Abstract
Acquired factor VIII deficiency is very rare, often fatal. It is associated with pregnancy, autoimmune diseases, malignancy, and drugs, although no underlying cause is found in 50%. A 49-year-old male was referred with right shoulder bruising. The coagulation test showed a prolonged activated partial thromboplastin time. The factor VIII level was less than 1%, and the factor VIII inhibitor antibody titer was 246 Bethesda units/mL. The findings were compatible with acquired factor VIII deficiency. He had consumed the dried gallbladder of a cobra, Naja naja, for two weeks, it contained venom. After the initial treatment with factor VIII, he did not take supplemental coagulation factor VIII. The patient was readmitted with left forearm swelling. He lost consciousness suddenly and brain computed tomography (CT) revealed a subdural hematoma. Despite administering recombinant factor VII, his bleeding was not controlled and he died.
Acquired factor VIII deficiency is caused by the development of autoantibodies directed against circulating coagulation factor VIII, which inhibits its function [1, 2]. It is very uncommon, often life-threatening [3]. It may be associated with pregnancy, the postpartum period, autoimmune conditions, drugs, lymphoproliferative disorders, or malignancies. In approximately half of the diagnosed cases, no underlying disease is detected [3-6]. We report a rare case of subdual hemorrhage in a man, who acquired factor VIII inhibitors and developed coagulopathy after consuming toxin of the cobra, Naja naja. This is the first report of acquired factor VIII inhibitor developed after Cobratoxin intake.
A 49-year-old male was admitted with a 10-day history of subcutaneous hemorrhage of the right shoulder (Fig. 1) and left thigh. His medical history included diabetes mellitus and hypertension. The patient was being treated with losartan 50 mg/day for hypertension and metformin 500 mg twice a day for diabetes. He had eaten 10 g of dried gall bladder of a cobra, Naja naja in Thailand one month ago. The gallbladder contained venom, and had been manufactured using an unknown process. His family history was negative for hemorrhagic disorder.
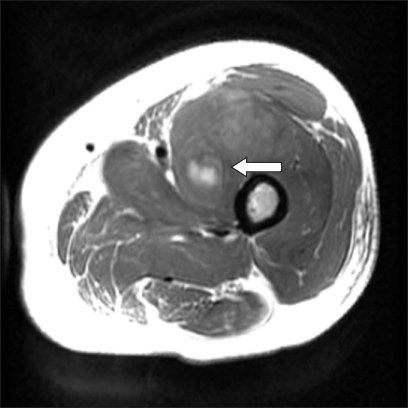
His vital signs included blood pressure of 130/70 mmHg and heart rates of 100/min. Laboratory test showed a prolonged activated partial thromboplastin time (aPTT) exceeding 120 seconds (normal range, 30-47 seconds), not corrected with plasma mixing test. His prothrombin time was 10 seconds (normal range, 10-13 seconds), the level of FDP was 11.71 ug/mL (normal range, below 5 ug/mL), and D-dimer was 3.42 ug/mL (normal range, below 1.3 ug/mL). His hemoglobin was 7.0 g/dL and platelet count was 323×109/L. The factor VIII level was less than 1%, and his factor VIII inhibitor antibody titer was 246 Bethesda units/mL (normal range, 0-0.7 Bethesda units/mL). Lupus anticoagulant antibody, anti-nuclear antibody and anti-phospholipid antibody were negative. The level of factor XI and factor XII was normal. His chest and abdominopelvic CT scan were negative for malignancy. He was diagnosed with acquired factor VIII deficiency. Magnetic resonance imaging (MRI) of the thigh showed hematomas in the left vastus medialis muscle (Fig. 2). The patient was treated with an intravenous infusion of factor VIII 3,000 U (50 U/kg) every 8 hours. One month after treatment, the patient's symptoms improved, but his factor VIII inhibitor antibody titer was still high (147 Bethesda units/mL).
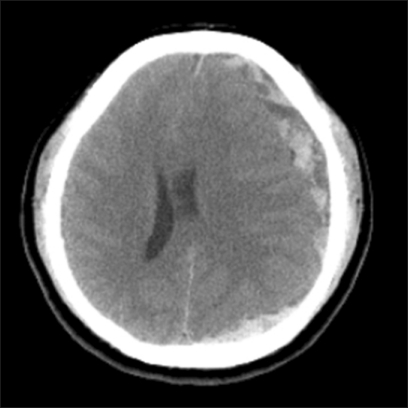
One year later, the patient presented with swelling of the left forearm. He had an aPTT exceeding 120 seconds due to the presence of high titers of factor VIII inhibitor (217 Bethesda units/mL). Ten days after admission, he lost consciousness suddenly. Brain CT scan revealed a mixed subacute subdural hematoma in the left fronto-temporo-occipital areas (Fig. 3) and recombinant factor VII was infused at a dose of 360 KIU/day. Despite treatment, the patient's bleeding worsened. Two weeks later, multifocal subarachnoid hemorrhages and intracranial hemorrhages in both cerebral hemispheres were revealed. He subsequently died.
Acquired factor VIII deficiency is rare, but life-threatening. It results from the development of inhibitors, that typically interfere with the coagulant properties of factor VIII [1, 2, 7]. The estimated annual incidence is between 1.3 and 1.5 million per year [1]. The clinical picture is characterized by spontaneous and often sudden onset of severe hemorrhage in a patient with no bleeding history. More than 80% of patients have hemorrhages into the skin, muscles or soft tissues, and mucous membranes [2]. Mortality rates range from 9 to 22% [8]. Up to 30% of patients resolve without treatment. However, the spontaneous disappearance of inhibitors is unpredictable and may occur over many years [8]. The prognosis is worse in patients with higher inhibitor titers [9]. Our patient had a persistently high titer of factor VIII inhibitor antibody. For a better prognosis, eradication of the inhibitor and maintenance of normal level of clotting factor VIII are important [10].
The therapeutic strategy is to stop the hemorrhage and reduce the autoantibody levels. Bypassing products currently available for bleeding control are recombinant activated factor VII (rFVIIa) and plasma-derived activated prothrombin complex concentrate (aPCC) [11]. In patients with a high inhibitor titer and severe hemorrhages, the extracorporeal removal of the autoantibody by therapeutic plasmapheresis can be used before factor concentrate treatment [11]. There are two case reports in Korea which were successfully treated with combination therapy that included therapeutic plasmapheresis [12]. Once hemostasis is achieved, autoantibody eradication is the second major goal of acquired hemophilia therapy. The inhibitor may also be eradicated with immunosuppressive agents, including corticosteroids and cytotoxic drugs, such as cyclophosphamide, azathioprine, 6-mercaptopurine, and vincristine.
We report the first case of acquired factor VIII deficiency in a patient, who suffered from coagulopathy after consuming the dried gallbladder of a cobra. Coagulopathy is a significant cause of both morbidity and mortality in snakebite patients [13, 14]. A wide variety of venom components can act as procoagulants, activating the coagulation system in vivo, and causing the consumption of coagulation factors, resulting in clinical anticoagulation. Fibrinogen clotting and fibrinolytic snake venom toxins exert a direct effect on the actual thrombus-forming protein, fibrinogen, but in varying ways. Fibrinogen may be split into fibrin and then degradation products, or it may be only partially split, leaving an ineffective form of fibrinogen circulating, the end result being an increased bleeding tendency. Snake venom inhibits platelet activity too, thus reducing their effectiveness in hemostasis [13, 14].
Another study reported there is transient presence of an inhibitor to factors VIII, IX and XI in cases of tiger snake envenomation [15]. In our case, cobra toxin was probably the cause of development of factor VIII inhibitor, since the acquired factor VIII deficiency developed right after consuming the cobra toxin, and we did not find any other possible cause of acquired factor VIII deficiency in this patient. Perhaps cobra toxin entered the blood stream through damaged oral mucosa, and acted as factor VIII inhibitor. In order to make a clear connection between cobra toxin and acquired factor VIII deficiency, further evaluation about the effects of snake venom on individual coagulation factors is needed.
References
1. Hay CR. Acquired haemophilia. Baillieres Clin Haematol. 1998; 11:287–303. PMID: 10097808.
2. Hay CR, Baglin TP, Collins PW, Hill FG, Keeling DM. The diagnosis and management of factor and IX inhibitors: a guideline from the UK haemophilia centre doctors organization (UKHCDO). Br J Haematol. 2000; 111:78–90. PMID: 11091185.
3. Franchini M. Postpartum acquired factor VIII inhibitors. Am J Hematol. 2006; 81:768–773. PMID: 16868941.

4. Stewart AJ, Manson LM, Dasani H, et al. Acquired haemophilia in recipients of depot thioxanthenes. Haemophilia. 2000; 6:709–712. PMID: 11122403.

5. Sallah S, Wan JY. Inhibitors against factor VIII associated with the use of interferon alpha and fludarabine. Thromb Haemost. 2001; 86:1119–1121. PMID: 11686336.
6. Regina S, Colombat P, Fimbel B, Guerois C, Gruel Y. Acquired inhibitor to factor VIII in a patient with Hodgkin's disease following treatment with interferon-alpha. Haemophilia. 2001; 7:526–527. PMID: 11554946.

7. Moraca RJ, Ragni MV. Acquired anti-FVIII inhibitors in children. Haemophilia. 2002; 8:28–32. PMID: 11886462.

8. Lottenberg R, Kentro TB, Kitchens CS. Acquired hemophilia. A natural history study of 16 patients with factor VIII inhibitors receiving little or no therapy. Arch Intern Med. 1987; 147:1077–1081. PMID: 3109341.

9. Tagariello G, Sartori R, Radossi P, Gandini G, Franchini M. Intensive blood transfusion support in acquired hemophilia A. Ann Hematol. 2007; 86:229–230. PMID: 17151880.

10. Delgado J, Jimenez-Yuste V, Hernandez-Navarro F, Villar A. Acquired haemophilia: review and meta-analysis focused on therapy and prognostic factors. Br J Haematol. 2003; 121:21–35. PMID: 12670328.

11. Franchini M, Gandini G, Di Paolantonio T, Mariani G. Acquired hemophilia: a concise review. Am J Hematol. 2005; 80:55–63. PMID: 16138334.
12. Park EK, Jang JS, Park SY, Lee SJ. Two patients with acquired hemophilia successfully treated with combination therapy including therapeutic plasmapheresis. Korean J Med. 2009; 77:367–370.
14. Brown SGA, Caruso N, Borland ML, McCoubrie DL, Celenza A, Isbister GK. Clotting factor replacement and recovery from snake venom-induced consumptive coagulopathy. Intensive Care Med. 2009; 35:1532–1538. PMID: 19547954.

15. Ferguson LA, Morling A, Moraes C, Baker R. Investigation of coagulopathy in three cases of tiger snake (Notechis ater occidentalis) envenomation. Pathology. 2002; 34:157–161. PMID: 12009098.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download