Abstract
Objectives
Methods
Results
Figures and Tables
Figure 1

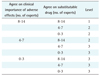
Table 2






Oxybutynin in class 15 was classified anticholinergic in Fialova et al. [16]. However, it is classified as muscle relaxants and antiasmonic according to Beers criteria [6].
CNS: central nervous system, NSAIDs: non steroidal anti-inflammatory drugs, GI: gastrointestinal, ASA: acetylsalicylic acid, TCA: tricyclic antidepressant, SSRI: selective serotonin reuptake inhibitor, BZD: benzodiazepines, SIADM: syndrome of inappropriate antidiuretic hormone secretion.
aReferences for substitute drugs: a1McLeod [13], a2MICROMEDEX (www.micromedex.com). bIndicates the number of respondents who answered 3 or more points/number of respondents for the agreement on the clinical importance of side effect and alternative drugs. cThe average scores among those who answered the clinical importance of side effect as 4-likert scale. dKorean classification: group 1 drugs need to be avoided, group 2 drugs need to be monitored, group 3 drugs without need of monitoring due to minimal danger to the elderly. eZhan's classification - aa: always avoid, ra: rarely appropriate; si: some indications. fBeers criteria - √H: high severity, √L: low severity.
Table 3







Indicates the number of respondents who answered 3 or more points/number of respondents for the agreement on the clinical importance of side effect and alternative drugs. The average score among those who answered the clinical importance of side effect as 4-Likert scale.
NSAIDs: non steroidal anti-inflammatory drugs, SSRI: selective serotonin reuptake inhibitor, NDDM: non-insulin-dependent diabetes mellitus, INR: international normalized ratio, ASA: acetylsalicylic acid, ACE: angiotensin-converting enzyme, BPH: benign prostatic hyperplasia, SIADH: syndrome of inappropriate antidiuretic hormone secretion, TCA: tricyclic antidepressant, CNS: central nervous system, MAOI: monoamine oxidase inhibitor, COPD: chronic obstructive pulmonary disease.
aReferences for substitute drugs: a1McLeod [13], a2MICROMEDEX (www.micromedex.com). bKorean classification: group 1 drugs need to be avoided, group 2 drugs need to be monitored, group 3 drugs without need of monitoring due to minimal danger to the elderly. cBeers criteria - √H: high severity, √L: low severity. dAntispasmodics: alverine citrate, caroverine HCl, drotaverine HCl, fenoverine, flupropione, octylonium bromide, papaverine HCl, phloroglucinol, pipoxolan HCl, pramiverine HCl, rociverine citrate, timepidium bromide, tiquizium bromide, tiropramide HCl, trimebutine maleate, trimethylphloroglucinol. eCalcium channel blocker: amlodipine, barnidipine HCl, benidipine, cilnidipine, cinnarizine, diltiazem HCl, efonidipine, felodipine, flunarizine HCl, gallopamil HCl, isradipine, lacidipine, lercanidipine HCl, manidipine HCl, nicardipine HCl, nifedipine, nilvadipine, nimodipine, nisoldipine, nitrendipine, verapamil HCl. fAntidepressants: bupropion, dried kava kava root extract, hyperici dried ext., hyperici ext., hypericin, hypericum tinc-D2, minaprin HCl, buspirone, trazodone, milnacipran HCl, nefazodone, venlafaxin HCl, Citalopram, fluoxetine HCl, fluvoxamine maleate, paroxetine HCl, sertraline HCl, amitriptyline HCl, clomipramine HCl, Clozapine, dothiepin HCl, Doxepine HCl, imipramine HCl, mianserine HCl, mirtazapine, nortryptiline HCl, quinupramine, setiptilin maleate, amineptine, amoxapine, maprotiline HCl, escitalopram. gThiazide diuretic: chlortalidone, hydrochlorothiazide, irbesartan, losartan potassium, mefruside, moexipril HCl, metolazone, nadolol, polythiazide, spironolactone, bendroflumethiazide, inositol hexanicotinate, indapamide, tripamide. hAnticholinergics: atropine sulfate, belladonna ext., biperiden HCl, chlorbenzoxamine 2HCl, lidinium bromide, dicyclomine HCl, difemerine HCl, emepronium bromide, glycopyrrolate, hyoscine butylbromide, hyoscyamine sulfate, isopropamide iodide, mebeverine HCl, oxapium odide, oxybutynin chloride, pinaverium bromide, pirenzepine HCl, procyclidine HCl, propiverine HCl, scopolia ext., tiemonium iodide, tiemonium methylsulfate, tolterodine tartrate, trihexyphenidyl HCl, trospium chloride, valethamate bromide. iMuscle relaxants: afloqualone, atracurium besylate, baclofen, carisoprodol, chlorphenesin arbamate, chlorzoxazone, cisatracurium besylatel (as cisatracurium, clostiridium botulinum A oxin, cyclobenzaprine HCl, dantrolene sodium, eperisone HCl, galamine triethiodide, methocarbamol, orphenadrine citrate, pancuronium bromide, pipecuronium bromide, pridinol esylate, rocuronium bromide, succinylchoine chloride, suxamethonim chloride, thiocolchicoside, tizanidine HCl, tolperisone HCl, vecuronium bromide, metocurine iodide. jNSAIDs: aceclofenac, acemetacin, alminoprofen, aloxiporin, amfenac sodium, benzydamine HCl, innoxicam, clonixin lysinate, diclofenac sodium, difenpiramide, emorfazone, enfenamic acid, etodolac, etofenamate, fenbufen, fenoprofen calcium, floctafenine, flufenamic acid, flurbiprofen, glucamethacin, ibuprofen, indomethacin, ketoprofen, ketorolac tromethamine, lonazolac calcium, lornoxicam, loxoprofen sodium, meclofenamate sodium, mefenamic acid, meloxicam, mepirizole, morniflumate, nabumetone, naproxen, niflumic acid, nimesulide, oxaprozin, piroxicam, pranoprofen, proglumetacin maleate, proquazone, pyrazinobutazone, sulindac, sulpyrin, tenoxicam, tiaprofenic cid, tolfenamic acid, trometamol tiaprofenate, zaltoprofen, bumadizone, talniflumate, (celecoxib, rofecoxib), aspirin, balsalazide disodium dihydrate, benorylate, bismuth ubsalicylate, choline magnesium trisalicylate, diflunisal, imidazole salicylate, magnesium salicylate, esalazine, salsalate, sodium salicylate, sulfasalazine, theobromine sodium salicylate, salicylamide. kSteroids: betamethasone valerate, deflazacort, dexamethasone, dexamethasone palmitate, examethasone sodium phosphate, fludrocortisone acetate, halopredone, hydrocortisone, hydrocortisone sodium succinate, methylprednisolone acetate, methylprednisolone sodium succinate, prednisolone, prednisolone acetate, prednisolone sodium succinate, prednisolone stearylglycolate, triamcinolone, triamcinolone acetonide. lβ-adrenergic blocking agent: acebutolol HCl, amosulalol HCl, arotinolol HCl, atenolol, betaxolol HCl, bevantol, bisoprolol, carteolol HCl, carvedilol, celiprolol HCl, cloranolol HCl, labetalol HCl, metoprolol succinate, nadolol, nipradilol, penbutolol sulfate, pindolol, propranolol HCl, sotalol HCl, acebutolol HCl, amosulalol HCl, arotinolol HCl, atenolol, betaxolol HCl, bevantol, bisoprolol, carteolol HCl, carvedilol, celiprolol HCl, cloranolol HCl, labetalol HCl, metoprolol succinate, nadolol, nipradilol, penbutolol sulfate, pindolol, propranolol HCl, sotalol HCl. mTricyclic antidepressant: amitriptyline HCl, clomipramine HCl, Clozapine, dothiepin HCl, Doxepine HCl, imipramine HCl, mianserine HCl, mirtazapine, nortryptiline HCl, quinupramine, setiptilin maleate, amineptine, maprotiline HCl, amitriptyline HCl, clomipramine HCl, Clozapine, dothiepin HCl, Doxepine HCl, imipramine HCl, mianserine HCl, mirtazapine, nortryptiline HCl, quinupramine, setiptilin maleate, amineptine, maprotiline HCl. nAntihistamines: acrivastine, astemizole, azatadine maleate, bepotastine besilate, brompheniramine aleate, buclizine 2HCl, carbinoxamine maleate, cetirizine HCl, chlorcinnazine 2HCl, chlorpheniramine maleate, clemastine fumarate, cyproheptadine HCl, dexbromopheniramine, dimenhydrinate, diphenylpyraline HCl, doxylamine succinate, ebastine, emedastine fumarate, epinastine HCl, fexofenadine, homochlorcyclizine HCl, hydroxyzine HCl, ketotifen fumarate, levocetirizine, loratadine, mequitazine, mizolastine, oxomemazine HCl, phenindamine tartrate, piprinhydrinate, promethazine HCl, terfenadine, trimeprazine tartrate, triprolidine HCl, diphenhydramine, azelastine, shiosulamime, oxatomide. oConventional antipsychotics: amisulpiride, melperone HCl, aripiprazole, bromperidol, chlorpromazine, chlorprothixene, droperidol, flupentixol HCl, haloperidol, levomepromazine maleate, loxapine, mesoridazine besylate, molindone HCl, nemonapride, olanzapine, perphenazine, pimozide, quetiapine fumarate, risperidone, sulpiride, thioridazine HCl, trifluoperazine HCl, ziprasidone hydrochloride monohydrate, zotepin, zuclopenthixol, thiothixene. pLong benzodiazepines: Chlordiazepoxide, clorazepate dipotassium, diazepam, ethyl loflazepate, flurazepam HCl, nordazepam. qDecongestant: ethylphenylephrine HCl, methylephedrine HCl, phenylpropanolamine HCl, pseudoephedrin HCl, phenyephrine. rBarbiturates: mytal sodium, entobarbital sodium, henobarbital, ecobarbital sodium, hiopental. sMAOI: amoxapine, moclobemide, toloxatone. tSSRI: citalopram, fluoxetine, fluvoxamine, paroxetine, sertraline. ushort-to intermediate-acting benzodiazepines: alprazolam, brotizolam, clobazam, clonazepam, clotiazepam, estazolam, etizolam, fludiazepam, flunitrazepam, flutoprazepam, lorazepam, mexazolam, midazolam, oxazepam, pinazepam, tofisopam, triazolam




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download