Abstract
Most cases of hypercalcaemia are secondary to malignancy or primary hyperparathyroidism. We report a patient presenting with a triad of hypercalcemia, metabolic alkalosis, and renal failure secondary to treatment of iatrogenic hypoparathyroidism and osteoporosis. Persistent ingestion of calcium carbonate and vitamin D caused milk-alkali syndrome. The patient was managed with intravenous fluids and withdrawal of calcium carbonate and vitamin D. She responded well to the treatment and the calcium concentration, renal function and metabolic alkalosis were normalized. Milk-alkali syndrome may be important as a reemerging cause of hypercalcemia.
Most cases of hypercalcemia are secondary to malignancy or primary hyperparathyroidism1). Milk-alkali syndrome previously accounted for about 12% of cases and ranks the third among the causes of hypercalcemia in hospitalized patients2). The syndrome consists of the triad of hypercalcemia, metabolic alkalosis, and renal insufficiency associated with ingestion of large amount of calcium and absorbable alkali. After the advent of non absorbable antacids and later histamine-2 blockers, the incidence of this syndrome dropped to less than 1% of etiologies of hypercalcemia in the mid-seventies3). However, recently the incidence has increased secondary to the use of calcium carbonate for the prevention and treatment of osteoporosis and hyperphosphataemia in patients with chronic kidney disease4). We report a case of milk-alkali syndrome secondary to ingestion of calcium carbonate and vitamin D, in addition to taking bisphosphonate, and iatrogenic hypoparathyroidism.
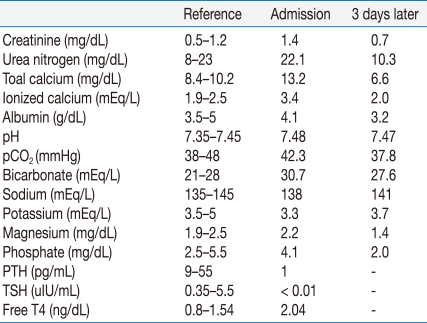
An 80-year-old female visited our hospital with a one-week history of nausea and general weakness. Her past medical history included a total thyroidectomy 10 years ago for papillary thyroid carcinoma. She had been taking levothyroxine for iatrogenic hypothyroidism, calcium carbonate (3.0 g daily) and active vitamin D (1.5 µg daily) for iatrogenic hypoparathyroidism, and bisphosphonate for osteoporosis. Her pulse was 68/min, blood pressure 130/80 mmHg, body temperature 36.9℃, and her skin turgor was decreased. Urinalysis was within the normal range except for the red blood cell count, 8-10/HPF. The pertinent laboratory tests revealed severe hypercalcemia, acute kidney injury and metabolic alkalosis (Table 1). Her chest computed tomography, protein electrophoresis, esophagoduodenoscopy were non-specific. She was initially managed with 3 L of saline solution, 20 mg of furosemide administered intravenously and withdrawal of calcium carbonate and vitamin D. She responded well to aggressive intravenous fluid administration and the calcium concentration fell rapidly. Three days later, nausea and other symptoms improved, and her hypercalcemia, metabolic alkalosis and renal function were normalized (Table 1).
Milk-alkali syndrome consists of the triad of hypercalcemia, metabolic alkalosis, and renal insufficiency associated with ingestion of large amount of calcium and absorbable alkali. Our patient had profound symptomatic hypercalcemia, which caused gastrointestinal symptoms and muscle weakness. Work-up for malignancy was negative and a thorough history taking revealed calcium and alkali ingestion. The clinical laboratory data showed characteristics of milk-alkali syndrome and we excluded other causes of hypercalcemia5).
In the early 20th century, calcium-containing antacids and milk were used to treat peptic ulcer disease. Sometimes this therapy was associated with toxicity. Hardt and Rivers identified milk-alkali syndrome in 1923 and reported that it caused headache, nausea, vomiting, dizziness, musculoskeletal pains, and weakness6). By 1985, milk-alkali syndrome was considered as less than one percent of cases of hypercalcemia. However, there has been a resurgence of this disorder, probably secondary to the use of calcium carbonate for osteoporosis and hyperphosphataemia in patients with chronic kidney disease4). Therefore, some recommend that the term "calcium-alkali syndrome", which broadens the definition of the condition, should replace milk-alkali syndrome, since the term "milk-alkali syndrome" no longer reflects the etiologic origin7).
The pathophysiology of the milk-alkali syndrome is poorly understood. It is unclear why only some individuals are affected by excessive ingestion, but it has been suggested that they absorb more calcium than others8). Patients who appear to be at high risk for milk-alkali syndrome include old age, volume depletion and medication that reduces glomerular filtration rate, such as angiotensin converting enzyme inhibitors, angiotensin receptor blockers or non-steroidal anti-inflammatory agents8). Hypercalcemia causes reduced glomerular filtration rate, increased sodium excretion and depletion of total body water, leading to increased bicarbonate reabsorption and metabolic alkalosis,. Alkalosis enhances calcium reabsorption in the distal nephron, thus, aggravating the hypercalcemia8, 9).
As for the management, withdrawal of the offending agent and intravenous volume expansion are the most initial steps. Usually, these interventions will reverse hypercalcemia and alkalosis. Renal function can return to normal if the diagnosis of milk alkali syndrome is made early in the course of the disease. Hemodialysis may be required in some clinical settings. In conclusion, milk alkali syndrome may be important as a reemerging cause of hypercalcemia. A detailed history, including the use of over-the-counter medication, should be taken in all patients.
References
1. Lafferty FW. Differential diagnosis of hypercalcemia. J Bone Miner Res. 1991; 6(Suppl 2):S51–S59. PMID: 1763670.

2. Beall DP, Scofield RH. Milk-alkali syndrome associated with calcium carbonate consumption. Report of 7 patients with parathyroid hormone levels and an estimate of prevalence among patients hospitalized with hypercalcemia. Medicine (Baltimore). 1995; 74:89–96. PMID: 7891547.

5. Orwoll ES. The milk-alkali syndrome: current concepts. Ann Intern Med. 1982; 97:242–248. PMID: 7049033.

6. Hardt LL, Rivers AB. Toxic manifestations following the alkaline treatment of peptic ulcer. Arch Intern Med. 1923; 31:171–180.

7. Patel AM, Goldfarb S. Got calcium? Welcome to the calciumalkali syndrome. J Am Soc Nephrol. 2010; 21:1440–1443. PMID: 20413609.

8. Felsenfeld AJ, Levine BS. Milk alkali syndrome and the dynamics of calcium homeostasis. Clin J Am Soc Nephrol. 2006; 1:641–654. PMID: 17699269.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download