Abstract
Objectives
The purposes of this study were to examine the predictive validity of the Cubbin and Jackson pressure ulcer risk assessment scale for the development of pressure ulcers in intensive care unit (ICU) patients retrospectively and to evaluate the reusability of Electronic Medical Records (EMR) data.
Methods
A retrospective design was used to examine 829 cases admitted to four ICUs in a tertiary care hospital from May 2010 to April 2011. Patients who were without pressure ulcers at admission to ICU, 18 years or older, and had stayed in ICU for 24 hours or longer were included. Sensitivity, specificity, positive predictive value, negative predictive value, and area under the curve (AUC) were calculated.
Results
The reported incidence rate of pressure ulcers among the study subjects was 14.2%. At the cut-off score of 24 of the Cubbin and Jackson scale, the sensitivity, specificity, positive predictive value, negative predictive value, and AUC were 72.0%, 68.8%, 27.7%, 93.7%, and 0.76, respectively. Eight items out 10 of the Cubbin and Jackson scale were readily available in the EMR data.
Conclusions
The Cubbin and Jackson scale performed slightly better than the Braden scale to predict pressure ulcer development. Eight items of the Cubbin and Jackson scale except mobility and hygiene can be extracted from the EMR, which initially demonstrated the reusability of EMR data for pressure ulcer risk assessment. If the Cubbin and Jackson scale is a part of the EMR assessment form, it would help nurses perform tasks to effectively prevent pressure ulcers with an EMR alert for high-risk patients.
Pressure ulcers cause patients' pain and discomfort as well as other physical, psychosocial, and financial problems, such as the inevitability of operation, infection, and sepsis, disability and dependency, and thus, increased medical expenses and mortality [1,2]. Although there is a lack of reports regarding the medical cost of pressure ulcer in South Korea, pressure ulcers cost 9.1 billion to 11.6 billion dollars per year in the United States [2]. And the total treatment cost of pressure ulcers in the UK is 1.4 to 2.1 billion pounds annually and that was 4% of the total National Health Service expenditure in 2004, and 90% of this cost was related to nursing service time as the cost increased with ulcer grade because the time to treat became longer due to complications [3].
The occurrence of pressure ulcers during hospitalization is a significant patient safety indicator [4] and a nursing-sensitive outcome [5,6]. The criteria for evaluating healthcare institutions mandated by the Ministry of Health & Welfare and the Korea Institute for Healthcare Accreditation [7] also included pressure ulcer prevention as a necessary nursing service. Hence, nursing need assessment, nursing data collection, and nursing process are required to prevent pressure ulcers.
In comparison with patients in general wards, patients admitted to intensive care units (ICUs) are at high-risk for pressure ulcers [8] as they have many risk factors resulting in immobilization, such as a mechanical ventilator, lowered level of consciousness, decreased sensation, malnutrition, edema, and fecal and urinary incontinence [9,10]. Thus, by identifying risk factors for pressure ulcers in ICUs and the high-risk groups, focused and effective nursing care prevents pressure ulcers, assures patients safety, and reduces the cost by decreasing the length of a hospital stay [11].
Pressure ulcer risk assessment scales have been developed and used to identify high-risk groups for pressure ulcers. A proper assessment scale focusing on specific patient groups, such as ICU patients, would be very important and would enable the provision of proper nursing care in timely manner. Although the Braden scale [12], most broadly used in clinical settings, has been developed for patients in general wards, previous studies have shown that the Braden scale tends to overestimate the risks of developing pressure ulcer and thus has resulted in increased costs for pressure ulcers prevention as well as unnecessary nursing workload [13,14]. Other assessment scales have also been developed, and the Cubbin and Jackson scale [15] is one that is specifically focused on ICU patients. It has been reported to show better ability to predict pressure ulcer development in this population than the Braden scale [8,16,17]. The Cubbin and Jackson scale includes ICU specific items, such as hemodynamics and respiration, whereas the Braden scale has items that can apply to any clinical settings. Because the Braden scale is widely used in hospitals, it is speculated that the Braden scale is more convenient to utilize than the Cubbin and Jackson scale [18] in terms of time and effort of nurses' assessment, and a hospital may want to have a universal tool for hospital-wide statistics.
When promoting a practical way of using the Cubbin and Jackson scale for ICU patients, it is important to investigate whether the data already existing in current Electronic Medical Records (EMRs) are reusable in an effective way, such that they can help nurses identify ICU patients at high-risk for pressure ulcers more accurately while reducing the time and efforts to apply a new pressure ulcer risk assessment scale. However, there has been no research about whether and how information from EMRs structurally matches with the items of the Cubbin and Jackson scale; therefore, more validation studies of the Cubbin and Jackson scale are needed to support its further use [14]. To address this issue, we first examined the predictive validity of the Cubbin and Jackson scale on pressure ulcer development in ICU patients, and then evaluated the reusability of EMR data for the Cubbin and Jackson scale.
Before evaluating the reusability of EMR data for applying the Cubbin and Jackson pressure ulcer risk assessment scale in ICU patients, a retrospective study was conducted to examine the predictive validity of pressure ulcer development risk scales in medical and surgical ICU patients comparing the Cubbin and Jackson scale and the Braden scale using nursing records extracted from EMR.
The subjects of this study were patients admitted to four ICUs (two medical and two surgical ICUs) at a university hospital in Seoul, Korea where EMR has been fully utilized since 2005. The selection criteria were patients aged 18 years or older who stayed in the ICU longer than 24 hours and did not have pressure ulcers indicated in nursing records when they were admitted to ICUs.
Among 2,710 patients who were admitted to ICUs for one year from May 2010 to April 2011, 1,614 were electronically selected based on the selection criteria. The total number of subjects who were finally included in the data analysis was 829 after excluding subjects whose nursing records had missing data on essential variables of the Cubbin and Jackson scale and the Braden scale. In case of multiple admissions to ICUs of one patient during the study period, only the admissions for the initial hospitalization and re-hospitalization were included due to concern about the influence of severity from the same hospitalization on pressure ulcer development.
The pressure ulcer risk assessment scales included in this study were the Cubbin and Jackson scale to evaluate the validity of its application to ICU patients and the Braden scale that is generally used across all wards in hospitals.
This scale was developed by Cubbin and Jackson in 1991 [13] for ICU patients, and consists of 10 items: age, weight, general skin condition, mental condition, mobility, hemodynamics, respiration, nutrition, incontinence, and hygiene. Each item has a 4-point scale; thus, the point total is 40. The lower the point total is, the higher the likelihood of pressure ulcer development is. To use EMR data to match the Cubbin and Jackson items, operational definitions were created as shown in Table 1. For example, for hemodynamic criteria, mean blood pressure, which most accurately reflects the blood flow of tissue, was used, and the lowest value on the day of ICU admission was extracted. Then 'stable' or 'unstable' was determined after literature review and discussion with ICU and trauma specialists.
The Braden scale consists of 6 items, including sensory perception, moisture, activity, mobility, nutrition, and friction/shearing. Friction/shearing is on a 3-point scale, and other 5 items are on a 4-point scale. The possible score range is from 6 to 23, and the lower the point total is, the higher the risk of pressure ulcer development [12]. The Braden scale is the instrument assessed by each shift at ICUs in the study site, and the values at admission to the ICU were used in this study.
Finally, a total of 24 items were extracted from EMRs to possibly match items of the Cubbin and Jackson and Braden scales, along with other variables including sex, hospital departments, ICU length of stay, use of restraint and ventilator, and diagnosis with diabetes mellitus (DM). In addition, pressure ulcer was determined when patients developed pressure ulcers during their ICU stay.
Upon the approval of the Institutional Review Board of College of Nursing, Yonsei University (IRB 2012-1007), all data fields were initially obtained from the EMR system with assistance from a nurse informatician, and then further review of the EMRs was performed for semi-structured or unstructured fields (e.g., nutrition, incontinence) that required researchers' inspection for text data or understanding of the context associated with other data fields. The scores of the two pressure ulcer risk assessment scales from all patients were obtained upon the admission. The Braden scale was extracted from the information already existing in the EMR, and the items of the Cubbin and Jackson scale were extracted from the EMR based on the operational definitions given in Table 1.
Descriptive statistics were used to describe the characteristics of the subjects and pressure ulcers. The scores of the pressure ulcer risk assessment scales were compared between the pressure ulcer development group and non-pressure ulcer group using a t-test. The predictive validity of the scales, such as sensitivity, specificity, positive predictive value, negative predictive value, and receiver operating characteristics (ROC) curve with area under the curve (AUC) were obtained. Data analysis was performed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA).
The EMR reusability was evaluated by applying the following criteria to assess data corresponding to each item of the EMR [19]: 1) Complete match with structured data: one-to-one match with a certain item of a structured input screen; 2) Complete match with nursing statement: no match with an item of a structured input screen but match with nursing statements; 3) Suboptimal match: no match with an item of a structured input screen but it is possible to logically extract information from more than two data items and/or standardized statements; and 4) Incomplete match: no match with data from either a structured screen or nursing statements that is difficult to presume any information when combining those.
The total number of subjects used in the final analysis was 829. Among them, 522 (63.0%) were men, and the average age of the subjects was 59.77 years (standard deviation [SD], 14.87 years). The average body mass index (BMI) and ICU length of stay were 23.14 kg/m2 (SD, 3.77 kg/m2) and 1.43 days (SD, 0.88 days), respectively. The incidence of pressure ulcers during ICU stay was 14.2% (n = 118) (Table 2).
As shown in Table 3, there was no significant difference of age and BMI between groups with pressure ulcer development and no development. The length of stay of the two groups showed a significant difference (χ2 = 193.22, p < 0.001); the incidence of pressure ulcers increased as the length of stay was prolonged. The number of patients who died upon discharge was statistically higher in the pressure ulcer development group than their counterparts (χ2 = 65.76, p < 0.001).
Subjects who had DM showed a higher incidence of pressure ulcer development (25.26% vs. 9.99%) with a statistical significance (χ2 = 10.69, p < 0.001). If subjects had edema at the time of admission, pressure ulcers developed more than those without (38.1% vs. 18.1%; χ2 = 24.39, p < 0.001). Similarly, subjects who had to use a ventilator (χ2 = 96.28, p <0.001) and restraints (χ2 = 82.51, p < 0.001) showed a significantly higher incidence of pressure ulcer development than their counter parts. Subjects who had hemodynamic status with less than or equal to 55 mmHg mean blood pressure were 29 (24.6%) in the pressure ulcer development group and 66 (9.3%) in the non-pressure ulcer group (χ2 = 32.89, p < 0.001).
The scores of the Cubbin and Jackson scale at the time of admission to the ICU are shown in Table 4. The total score of the Cubbin and Jackson scale was 22.98 ± 3.30 in the pressure ulcer development group and 26.49 ± 3.51 in the non-pressure ulcer group, which showed statistical significance (t = 10.605, p < 0.001). There was a significant difference between the two groups in 8 out of 10 items of the Cubbin and Jackson scale, including weight, mental condition, mobility, hemodynamics, respiration, nutrition, incontinence, and hygiene, where the group in which pressure ulcers developed scored worse than their counterparts. However, there was no significant difference in age and general skin condition.
The total Braden scale scores were 12.94 ± 2.38 in the pressure ulcer development group and 14.69 ± 2.01 in the non-pressure ulcer group (t = 7.554, p < 0.001). When comparing the scores per item by groups to examine whether or not pressure ulcers developed, there was a significantly higher score on five items out six, namely, sensory perception, moisture, mobility, nutrition, and friction/shearing (data not shown).
For the cut-off point to calculate the validity of each scale, the cut-off point suggested by the developer of each instrument was used. The sensitivity, specificity, positive predictive value, and negative predictive values were 72.0%, 68.8%, 27.7%, and 93.7% for the Cubbin and Jackson scale and 93.2%, 16.6%, 15.6%, and 93.7% for the Braden scale, with the cut-off points of 24 and 16, respectively.
The ROC curve and AUC of each scale were obtained to compare the predictive validity for the subjects' pressure ulcer development. The AUC showed 0.763 for Cubbin and Jackson scale, and 0.711 for Braden scale, which indicates that the Cubbin and Jackson scale performed slightly better to predict pressure ulcer development (Figure 1).
This study investigated the reusability of 10 items in order to examine the feasibility of EMR use for the Cubbin and Jackson scale. The reusability of EMR data was analyzed by applying criteria [19], such as complete match with structured data, complete match with nursing statement, suboptimal match, and incomplete match. We were able to extract data from 6 structured input screens on EMR, such as timeline worksheet, clinical medical records, nursing records, nutrition, medication, and the assessment form used in the ICU of the hospital. Four items out of 10 matched completely with structured data items, one item matched completely with structured statement, three items with a suboptimal match, and two items with an incomplete match (Table 5).
Looking into more details, age, mental condition, respiration, and incontinence showed complete matching with structured data, and skin condition showed complete matching with structured statement. The examples of suboptimal matches, in which matching was possible by combining more than two data items, were weight, hemodynamics, and nutrition. For weight, BMI on the clinical record and edema or no edema on the assessment form was used. For hemodynamics, both mean blood pressure on the clinical record and inotropic use on the medication screen were used. Nutritional treatment and total parenteral nutrition on the medication screen were used for nutrition. Activity and hygiene showed incomplete matching, which could not be obtained from the organized screen of EMR and data of standardized statements.
The purposes of this study were to examine the predictive validity of the Cubbin and Jackson scale for pressure ulcer development in ICU patients retrospectively and to assess the reusability of EMR data for the Cubbin and Jackson scale. Therefore, we first discuss the characteristics of pressure ulcers, risk factors of pressure ulcer development, and the predictive validity of the Cubbin and Jackson scale. Then, we discuss the reusability of EMR data.
The total number of subjects in this study was 829, and pressure ulcer incidence during ICU stay was 118 (14.2%). Although the incidence rates of pressure ulcers differ depending on the data-collection methods used or the characteristics of patients, it was lower in this study than in other studies. Pressure ulcers occur in 31.3% of neurologic, medical, and surgical ICU patients [17] and 28.6% of medical ICU patients [20] in Korea. In addition, it is reported that 34.4% [11] or 18.7% [18] of medical and surgical ICU patients developed pressure ulcers in overseas studies. As severity, surgery, and mechanical ventilator are known risk factors of pressure ulcers [21-23], pressure ulcers also tend to develop more frequently at immediate admission because of the high doses of inotropics infused and the difficulty of position change due to unstable hemodynamics and the performance of necessary procedures. The risk factors of pressure ulcer development that were related with general and clinical features identified in this study included ICU length of stay, patient's condition at the time of discharge, DM, edema, use of mechanical ventilator, restraint application, and mean blood pressure.
General edema and increased weight are associated with aggravation of skin condition [23]. In particular, the use of a mechanical ventilator causes edema due to positive pressure, which thus can lead to the development of pressure ulcers [24,25]. Also, using restraints often causes pressure ulcer development in critical care patients [26]. DM is reported as a risk factor of pressure ulcers [21], and it was also a significant risk factor in this study. Additionally, the incidence of pressure ulcers was higher in the group with lower mean blood pressure. Mean blood pressure lower than 60 to 70 mmHg was associated with impaired skin condition [13,23].
It is essential to study the predictive validity of a scale that can detect the risk of pressure ulcers to prevent lengthening of hospital stay and spending on unnecessary medical cost. Based on the data analysis in this study, the sensitivity, specificity, positive predictive value, and negative predictive value at the cut-off point of 24 were 72%, 68.8%, 27.7%, and 93.7% for the Cubbin and Jackson scale. For the Braden scale, they were 93.2%, 16.6%, 15.6%, and 93.7%, respectively, at the cut-off point of 16. In a previous study with a prospective study design, the sensitivity, specificity, positive predictive value, and negative predictive value of the Cubbin and Jackson scale were 89%, 61%, 51%, and 92% [17].
Given that the AUC calculated in this study was 0.711 in the Braden scale, and 0.763 in the Cubbin and Jackson scale, the value in the Cubbin and Jackson scale was slightly higher but lower than the validity from previous studies. This is probably because we used proxies for mobility and hygiene that were derived from a mobility item of the Braden scale without directly identifying skin conditions from either observation or nursing records. However, there have been several previous studies indicating that the ability of the Cubbin and Jackson scale to predict pressure ulcer development is more accurate than that of the Braden scale in ICU patients [8,16,17]. Thus, further studies are needed to verify the scale prospectively prior to development of an EMR data form. Also, re-evaluation and adjustment of cut-off points are needed to enhance the prediction ability of the scale.
When a scale with high sensitivity and positive prediction ability without considering specificity is used, nurses might miss patients who need preventive nursing care. Therefore, it is important to choose a scale with high sensitivity and negative prediction ability to provide care to patients with possible pressure ulcer development. If there are scales with similar sensitivity and negative prediction ability, a scale with fair specificity and positive prediction ability should be the choice. Therefore, the Cubbin and Jackson scale would be more appropriate than the Braden scale based on the study findings.
Another important objective of this study was to examine the reusability of nursing data in applying the pressure ulcer risk assessment scale to predict pressure ulcer development in critical care patients. In the extraction of 10 items in the Cubbin and Jackson scale, 8 items (i.e., age, weight, general skin condition, mental condition, hemodynamics, respiration, nutrition, and incontinence) were extracted using EMR data as they had either a complete match with structured data, a complete match with nursing statement, or a suboptimal match, whereas two items (mobility and hygiene) did not match with EMR data fields. When nurses are dissatisfied with the method of documentation, nurses often enter information into the nursing record with free text rather than choosing standardized statements. Free text has the advantage that it is relatively fast and expression is unrestrained, but it is difficult to extract data in a standardized and coded format for further reuse. Also, inappropriate data or errors can be minimized through further education for nurses about documenting appropriately or EMR structure modification [27].
In the era of Big Data, the reuse of patient documentation [28] and structured data format [29] has been greatly emphasized. The use of standardized statements is a significant consideration in using the data of electronic nursing records given that the documentation on nursing records is more unstructured documentation than structured documentation [19]. Also, if researchers study the structure of nursing information of EMR and develop the knowledge and capacity of data usage, structured documentation would support the broader use of nursing record data [30] and ultimately increase the efficiency of nursing services.
Although this study is limited as a retrospective study by using operational definitions for hemodynamics, mobility, incontinence, and hygiene, the reusability of EMR data to assess pressure ulcer risks by using the Cubbin and Jackson scale has been initially demonstrated. Nurses manually enter data to identify patients at high-risk of pressure ulcers development using pressure ulcer risk assessment scales on a regular basis. Therefore, it is more desirable to maximize the use of data already collected and stored through EMR and minimize the number of items nurses have to document. This helps to decrease the workload by facilitating pressure ulcer risk assessment by nurses and focuses on the timely and effective prevention of pressure ulcers for high-risk patients by adding the electronic nursing assessment of the Cubbin and Jackson scale to current EMR systems.
Figures and Tables
Figure 1
The receiver operating characteristics curve of Cubbin and Jackson scale and Braden scale. The area under the curve (AUC) showed 0.763 for Cubbin and Jackson scale, and 0.711 for Braden scale.
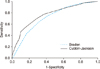
Table 4
Differences in item scores of Cubbin and Jackson scale by pressure ulcer development (n = 829)

Table 5
Matches of Electronic Medical Record data with Cubbin and Jackson scale

aOne-to-one match with a certain item of a structured input screen. bNo match with an item of a structured input screen but match with nursing statements. cNo match with an item of a structured input screen, but it is possible to logically extract information from more than two data items and/or standardized statements. dNo match with data from either a structured screen or nursing statements that is difficult to presume any information when combining those.
References
1. Nijs N, Toppets A, Defloor T, Bernaerts K, Milisen K, Van Den Berghe G. Incidence and risk factors for pressure ulcers in the intensive care unit. J Clin Nurs. 2009; 18(9):1258–1266.

2. Agency for Healthcare Research and Quality. Preventing pressure ulcers in hospitals: a toolkit for improving quality of care. Rockville (MD): Agency for Healthcare Research and Quality;2011. cited at 2013 Dec 18. Available from: http://www.ahrq.gov/professionals/systems/long-term-care/resources/pressure-ulcers/pressureulcertoolkit/index.html.
3. Bennett G, Dealey C, Posnett J. The cost of pressure ulcers in the UK. Age Ageing. 2004; 33(3):230–235.

4. Hughes RG. Patient safety and quality: an evidence-based handbook for nurses. Rockville (MD): Agency for Healthcare Research and Quality;2008.
5. Furukawa MF, Raghu TS, Shao BB. Electronic Medical Records, nurse staffing, and nurse-sensitive patient outcomes: evidence from the national database of nursing quality indicators. Med Care Res Rev. 2011; 68(3):311–331.

6. Bergquist-Beringer S, Gajewski B, Dunton N, Klaus S. The reliability of the National Database of Nursing Quality Indicators pressure ulcer indicator: a triangulation approach. J Nurs Care Qual. 2011; 26(4):292–301.

7. Korea Institute for Healthcare Accreditation. Survey standards for healthcare accreditation. Seoul: Ministry of Health & Welfare;2011.
8. Shahin ES, Dassen T, Halfens RJ. Pressure ulcer prevalence in intensive care patients: a cross-sectional study. J Eval Clin Pract. 2008; 14(4):563–568.

9. Theaker C. Pressure sore prevention in the critically ill: what you don't know, what you should know and why it's important. Intensive Crit Care Nurs. 2003; 19(3):163–168.

10. Manzano F, Navarro MJ, Roldan D, Moral MA, Leyva I, Guerrero C, et al. Pressure ulcer incidence and risk factors in ventilated intensive care patients. J Crit Care. 2010; 25(3):469–476.

11. Cremasco MF, Wenzel F, Zanei SS, Whitaker IY. Pressure ulcers in the intensive care unit: the relationship between nursing workload, illness severity and pressure ulcer risk. J Clin Nurs. 2013; 22(15-16):2183–2191.

12. Bergstrom N, Braden BJ, Laguzza A, Holman V. The Braden Scale for Predicting Pressure Sore Risk. Nurs Res. 1987; 36(4):205–210.

13. Cubbin B, Jackson C. Trial of a pressure area risk calculator for intensive therapy patients. Intensive Care Nurs. 1991; 7(1):40–44.

14. Sousa B. Translation, adaptation, and validation of the Sunderland Scale and the Cubbin & Jackson Revised Scale in Portuguese. Rev Bras Ter Intensiva. 2013; 25(2):106–114.

15. Boyle M, Green M. Pressure sores in intensive care: defining their incidence and associated factors and assessing the utility of two pressure sore risk assessment tools. Aust Crit Care. 2001; 14(1):24–30.

16. Jun S, Jeong I, Lee Y. Validity of pressure ulcer risk assessment scales; Cubbin and Jackson, Braden, and Douglas scale. Int J Nurs Stud. 2004; 41(2):199–204.

17. Cox J. Predictors of pressure ulcers in adult critical care patients. Am J Crit Care. 2011; 20(5):364–375.

18. Pancorbo-Hidalgo PL, Garcia-Fernandez FP, Lopez-Medina IM, Alvarez-Nieto C. Risk assessment scales for pressure ulcer prevention: a systematic review. J Adv Nurs. 2006; 54(1):94–110.

19. Cho IS, Yoon HY, Park SI, Lee HS. Availability of nursing data in an electronic nursing record system for a development of a risk assessment tool for pressure ulcers. J Korean Soc Med Inform. 2008; 14(2):161–168.

20. Kim HJ, Jeong IS. Optimal time interval for position change for ICU patients using foam mattress against pressure ulcer risk. J Korean Acad Nurs. 2012; 42(5):730–737.

21. Alderden J, Whitney JD, Taylor SM, Zaratkiewicz S. Risk profile characteristics associated with outcomes of hospital-acquired pressure ulcers: a retrospective review. Crit Care Nurse. 2011; 31(4):30–43.

22. Compton F, Hoffmann F, Hortig T, Strauss M, Frey J, Zidek W, et al. Pressure ulcer predictors in ICU patients: nursing skin assessment versus objective parameters. J Wound Care. 2008; 17(10):417–420. 422–424.

23. Curry K, Kutash M, Chambers T, Evans A, Holt M, Purcell S. A prospective, descriptive study of characteristics associated with skin failure in critically ill adults. Ostomy Wound Manage. 2012; 58(5):36–38. 40–43.
24. Brunk D. Are pressure ulcers really a 'Never Event'? Chest Physician. 2011; 6(3):6.
25. Schindler CA, Mikhailov TA, Kuhn EM, Christopher J, Conway P, Ridling D, et al. Protecting fragile skin: nursing interventions to decrease development of pressure ulcers in pediatric intensive care. Am J Crit Care. 2011; 20(1):26–34.

27. Cho IS. Assessing the quality of structured data entry for the secondary use of Electronic Medical Records. J Korean Soc Med Inform. 2009; 15(4):423–431.

28. Takabayashi K, Doi S, Suzuki T. Japanese EMRs and IT in medicine: expansion, integration, and reuse of data. Healthc Inform Res. 2011; 17(3):178–183.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download