nedir R, Szmukler-Moncler S, Bernard JP, Samson J. Implant stability measurement of delayed and immediately loaded implants during healing. Clin Oral Implants Res. 2004; 15:529–539.

28. Miyamoto I, Tsuboi Y, Wada E, Suwa H, Iizuka T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery--clinical, prospective, biomechanical, and imaging study. Bone. 2005; 37:776–780.

29. Johns RB, Jemt T, Heath MR, Hutton JE, McKenna S, McNamara DC, et al. A multicenter study of overdentures supported by Brånemark implants. Int J Oral Maxillofac Implants. 1992; 7:513–522.
30. Saadoun AP, LeGall ML. Clinical results and guidelines on Steri-Oss endosseous implants. Int J Periodontics Restorative Dent. 1992; 12:486–495.
31. Atsumi M, Park SH, Wang HL. Methods used to assess implant stability: current status. Int J Oral Maxillofac Implants. 2007; 22:743–754.
32. Huwiler MA, Pjetursson BE, Bosshardt DD, Salvi GE, Lang NP. Resonance frequency analysis in relation to jawbone characteristics and during early healing of implant installation. Clin Oral Implants Res. 2007; 18:275–280.

33. Ito Y, Sato D, Yoneda S, Ito D, Kondo H, Kasugai S. Relevance of resonance frequency analysis to evaluate dental implant stability: simulation and histomorphometrical animal experiments. Clin Oral Implants Res. 2008; 19:9–14.

34. Nkenke E, Hahn M, Weinzierl K, Radespiel-Tröger M, Neukam FW, Engelke K. Implant stability and histomorphometry: a correlation study in human cadavers using stepped cylinder implants. Clin Oral Implants Res. 2003; 14:601–609.

35. de Oliveira RC, Leles CR, Lindh C, Ribeiro-Rotta RF. Bone tissue microarchitectural characteristics at dental implant sites. Part 1: identification of clinical-related parameters. Clin Oral Implants Res. 2012; 23:981–986.

36. Ab-Lazid R, Perilli E, Ryan MK, Costi JJ, Reynolds KJ. Pullout strength of cancellous screws in human femoral heads depends on applied insertion torque, trabecular bone microarchitecture and areal bone mineral density. J Mech Behav Biomed Mater. 2014; 40:354–361.

37. Ab-Lazid R, Perilli E, Ryan MK, Costi JJ, Reynolds KJ. Does cancellous screw insertion torque depend on bone mineral density and/or microarchitecture? J Biomech. 2014; 47:347–353.

38. Baum T, Carballido-Gamio J, Huber MB, Müller D, Monetti R, Räth C, et al. Automated 3D trabecular bone structure analysis of the proximal femur--prediction of biomechanical strength by CT and DXA. Osteoporos Int. 2010; 21:1553–1564.

39. Huh KH, Yi WJ, Jeon IS, Heo MS, Lee SS, Choi SC, et al. Relationship between two-dimensional and three-dimensional bone architecture in predicting the mechanical strength of the pig mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:363–373.

40. Syahrom A, Abdul Kadir MR, Abdullah J, Öchsner A. Mechanical and microarchitectural analyses of cancellous bone through experiment and computer simulation. Med Biol Eng Comput. 2011; 49:1393–1403.













 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download