Dear Editor:
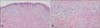
A 41-year-old Japanese man presented in October 2013 with a 2-week history of pruritic, erythematous papules. He had diabetes mellitus, hyperlipidemia, and hypertriglyceridemia, but had stopped treatment 5 years prior to this visit. He also suffered from acute pancreatitis, and was admitted to the Department of Medicine, Japan Community Healthcare Organization Osaka Hospital, 1 day prior. Topical steroid ointment prescribed during a previous visit to another clinic was ineffective for the treatment of the papules. At the time of consultation, he presented with multiple, approximately 5-mm, pruritic, yellowish, erythematous papules on the trunk and extensor surfaces of the extremities (Fig. 1A). Dermoscopic examination of the papules clearly revealed granular yellowish characteristics (Fig. 1B). The laboratory findings (normal values are in parentheses) were: white blood cell count, 13.3×103 (4.0×103~8.5×103)/µl; neutrophils, 83.5% (38%~58%); alkaline phosphatase, 369 (115~359) U/L; C reactive protein, 5.91 (<0.3) mg/dl; hemoglobin A1c, 9.2% (4.6%~6.2%); amylase, 340 (40~130) IU/L; lipase, 960 (11~53) U/L; triglyceride, 6,784 (30~150) mg/dl; total cholesterol, 803 (130/219) mg/dl; high density lipoprotein cholesterol, 12 (42~74) mg/dl; low density lipoprotein cholesterol, 23 (70~140) mg/dl; remnant-like lipoprotein particle cholesterol, 84.4 (<7.5) mg/dl; apolipoprotein (Apo) A-I, 89 (119~155) mg/dl; Apo A-II, 12.6 (25.9~35.7) mg/dl; Apo B, 135 (73~109) mg/dl; Apo E, 11.0 (2.7~4.3) mg/dl; Apo C-II, 16.5 (1.8~4.6) mg/dl; Apo C-III, 28.3 (5.8~10.0) mg/dl. A skin biopsy sample obtained from papules on the waist revealed foamy cells that infiltrated the dermis. At higher magnification, foamy cells and extracellular lipids were present (Fig. 2). Therefore, we diagnosed the patient as having eruptive xanthoma with type V hyperlipoproteinemia according to Fredrickson's classification of hyperlipoproteinemias. We treated the acute pancreatitis with fasting, nafamostat mesilate, and ulinastatin, and the hypercholesterolemia with bezafibrate. The acute pancreatitis improved 16 days after admission. Serum triglyceride and total cholesterol values decreased to within normal range 1.5 months after the initiation of treatment. The eruptive xanthoma lesions rapidly resolved as the hyperlipidemia improved.
Hyperlipidemia is divided into six subgroups. Cutaneous xanthomatous lesions can occur in all six types of hyperlipidemia1. Cutaneous xanthomas can be divided into subgroups, including eruptive xanthomas, tuberous xanthomas, tendon xanthomas, xanthelasmata, and plane xanthomas2. Eruptive xanthomas can be associated with hypertriglyceridemia (Type I, IV, or V hypercholesterolemia), particularly when diabetes is poorly controlled23. Eruptive xanthomas contain more triglycerides and fewer cholesteryl esters than other types of xanthomas, and lipids present in xanthomas are derived from circulating plasma lipoproteins. Triglyceride is mobilized more rapidly than cholesterol, so resolving eruptive xanthomas are rich in cholesterol4. Hypertriglyceridemia also increases the risk of acute pancreatitis, and the risk of eruptive xanthoma and pancreatitis increases when the serum triglyceride concentration reaches the thousands5. Eruptive xanthomas manifested in this patient 2 weeks before his visit, followed by acute pancreatitis. Dermatologists should carefully consider the possibility of acute pancreatitis with hypertriglyceridemia in eruptive xanthoma patients.
Figures and Tables
Fig. 1
(A) Clinical appearance and (B) dermoscopic appearance of multiple yellowish erythematous papules on the patient's back in October 2013.

Fig. 2
Skin biopsy from the erythematous papules present on the patient's waist. (A) At lower magnification, numerous pale areas containing foamy cells infiltrate the dermis, especially the upper dermis and perivascular areas (H&E, ×40). (B) At higher magnification, foamy cells with extracellular lipids are present (×200).
References
1. Beaumont JL, Carlson LA, Cooper GR, Fejfar Z, Fredrickson DS, Strasser T. Classification of hyperlipidaemias and hyperlipoproteinaemias. Bull World Health Organ. 1970; 43:891–915.
3. Ladizinski B, Lee KC. Eruptive xanthomas in a patient with severe hypertriglyceridemia and type 2 diabetes. CMAJ. 2013; 185:1600.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download