INTRODUCTION
Touraine-Soulente-Golé (TSG) Syndrome or primary hypertrophic osteoarthropathy (PHO) is a genodermatosis characterized by digital clubbing of hands and feet, enlargement of extremities, secondary to bones and periarticular tissue proliferation. There is bilateral ptosis, leonine facies, and skin thickening along with joint pains. It is PHO of a presumable autosomal dominant inheritance with mainly variable expression and incomplete penetrance. Although recessive autosomal inheritance and x-linked mutations may also be present, these may differ in severity and prevalence of clinical features1. Secondary form of diseases can occur in association with other diseases like Pulmonary: Bronchogenic carcinoma, nasopharyngeal carcinoma, bronchiectasis, abscess, emphysema, metastasis, mesothelioma, cystic fibrosis; Cardiac: Congenital heart disease, aortic or axillary artery graft rejection and gastrointestinal tract: Crohn's disease, ulcerative colitis, polyps, biliary atresia, biliary cirrhosis, biliary neoplasm and esophageal carcinoma2.
CASE REPORT
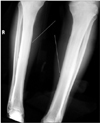
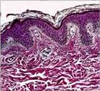
A 27-year-old male came with complaints of repetitive wrinkling and thickening of skin on face and scalp along with broadening of hands since 8 years ago. He also complained of increased oiliness on the face. This healthy Indian male with normal physique and intelligence level was the 1st son of non-consanguineous parents, his elder brother was 31. He has a 3 years old son and a 5 years old daughter. Family history was unremarkable. History of joint pains, oral and genital ulceration, hoarseness of voice, epistaxis and sensory loss was denied. No similar history was found in the family. Physical examinations revealed scalp skin was folded, giving appearance of peculiarity cutis verticis gyrata (Fig. 1), whereas the hair growth appeared normal. Eyebrows appeared dense. Skin over face was thickened, non-pinchable, greasy to touch and folded, giving appearance of leonine faces (Fig. 2). Follicular openings were prominent and so were the video-dermoscopy. In addition, clubbing of fingers and toes was presented along with broadening of hands and fingers (Fig. 3). Cutaneous examination over the rest of his body including mucosae was normal. Laboratory investigations included growth hormone assay, thyroid profile, and Venereal Diseases Research Laboratory Assay and were found to be within normal limits. Erythrocyte sedimentation rate was elevated (45 mm in 1st hour). Serum calcium, alkaline phosphatase and other biochemical tests were also within normal limits. Smears for lepra bacilli were negative. Radiological investigations included radio-graphs' of skull, which were normal including sella turcica. Long bones of legs showed minimal periosteal reaction along the shaft (Fig. 4) and his feet showed evidence of cortical erosions and tufting ends of terminal phalanges. Histopathological examination from skin behind ear lobule showed a hyperplastic epidermis and dermis (Fig. 5). On the basis of history, clinical features, radiological and lab findings, the diagnosis of TSG syndrome was formulated.
DISCUSSION
TSG syndrome, which is a rare disease, precise incidence of which is not known, with approximately estimated prevalence 0.16%3. TSG syndrome accounts for 3~5% of all cases of hypertrophic osteoarthropathy and occurs predominantly in men (80%), in which severe phenotype is observed4. Pathogenesis is not fully clear. Biopsy of skin and bone marrow may show an exacerbated proliferation of fibroblasts, which are associated with diffused epidermal hyperplasia and lymphohistiocytic infiltration with collagen redistribution. Studies have shown a circulating connective tissue growth modulator, increase in plasmatic substances including osteocalcin, endothelin-1, β-tromboglobulin, PDGF, v W factor, VEGF and dermal acid mucopolysaccharide of ground substance5,6. Increased steroid receptors concentration in these patients suggest an increase in tissue sensitivity to circulating sex hormones7. One study showed TSG syndrome mapped to band 4q33-q34 and mutation in HPGD, encoding 15-hydroxyprostaglandin dehydrogenase, the main enzyme of prostaglandin degradation8. The clinical condition typically begins in adolescence and manifest variably depending on the presentations. Touraine et al.9 described 3 forms of syndrome: Complete (pachydermia and periostitis), Incomplete (with periostitis and no pachydermia), and Forme fruste (pachydermia with minimal or absent periostitis). Characteristic cutaneous changes are pachydermia i.e. thickening of facial skins resulting in leonine faces, over scalp, cutis verticis gyrata, and over the eyes blephroptosis10. These changes give a characteristic known as 'bull dog appearance'. Other influences are acne, eczema, seborrhea, palmoplanter hyperhydrosis, burning sensation of hands and feet, clubbing of fingers with or without paronychial thickening. Skeletal and radiological changes are symmetrical and irregular subperiosteal deposits in metaphysis and epiphysis of long bones especially in the forearm and leg, and small bones, widening ends of long bones especially wrist and knee, enlargement of distal part of digits with resorption of phalanges and acro-osteolysis, calcification of ligaments and interosseous membranes, cortical thickening with or without narrowing of medullary cavity, enlargement of paranasal sinuses4,11-13. There is joint effusion, inflammation and reduction of joint spaces, contractures in late stages and rarely periarticular erosion14. In axial skeleton, changes are spondylolithiasis, with narrowing of intervertebral disc spaces and foramina, ligamentous ossification and laxity4. Differential diagnoses are secondary hypertrophic osteoarthropathy, thyroid acropachy, acromegaly, van Buchem's disease, diaphyseal dysplasia and syphilitic periostitis. There is no specific treatment for the condition. Surgical management includes plastic surgery and correction of associated bony deformities15-17. Medical treatment includes non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, tricyclic antidepressants, resedronate, and pamidronate and tamoxifen citrate to control arthritis. Due to heterogeneity in transmission of TSG and difficulty of genetic tests, guidance to these patients is often complicated13. Such disease runs insidiously and chronically for about a decade with phases of exacerbations and asymptomatic periods stabilizing spontaneously13. Disabilities may be left-sided kyphosis, restricted motions and neurological complications which may occur later. However, it usually doesn't interfere with patient's life expectancy18.
Current clinical and radiological findings favor the 3rd type diagnosis, the forme fruste of TSG syndrome in our case. Other family members were also advised for clinico-radiological examinations. Patient was referred to plastic surgery department for the improvement of cosmetic appearance. As the condition is amenable to treatment, prognosis depends mostly upon the extent of joint involvements and periarticular periosteal thickening. Detailed investigation and early diagnosis may help in prevention of disabilities later in life.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download