Abstract
Objectives
In order to adopt and activate telemedicine it is necessary to survey how medical staff, who are providers of medical service, and consumers, who are the service targets, perceive information and communication technology (ICT)-based healthcare service.
Methods
This study surveyed the awareness and acceptability of ICT-based healthcare by involving service targets, specifically workers and students living in the Seoul and Gyeonggi regions who are consumers of healthcare service. To determine the correlation among awareness of ICT-based healthcare, the need for self-management, and acceptability, this study conducted a correlation analysis and a simple regression analysis.
Results
According to the responses to the questions on the need for ICT-based healthcare service by item, blood pressure (n = 279, 94.3%) and glucose (n = 277, 93.6%) were revealed to be the physiological signal monitoring area. Among the six measurement factors affecting ICT-based healthcare service acceptability, age, health concerns, and effect expectation had the most significant effects. As effect expectation increased, acceptability became 4.38 times higher (p < 0.05).
Conclusions
This study identified a positive awareness of service targets on ICT-based healthcare service. The fact that acceptability is higher among people who have family disease history or greater health concerns may lead to service targets’ more active participation. This study also confirmed that a policy to motivate active participation of those in their 40s (who had high prevalence rates) was needed.
As medical service paradigm has shifted from disease treatment to disease prevention, interest in information and communication technology (ICT)-based healthcare, through which medical service can be received without time and space restrictions, has increased. ICT-based healthcare is characterized by the following: first, wired/wireless network ICT is used, and second, medical service to determine one’s health state or to provide treatment can be offered anywhere and anytime. Such a medical service is called telemedicine or u-Health (all these are ICT-based healthcare services) [1].
As a recent technological change in medical service, the evolution of IoT-Cloud Big data-Mobile (ICDBM) has enabled real time and intelligent customized services and leads the innovation in the medical service field. Various research on linking different types of technologies, such as artificial intelligence, wearables, and robots, as well as ICDBM, have been carried out recently [2].
Business Insider (BI) Intelligence projects that the size of the global wearable device market will reach US$ 14 billion in 2018 [3], while Gartner predicted that the global IoT market will reach US$ 309.0 billion in 2020 and that healthcare will take up the highest ratio at 15% of the IoT market [4]. Cisco Systems, Inc. forecasted that a value creation of US$ 1 trillion, particularly US$ 106.0 billion in value creation in the patient care sector, will be made with the healthcare industry’s IoT application in 2020 [5]. McKinsey estimated US$ 1.6 trillion in value creation in 2025 [6]. The competition to secure healthcare platforms among ICT companies or in the ICT industry has become fierce at home and abroad, and many companies have released relevant products and medical services, with Nike+ Fuelband and Fitbit being representative cases. Cases related to medical diagnosis-assisting service are NuVant and Triggerfish [7]. In Korea, the demand for IT utilizing services increased according to the increase in the introduction of the Internet, mobile gadgets, and smart devices [8]. In spite of a pre-announcement of legislation on telemedicine, centered on local hospitals in October 2013 and June 2016, the identification of the medical service area addressing the need of medical service providers and targets, along with the identification of its marketability status, has not been sufficiently conducted [910].
ICT-based healthcare service is projected to generate positive results in the healthcare market through treatment result improvement, medical service expenditure reduction, and patients’ active participation [11]. Nonetheless, ICT-based healthcare is closely related to life in a broad sense, and there is an opinion that the acceptance of relatively innovative ICT-based healthcare can be negative or delayed [12]. Awareness of telemedicine is low, and so is the intention to use it [13]; therefore, there is a need to determine how the medical staff, who are the providers of medical service, and the consumers, who are the service targets, perceive ICT-based healthcare service in order to adopt and activate telemedicine.
Concerning existing domestic and international studies on ICT-based healthcare service, various studies including doctors’ positive or negative effects, usage effects and usage satisfaction have been conducted [141516]. However, studies on consumers’ acceptability of ICT-based healthcare service are insufficient. In this study, the factors affecting service targets’ awareness, use, or acceptability of ICT-based healthcare were examined. This study presents measures to induce the adoption and activation of service targets’ active ICT-based healthcare service.
This study surveyed the awareness and acceptability of ICT-based healthcare by involving service targets, specifically workers and students living in the Seoul and Gyeonggi regions who were consumers of healthcare. The distribution and collection of the questionnaires were carried out from May to June 2016. A total of 379 questionnaire copies were distributed, 296 were statistically analyzed with the other 83 excluded for incomplete answers (24 copies) and service provider (59 copies). This survey has passed through the Institutional Review Board approval procedure.
The survey tool (questionnaire) was divided into Sociodemographic variables (10 questions) and the four following areas: health concerns, 7 questions; coverage areas and required populations, 36 questions; self-management necessity, 6 questions; acceptability, 4 questions.
All items were rated using a 7-point Likert scale from ‘not required at all’ to ‘very much required’.
As Socio-demographic variables (10 questions), the region, gender, age, occupational group, family history, accessibility to hospitals, device (cellphone)-based healthcare use of the samples were surveyed.
The occupational group was divided into a health related occupational group, (i.e., pharmaceutical company employees and health-related public officials), non-health related occupational group (general company employees and other public officials), and student and general people (students, homemakers, and unemployed people).
Concerning the family history, the participants with lineal family members who had had continuous drug administration and treatment due to chronic diseases, and the chronic diseases concerned were also surveyed.
Health concerns (7 questions) were measured through the compliance (fidelity) of health-related habits. The questions included “I exercise regularly,” and “I receive physical examinations periodically,” which measured the participants’ interest in health.
This study surveyed the coverage area requiring ICT-based healthcare (16 questions). It was divided into a physiological signal acquisition area and an alert and remind area: the physiological signal acquisition area included body temperature measurement, blood pressure and glucose checks. The alert and remind area included medication time, time to exercise, and sleep duration.
This study surveyed the population requiring ICT-based healthcare (20 questions). The required population was divided into an age cluster and a status cluster. The age cluster was classified into infant, teens, 20s, and 50 or over. Regarding the status cluster, a self-survey on necessity according to the status and situation of pregnant women, the elderly living alone, and diabetics was undertaken.
For the socio-demographic variable of the participants acquired through the questionnaire responses, this study calculated frequency (n) and percentage (%) through a technical statistics frequency analysis. To determine the correlation among awareness of ICT-based healthcare, the need for self-management, and acceptability, this study conducted a correlation analysis and a multi-regression analysis. To determine the differences between the need for self-management and acceptability according to the sociodemographic variable, a t-test and ANOVA were carried out. Lastly, this study conducted a logistic regression analysis to determine the factors affecting the acceptability of ICT-based healthcare. SPSS ver. 23.0 software (IBM, Armonk, NY, USA) was used, and a statistical significance was defined as a p-value less than 0.05.
The general characteristics of the participants in this study are shown in Table 1. As regards gender, there were 161 male participants (54.4%) and 125 female participants (42.2%). As for distribution according to age, 122 people were younger than 30 years (minimum age, 18 years) (41.2%), 69 people were 30–39 (23.3%), 70 people were 40–49 (23.6%), and 26 people were 50 or over (8.8%).
According to occupational groups, 69 people (18.2%) were surveyed in health related group (pharmaceutical company employees and health-related public officials), 110 people (29.0%) were surveyed in the non-health related group (general company employees and other public officials), and 117 people (30.9%) were surveyed to belong to general people (including students).
Of those surveyed, 149 people (50.3%) had a family history for chronic diseases, and 143 people (48.3%) did not have such a history; 87 people (29.4%) had experience in ICT-based healthcare, and 208 people (70.3%) did not have such experience; 249 people (84.1%) said they were within 30 minutes of access to a hospital, and 46 people (15.5%) said they were more than 30 minutes from a hospital (Table 1).
The survey results of medical service targets’ opinions on ICT-based healthcare were as follows:
Concerning the responses in the physiological signal acquisition area, blood pressure check (n = 279, 94.3%) and blood glucose check (n = 277, 93.6%) were revealed. In the alert area, obesity (n = 273, 92.2%) and health problem alarm (n = 274, 92.6%) were revealed.
Upon looking at the age-related cluster in potential group that needed ICT-based healthcare, 288 people 97.3%) were surveyed to be 50 years old or over, and 236 people (79.7%) were infants.
Upon looking at the status-related cluster, 289 people (97.6%) were diabetics and heart disease patients, 286 people (96.6%) were seniors living alone.
To determine differences in the need for self-management and acceptability of ICT-based healthcare according to service targets’ socio-demographic variable, the t-test and ANOVA were carried out (Table 2).
The need of self-management of the participants who said that their health concerns were low was 5.49 on average in the Likert scale score and 5.77 on average for the patients who said that their health concerns were high. Therefore, the patients with high health concerns were found to have higher need for self-management (p = 0.015). The mean score of ICT-based healthcare acceptability of the participants without family history for chronic diseases was 4.10, and that of the participants with family disease history was 4.50. The acceptability of the participants with family history was higher and was statistically significant (p = 0.016).
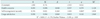
The correlation coefficient between health concerns and self-management necessity was 0.210 (p = 0.000), and the correlation coefficient between health concerns and acceptability was 0.198 (p = 0.001); therefore, there were positive correlations.
The correlation coefficient between usage satisfaction of devices and health concerns was 0.249, while the significance probability was 0.003; therefore, there was a strong positive correlation. The correlation coefficient between self-management necessity and acceptability was 0.322, while the significance probability was 0.000. Therefore, as self-management necessity became higher, acceptability also became higher (Table 3).
As a result of multi-regression analysis concerning the effect on ICT-based healthcare acceptability, the self-management necessity (p = 0.002) had a significant effect on acceptability (Table 4). As self-management necessity became higher (B = 0.376), so did acceptability become higher. The explanation power of the self-management necessity, usage satisfaction and acceptability was 8.3%.
To determine the factors affecting acceptability, this study carried out a binominal logistic regression analysis (Table 5). Among the seven measurement factors affecting ICT-based healthcare service acceptability, effect expectation about devices had the most significant effects.
The acceptability of the service targets with high effect expectation about a device was 4.4 times higher (p < 0.05) than that of the service targets with low effect expectation (Table 6).
This study surveyed the awareness of service targets on ICT-based healthcare service for prevention-centered medical service, which as attracting attention in the healthcare market. Furthermore, the factors affecting acceptability and that can generate positive effects to service targets for the activation of telemedicine were analyzed. Based on the results, this study presents directions for ICT-based healthcare service activation.
First, ICT-based healthcare service is a solution for chronic patients and the aging society. If telemedicine is actively carried out between patients and doctors through ICT, personally customized service and prevention service can be offered through temporal and spatial expansions of medical service, which will be greatly advantageous to all concerned [1117]. Upon looking at the survey result of service targets’ awareness of ICT-based healthcare, first, the demand on physiological signal measurement including 279 people (94.3%) for blood pressure, 277 people (93.6%) for glucose, and 273 people (92.2%) for obesity was high in the desired coverage areas. As for the group requiring the use of service, the need appears higher among chronic patients and aged people or among 289 people (97.6%) with diabetes, heart disease and hypertension.
Second, based on the survey, family history of disease and health concerns were found to be factors affecting acceptability. Therefore, there is a need to focus on the ICT-based healthcare service targeting those factors [18]. As a result of surveying service targets’ personal characteristics according to acceptability, the significance probability of family history of disease and health concerns were 0.016 and 0.002, respectively; thus, the result was significant. Those who had a high degree of health concerns and a family history of chronic diseases felt more of a need for the service. In a previous study, those who were interested in healthcare showed participation intention to overcome difficulties in the process of using ICT-based healthcare service face-to-face, and an in-depth survey targeting those who were offered the ICT-based healthcare service within a national project [19]. For patients with chronic diseases or the elderly, continuous self-management is needed [20]. In fact, if self-management service based on the medical service provider’s professional guide and care is carried out, the optimal effect can be generated [2122].
Third, a policy to concentrate on ICT-based healthcare for those in their 40s is necessary. As a result of looking at acceptability difference by age groups, the differences were not statistically significant, but people in their 40s had a higher acceptability than those in their 20s and 50 or over. This means that those in their 40s are in the period in which health concerns become high, and they can use services like ICT-based technology relatively without burden, compared to other age groups. Furthermore, the 40s age group seems to be the age group that has the intention to participate in the ICT-based healthcare [2324]. According to the 2014 data of Statistics Korea, the prevalence rates become high starting from those in their 40s, given that high blood pressure patients rose from 7.3% in their 30s to 17.7% in their 40s, whereas cholesterolemia rose from 6% among those in their 30s to 12.6% among those in their 40s [25]. Concerning the death rate due to neoplasm (cancer), it became higher from 10.2% among those between 30 and 34 to 19.9% among those between 35 and 40, to 35.4% among those between 40 and 44, and 63.7% among those between 45 and 49. This data suggests that concentrated care for healthcare and prevention should start in full-swing among those in their 40s, when aging starts in earnest. Therefore, it is desirable to focus on people in their 40s, while ICT-based healthcare service encompasses chronic disease patients and elderly people.
The conclusion of this study is as follows: As a result of the service target’s views on ICT-based healthcare, continuous care was surveyed to be necessary for chronic diseases such as diabetes, heart disease, and hypertension and for the age group of 50 or over. The mean acceptability of the service target with high health concerns and family history of disease was high in this study. Acceptability became higher, as self-management necessity and usage satisfaction were higher.
The study had a weakness in that the consensus on telemedicine was not ensured, and threats on institutional problems such as personal information protection and relevant regulations exist in the ICT-based healthcare service. However, the strength is that patients can actively participate and have opportunities for treatment result improvement and medical service expense reduction, which is projected to bring about positive results to the healthcare market. Through this study, a positive awareness of service targets on ICT-based healthcare service was identified. The fact that acceptability is higher for persons with a family history of disease and higher health concerns may lead to service targets’ active participation. This study drew a result that a policy for the prevention and motivation for active participation for those in their 40s (who had high prevalence rates) was needed. If an analysis is conducted by expanding the ICT-based healthcare service target to those having actual experience of the service and by extensively segmenting the acceptability and effects, the study is expected to more clearly contribute to ICT-based healthcare service design.
Figures and Tables
Table 3
Self-management necessity and acceptability about ICT-based healthcare by study participants
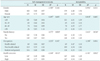
Table 4
Correlation coefficient of health concerned, self-management necessity, usage satisfaction and acceptability

Acknowledgments
This study was supported by the National R&D Program for Cancer Control, Ministry of Health & Welfare of Korea (1420210) and funded by the Ministry of Science, ICT & Future Planning (NRF-2010-0023700).
References
1. Korea Health Industry Development Institute. Weekly healthcare industry trend report. Seoul: Korea Health Industry Development Institute;2015. p. 159.
2. National Information Society Agency. IT & future strategy report. Seoul: National Information Society Agency;2015.
3. Korea Health Industry Development Institute. Digital healthcare platform and business trends. Seoul: Korea Health Industry Development Institute;2014.
4. Fenn J, Raskino M. Gartner’s hype cycle special report for 2013. . Stamford (CT): Gartner Inc.;2013.
5. Bradley J, Barbier J, Handler D. Embracing the Internet of everything to capture your share of $14.4 trillion. San Jose (CA): Cisco Systems Inc.;2013.
6. Bughin J, Manyika J, Woetzel J, Chui M, Bisson P, Dobbs R. The Internet of Things: mapping the value beyond the hype. Washington (DC): McKinsey Global Institute;2015.
7. Lee NY, Yoo HS, Lee SH, Kwon OB. U-healthcare service for psychological wellbeing lifecare. Korean J Bus Adm. 2012; 25(8):3397–3415.
8. Kim JK, Kim JH, Park DK, Lee YH. U-health platform based health management service model using context information. J Digit Converg. 2012; 10(8):185–192.
9. Lee HM. A study on the acceptance of wearable computers based on the extended technology acceptance model. Res J Costume Cult. 2009; 17(6):1155–1172.

10. Yun JL. Introduction of creative ICT R&D trends. J Korean Inst Inf Sci Eng. 2015; 33(1):4–5.
11. RBC Capital Markets. The RBC Capital Markets Consumer Health & Information Technology Survey: the 'wearable' issue [Internet]. New York (NY): RBC Capital Markets;2015. cited at 2016 Oct 24. Available from: https://healthmanagementacademyin-public.sharepoint.com/attachmentsexternal/publications/The_RBC_Capital_Markets_Consumer_Health_Information_Technology_Survey2015-07-13.pdf.
12. TechRepublic. IBM Watson Health computes a pair of new solutions to improve healthcare data and security [Internet]. [place unknown]: TechRepublic;2015. cited at 2016 Oct 24. Available from: http://www.techrepublic.com/article/ibm-watson-health-computes-a-pair-of-new-solutions-to-improve-healthcare-data-and-security/.
13. Cho HS, Koh DY. U-health service customer awareness and development. Sejong: Korea Institute for Industrial Economics & Trade;2011.
14. Varkey P, Schumacher K, Swanton C, Timm B, Hagen PT. Telemedicine in the work site: a study of feasibility, and patient and provider satisfaction. J Telemed Telecare. 2008; 14(6):322–325.

15. Whitten P, Doolittle G, Mackert M. Providers' acceptance of telehospice. J Palliat Med. 2005; 8(4):730–735.

16. Noh MJ, Park SC, Youn KI. The effects of consumer characteristics on the intention to use u-healthcare services. Korean J Hosp Manag. 2010; 15(4):27–42.
17. Jeong YG. Improvement on telemedicine regulations. Mag IEEK. 2016; 43(2):50–58.
18. Lee Y, Moon M. Utilization and content evaluation of mobile applications for pregnancy, birth, and child care. Healthc Inform Res. 2016; 22(2):73–80.

19. Choi H, Kim J. Low-income elders’ experiences in using u-health (ubiquitous healthcare) services. J Korean Acad Community Health Nurs. 2014; 25(4):270–281.

20. Lee YK, Park JY, Rho MJ, Wang BR, Choi IY. Doctors' perception and intention of the u-healthcare service. J Korea Contents Assoc. 2012; 12(2):349–357.

21. Kim H, Jo J, Choi Y, Oh J, Lee J, Yoon K. Ubiquitous health care system for chronic disease management. J Korean Inst Commun Sci. 2010; 27(9):3–8.
22. Choi EH, Seo JY. u-Health for management of chronic diseases: physical activity and therapeutic exercise. J Korean Med Assoc. 2009; 52(12):1154–1163.

23. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010; 79(11):736–771.

24. Song TM, Lee SY, Lee KS, Park DS, Jin DR. U-health: current status and tasks ahead. Seoul: Korea Institute for Health and Social Affairs;2011.
25. Statistics Korea. 2014 Causes of death statistics [Internet]. Daejeon: Statistics Korea;2015. cited at 2016 Oct 1. Available from: http://kostat.go.kr/portal/korea/kor_nw/3/index.board?bmode=read&aSeq=348541.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download