INTRODUCTION
The level of periodontal support is the most critical factor for predicting the prognosis of healing after periodontal treatment [
1,
2]. In general, a tooth with periodontal destruction extending beyond the root apex is considered hopeless, and extraction is the only possible treatment. Neither nonsurgical nor surgical treatment is effective in such cases because of limited accessibility to instrumentation and unfavorable tooth stability after treatment. In the process of periodontal treatment, thorough instrumentation and antibacterial cleansing are performed to remove microbial infection sources. Nevertheless, there are limitations to accessing the periapical area and several studies have reported that microbial etiologic factors were found around the root apex area in recurrent infectious diseases [
3,
4]. Moreover, the increased mobility of a treated tooth can affect the outcome of periodontal treatment negatively. Tooth mobility may inhibit bone gain and periodontal regeneration, consequently forming a deep pocket and inducing apical migration of epithelial attachment [
5].
Intentional replantation may be useful in these situations because this technique seems to resolve the limitations of conventional periodontal treatment. The tooth surfaces, including inaccessible areas, can be visualized and instrumented completely without damaging adjacent periodontal tissue. Some investigators have attempted intentional replantation with periodontally involved teeth. Lu [
6] reported successful treatment results with periodontally involved teeth in which intentional replantation was performed first. The researcher intentionally replanted an endodontically mistreated and periodontally involved mandibular first molar and maintained the tooth for 32 months in a functional and asymptomatic condition. Demiralp et al. [
7] intentionally replanted fifteen periodontally involved hopeless teeth and followed them for 6 months. They suggested that intentional replantation could be an alternative approach to extraction in cases where advanced periodontal destruction was present and no other treatment could be considered.
However, in spite of the potential of this technique, very few investigators have performed intentional replantation with periodontally involved teeth. This might be due to the questionable prognosis of replanted teeth. Although some studies have shown favorable results, intentional replantation of a periodontally involved tooth seems to carry the risk of reinfection and unstable tooth stability, which results in tooth loss.
Previously, Lee et al. extracted periodontally hopeless teeth and replanted them after a delay to relieve inflammation and provide a scaffold with woven bone formation (unpublished data). They reported successful clinical and radiographic results by delaying the replant procedure, which they named "delayed intentional replantation" and concluded that the procedure could be an alternative treatment option for periodontally involved hopeless teeth. However, in the study, the number of cases involved was limited and statistical analysis was not conducted. Therefore, additional research that evaluates the survival rate of the delayed intentional replantation procedure would be useful in determining the outcomes of the treatment.
The purpose of this study is to retrospectively evaluate the survival of periodontally hopeless teeth that were intentionally replanted after a delay and to compare the radiographic characteristics of the survival group with those of the failure group.
DISCUSSION
This study describes the clinical and radiological outcomes of delayed intentional replantation of teeth deemed hopeless due to severe periodontal destruction. We assumed that waiting for improved conditions of the extraction socket by delaying the replantation procedure could produce more favorable outcomes from intentional replantation.
Although it is commonly known that intentional replantation is contraindicated in a periodontally involved tooth [
11], several studies have reported successful clinical results and have suggested intentional replantation as an alternative treatment technique of last resort for a periodontally involved tooth [
6,
7]. However, little research has addressed this subject. This may be due to the possible risks mentioned below. Intentional replantation includes the following processes: atraumatic tooth extraction, removal of local factors on both the tooth surface and extraction socket, and reinsertion of the tooth. Through this process, local factors on the tooth surface and extraction socket causing periodontal disease can be eliminated completely. However, forming substantial space between the tooth and socket wall is inevitable as a result of this process. This space can negatively affect the result of the treatment. First, it is likely to increase the mobility of the replanted tooth. Generally, in case of tooth replantation, if the teeth are fixed in the coronal area, the teeth might be mobile in the apical area. Ferencz [
5] reported that reduced periodontal regeneration could occur if the treated teeth were not fixed firmly. Mobility can decrease the amount of regenerated periodontal tissue after treatment. Secondly, reinfection and delayed periodontal regeneration might occur because several microorganisms that can invade through the gap between a tooth root and extraction socket wall. In 2003, Demiralp et al. [
7] performed intentional replantation using teeth that needed to be extracted due to severe periodontal destruction. After 6 months, they found that alveolar bone loss had diminished somewhat, but was still more than 55% of the total tooth length.
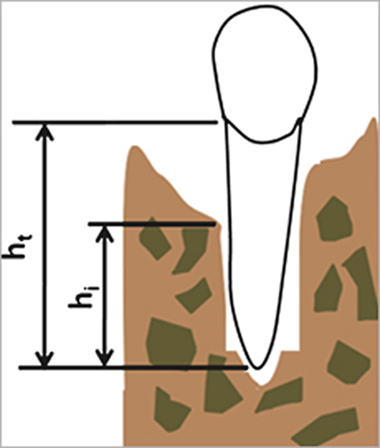
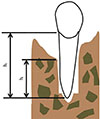
In order to overcome the drawbacks of intentional replantation such as increased tooth mobility and the possibility of reinfection, we separated hopeless teeth from their extraction sockets for 10 days and then performed delayed replantation. Woven bone formed in the extraction socket one to two weeks after tooth extraction [
12,
13], and this bone not only helped each replanted tooth to be fixed firmly but also acted as a scaffold for periodontal tissue regeneration. Furthermore, 10 days of separation was rarely long enough to permit a gap between the replanted tooth and socket wall and thus decreased the risk of reinfection and reduced regeneration. Additionally, the teeth could be replanted in the healing phase since the inflammatory phase of the extraction socket was converted to the healing phase during that separation period. In a previous immunochemical study [
14] regarding the socket from which a periodontally involved tooth was extracted, inflammation persisted in the socket for 3 to 7 days, and was followed by formation of woven bone and angiogenesis. In the same way, we assumed that we could expect a favorable outcome by performing replantation to the socket in the healing phase rather than during the inflammatory phase.
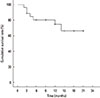
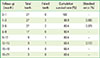
In our study, 27 teeth with severe periodontal destruction were intentionally extracted, replanted after a delay, and followed up for 3 to 21 months. Among these teeth, 7 teeth were removed and the cumulative survival rate was 66.4%. The radiologic examination was performed to all of the replanted teeth during the follow-up period, and there were remarkably different characteristics of the survival and failure groups.
In the survival group, the amount of BL was reduced from 68.4% to 34.77% three months after replantation. After that, a consistent level of alveolar bone was maintained. Similarly, the amount of BG was 45.02% three months after replantation and remained steady after that time. The regeneration of alveolar bone occurred rapidly from the bottom of the socket, and the amount of BG was sufficient to support the tooth stably. The advantages of delaying the replantation mentioned above might contribute to the rapid and sufficient bone formation we observed in our successful cases.
The healing process after replantation of the failure group produced different radiological findings from that of the survival group. Similar to the survival group, new bone rapidly formed from the bottom of socket in the failure group. However, an obvious radiolucent line was commonly exhibited along the replanted root surface in the failure group. The radiolucent line prolonged and expanded as time passed. Finally, the teeth had to be extracted due to signs of inflammation and loss of stability. Based on the radiologic findings, it was thought that the failure to maintain and construct vital periodontal structures on the root surface suitable for bone formation was the cause of extraction. Previously, Nasjleti et al. [
15] reported that, as along with other factors, maintaining the periodontal structures on the root surface during the delay period was important for periodontal healing after replantation. In our study, the surface of the extracted tooth was thoroughly debrided to remove pathologic factors completely and stored in dexamethasone solution. Kum et al. [
16] studied the effect of dexamethasone solution after delayed tooth replantation and concluded that the use of this solution might reduce the degree or rate of root resorption. However, the extracted teeth were stored for ten days, and periodontal structures on the tooth surface could be compromised by these procedures. According to a previous study, the necrotic periodontal membrane remaining on the tooth surface could cause ankylosis and root resorption [
17,
18]. Based on these reports, we debrided and polished the tooth surface by mechanical methods with an ultrasonic scaler and fine diamond bur. However, these could produce harmful effects on the periodontal structures needed for periodontal regeneration. In addition, the media used for storing the extracted teeth had no bioactive effect for maintaining and regenerating the periodontal structures. Baltacioglu et al. [
19] performed intentional replantation with regenerative techniques using enamel matrix derivative and demineralized freeze-dried bone allograft and reported successful results. Thus alternative methods for treating the tooth surface like using chemical agents and optimal storage media that can maintain regenerative periodontal structures should be developed for improved results of delayed intentional replantation.
In conclusion, delayed intentional replantation has many advantages and could serve as an alternative treatment for periodontally involved hopeless teeth. However, techniques and methods for maintaining the vitality of the periodontal structures on the tooth surface should be developed for improved and more predictable results.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download