1. Barritt DW, Jordan SC. Anticoagulant drugs in the treatment of pulmonary embolism: a controlled trial. Lancet. 1960; 1:1309–1312. PMID:
13797091.
2. Kearon C, Kahn SR, Agnelli G, et al. Antithrombotic therapy for venous thromboembolic disease: american college of chest physicians evidence-based clinical practice guidelines (8th Edition). Chest. 2008; 133(6 Suppl):454S–545S. PMID:
18574272.
3. Büller HR, Davidson BL, Decousus H, et al. Fondaparinux or enoxaparin for the initial treatment of symptomatic deep venous thrombosis: a randomized trial. Ann Intern Med. 2004; 140:867–873. PMID:
15172900.
4. Büller HR, Davidson BL, Decousus H, et al. Subcutaneous fondaparinux versus intravenous unfractionated heparin in the initial treatment of pulmonary embolism. N Engl J Med. 2003; 349:1695–1702. PMID:
14585937.

5. Konstantinides S, Geibel A, Heusel G, et al. Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism. N Engl J Med. 2002; 347:1143–1150. PMID:
12374874.

6. Torbicki A, Perrier A, Konstantinides S, et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the task force for the diagnosis and management of acute pulmonary embolism of the european society of cardiology (ESC). Eur Heart J. 2008; 29:2276–2315. PMID:
18757870.
7. Lee AY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003; 349:146–153. PMID:
12853587.

8. Meyer G, Marjanovic Z, Valcke J, et al. Comparison of low-molecular-weight heparin and warfarin for the secondary prevention of venous thromboembolism in patients with cancer: a randomized controlled study. Arch Intern Med. 2002; 162:1729–1735. PMID:
12153376.
9. Hull RD, Pineo GF, Brant RF, et al. Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. Am J Med. 2006; 119:1062–1072. PMID:
17145251.

10. White RH. The epidemiology of venous thromboembolism. Circulation. 2003; 107:I4–I8. PMID:
12814979.

11. Palareti G, Cosmi B, Legnani C, et al. D-dimer testing to determine the duration of anticoagulation therapy. N Engl J Med. 2006; 355:1780–1789. PMID:
17065639.

12. Cosmi B, Legnani C, Tosetto A, et al. Usefulness of repeated D-dimer testing after stopping anticoagulation for a first episode of unprovoked venous thromboembolism: the PROLONG II prospective study. Blood. 2010; 115:481–488. PMID:
19965693.

13. Eichinger S, Minar E, Bialonczyk C, et al. D-dimer levels and risk of recurrent venous thromboembolism. JAMA. 2003; 290:1071–1074. PMID:
12941680.

14. Prandoni P, Lensing AW, Prins MH, et al. Residual venous thrombosis as a predictive factor of recurrent venous thromboembolism. Ann Intern Med. 2002; 137:955–960. PMID:
12484710.

15. Siragusa S, Malato A, Anastasio R, et al. Residual vein thrombosis to establish duration of anticoagulation after a first episode of deep vein thrombosis: the Duration of Anticoagulation based on Compression UltraSonography (DACUS) study. Blood. 2008; 112:511–515. PMID:
18497320.

16. Prandoni P, Prins MH, Lensing AW, et al. Residual thrombosis on ultrasonography to guide the duration of anticoagulation in patients with deep venous thrombosis: a randomized trial. Ann Intern Med. 2009; 150:577–585. PMID:
19414836.

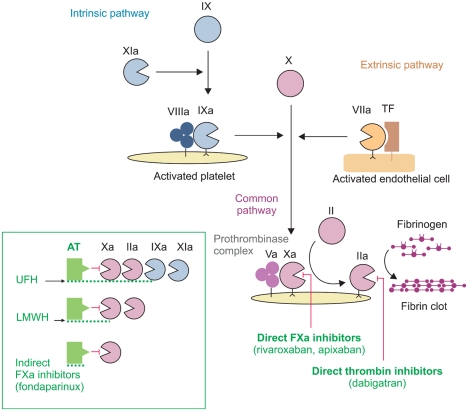
17. Turpie AGG. Oral, direct Factor Xa inhibitors in development for the prevention and treatment of thromboembolic diseases. Arterioscler Thromb Vasc Biol. 2007; 27:1238–1247. PMID:
17379841.

18. Weitz JI, Hirsh J, Samama MM. New antithrombotic drugs: American college of chest physicians evidence-based clinical practice guidelines (8th Edition). Chest. 2008; 133:234S–256S. PMID:
18574267.
19. European public assessment report: Pradaxa. 2008. Accessed January 10, 2010. London: European Medicines Agency (EMEA);
http://www.emea.europa.eu.
20. Schulman S, Kearon C, Kakkar AK, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009; 361:2342–2352. PMID:
19966341.

21. Kubitza D, Becka M, Voith B, Zuehlsdorf M, Wensing G. Safety pharmacodynamics and pharmacokinetics of single doses of BAY 59-7939, an oral, direct factor Xa inhibitor. Clin Pharmacol Ther. 2005; 78:412–421. PMID:
16198660.

22. Eriksson BI, Quinlan DJ, Weitz JI. Comparative pharmacodynamics and pharmacokinetics of oral direct thrombin and factor Xa inhibitors in development. Clin Pharmacokinet. 2009; 48:1–22. PMID:
19071881.
23. Kubitza D, Becka M, Wensing G, Voith B, Zuehlsdorf M. Safety pharmacodynamics and pharmacokinetics of BAY59-7939-an oral, direct Factor Xa inhibitor-after multiple dosing in healthy male subjects. Eur J Clin Pharmacol. 2005; 61:873–880. PMID:
16328318.
24. European public assessment report: Xarelto. 2008. Accessed January 10, 2010. London: European Medicines Agency (EMEA);
http://www.emea.europa.eu.
25. Agnelli G, Gallus A, Goldhaber SZ, et al. Treatment of proximal deep-vein thrombosis with the oral direct factor Xa inhibitor rivaroxaban (BAY59-7939): the ODIXa DVT (oral direct factor Xa inhibitor BAY59-7939 in patients with acute symptomatic deep-vein thrombosis) study. Circulation. 2007; 116:180–187. PMID:
17576867.
26. Buller HR, Lensing AW, Prins MH, et al. A dose-ranging study evaluating once-daily oral administration of the factor Xa inhibitor rivaroxaban in the treatment of patients with acute symptomatic deep vein thrombosis: the Einstein-DVT Dose-Ranging Study. Blood. 2008; 112:2242–2247. PMID:
18621928.

27. Buller HR. Once daily oral rivaroxaban versus placebo in the long term prevention of recurrent symptomatic venous thromboembolism. The Einstein-Extension study. Blood. 2009; 114:Abstract 2.[U01].
28. Wong PC, Crain EJ, Xin B, et al. Apixaban, an oral, direct and highly selective factor Xa inhibitor: in vitro, antithrombotic and antihemostatic studies. J Thromb Haemost. 2008; 6:820–829. PMID:
18315548.
29. Wang L, Zhang D, Raghavan N, et al. In vitro assessment of metabolic drug-drug interaction potential of apixaban through cytochrome P450 phenotyping, inhibition, and induction studies. Drug Metab Dispos. 2010; 38:448–458. PMID:
19940026.

30. Buller H, Deitchman D, Prins M, et al. Efficacy and safety of the oral direct facto Xa inhibitor apixaban for symptomatic deep vein thrombosis. The Botticelli DVT dose-ranging study. J Thromb Haemost. 2008; 6:1313–1318. PMID:
18541000.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download