Abstract
Purpose
The aim of this study was to evaluate the clinicopathologic characteristics of papillary thyroid cancer with thyroiditis, and to determine the rate of its complications for it.
Methods
A retrospective review of 1,247 patients with papillary thyroid cancer who underwent primary thyroidectomy was performed. Among them, 316 patients had thyroiditis (group I) while 931 patients had no thyroiditis (group II), as reflected in the final pathologic reports. The two groups' clinicopathologic results and rate of complications were compared.
Results
Female gender, preoperative hypothyroidism, total thyroidectomy, no extrathyroid extension, no lymphovascular invasion, and no perineural invasion were associated with group I. More central lymph nodes were removed in group I than in group II, but there were fewer central lymph nodes with metastasis in group I than in group II. For the lateral lymph nodes, the two groups had the same numbers of removed nodes and nodes with metastatic tumor. Multivariate analysis revealed female predominance, more cases of preoperative hypothyroidism, more dissected lymph nodes, and fewer lymph nodes with metastasis in group I. Among the patients who underwent lobectomy, postoperative hypothyroidism occurred more in group I than in group II (P < 0.001). There was no difference in postoperative complications between the two groups.
Thyroiditis is frequently present in patients with papillary thyroid carcinoma [1-7]. The development of thyroiditis in such cases has made thyroidectomy more difficult [8]. Due to the inflammation of the thyroid gland, the gland becomes swollen, enlarged, and hard, and often adheres to the surrounding structures. The central lymph nodes around the thyroid gland also become enlarged due to reactive hyperplasia. Thus, extensive central-lymph-node dissection due to enlarged lymph nodes makes the preservation of the parathyroid glands difficult. Extensive dissection can also increase the likelihood of recurrent laryngeal nerve injury. As a result, postoperative hypoparathyroidism and vocal-cord palsy are more common in these cases [9]. Patients with thyroiditis can be euthyroid or can have abnormal thyroid function, such as hypothyroidism or hyperthyroidism. Of these occurrences, hypothyroidism is the most commonly occurring. There is no standard for the extent of operation in patients with papillary thyroid cancer with thyroiditis, although these patients may have abnormal thyroid function before and after thyroid surgery. Many patients with thyroiditis develop clinical symptoms such as compression and neck pain as well as hoarseness as the thyroiditis worsens [9]. Thyroid lobectomy may be recommended for micropapillary thyroid carcinoma with thyroiditis regardless of the severity of the thyroiditis [10]. After lobectomy, however, some patients still complain of neck pain. The aim of this study was to evaluate the clinicopathologic characteristics and short-term postoperative functional outcomes of papillary thyroid cancer with thyroiditis, and to determine the rate of its complications, the incidence of central- and lateral-lymph-node metastasis.
The surgical department of the present hospital treated 1,247 patients who underwent thyroidectomy and central-lymph-node dissection with or without lateral-lymph-node dissection for papillary thyroid carcinoma within the period from March 2007 to February 2012. None of the patients had a history of previous thyroidectomy. A retrospective investigation of the clinical and pathological elements was performed on all the patients. The diagnosis of papillary thyroid cancer and thyroiditis were confirmed by reviewing the pathology reports. Among the patients, 316 (25.3%) had Hashimoto's thyroiditis, lymphocytic thyroiditis, or chronic thyroiditis (group I), while 931 had no thyroiditis (group II), as reflected in the final pathologic reports. Ultrasonography was performed on all the patients before surgery. The preoperative thyroid function was confirmed from each patient's medical history. The clinicopathologic characteristics, including coexistent thyroiditis, the patient's age and gender, tumor size, preoperative thyroid function, extent of operation, multiplicity of the disease, extrathyroid extension, lymphovascular invasion, presence of perineural invasion, number of dissected lymph nodes, and number of central and lateral lymph nodes with metastasis were investigated. Preoperative and postoperative hypothyroidism were defined as a history of preoperative T4 replacement or subclinical hypothyroidism (TSH, >5.5 µU/mL; normal range, 0.35 to 5.50 µU/mL). In the lobectomy patients, TSH suppression was not performed on the lobectomy patients. Postoperative hypothyroidism was determined in the lobectomy patients two to three months after lobectomy. Preoperative hyperthyroidism was defined as a history of taking antithyroid medication or subclinical hyperthyroidism (TSH, <0.5 µU/mL). The rates of complication, bleeding, hypocalcemia, hoarseness, and chylous fistula were reviewed. The patients with hypocalcemic symptoms along with a total calcium level of less than 7.8 mg/dL (normal range, 7.8 to 10.0 mg/dL) or an ionized calcium level of less than 0.96 mM/L (normal range, 0.96 to 1.40 mM/L) were considered as having hypocalcemia. The patients who continued to require calcium carbonate and oral 1,25-dihydroxycholecaldiferol more than six months after the operation were considered as having permanent hypocalcemia.
Statistical analyses were performed using the IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). Chi-square test, t-test, Fisher exact test, and logistic-regression analyses were used for the analysis of the variables related to thyroiditis. A P-value of less than 0.05 was regarded as a statistically significant result.
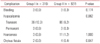
Among the total of 1,247 patients, 316 (25.3%) had Hashimoto's thyroiditis, lymphocytic thyroiditis, or chronic thyroiditis (group I), while 931 had no thyroiditis (group II), as reflected in the final pathologic reports. The preoperative antimicrosomal antibodies were 198.69 ± 313.04 and 27.58 ± 105.53 in groups I and II, respectively (P < 0.001). Female gender, preoperative hypothyroidism, total thyroidectomy, no extrathyroid extension, no lymphovascular invasion, and no perineural invasion were associated with group I (Table 1). The overall frequencies of central-lymph-node metastasis were 36.5% and 46.1% in groups I and II, respectively (P = 0.003). More central lymph nodes were removed in group I than in group II, but there were fewer central lymph nodes with metastasis in group I than in group II. The overall frequencies of lateral-lymph-node metastasis were 5.7% and 6.5% in groups I and II, respectively (P = 0.635). For the lateral lymph nodes, the two groups had the same numbers of removed nodes and nodes with metastatic tumor. No multicolinearity was found when checked using the variation inflation factor (1.015 to 1.642). Therefore, the data were appropriate for logistic-regression analysis. Multivariate analyses were performed to determine if there was a relationship between thyroiditis and the independent variables, with P < 0.1. The results indicated that female gender and preoperative hypothyroidism were more dominant in group I. Moreover, there were more central lymph nodes removed in group I. The number of lymph nodes with metastasis, however, was 1.179 (1/0.848) times higher in group II. The result of Hosmer-Lemeshow's goodness-of-fit test appears significant, with 0.777 probability. The estimated statistical model seems appropriate (Table 2).
Among the patients who underwent lobectomy, postoperative hypothyroidism occurred in 10 (52.6%) and 15 cases (14.2%) in groups I and II (P < 0.001), respectively.
Only the patients in group II (0.3%) had distant metastasis at the time of diagnosis. The recurrence rates were 0.3% (1 patient) and 0.6% (6 patients) in groups I and II, respectively. There was no significant difference between the two groups (P = 0.686). Neither was there a significant difference in the rate of complications between the two groups (Table 3).
The association between Hashimoto's thyroiditis and papillary thyroid cancer was first cited by Dailey et al. [1] in 1955. Since then, several studies have reported the association of thyroiditis with papillary thyroid cancer [4,5,7,11]. A controversy still exists, however, over the relationship between these two diseases. The possible mechanism between thyroiditis and papillary thyroid cancer is RET/PTC1 and RET/PTC3 mutation, PI3K/Akt expression, or immunoregulation defect and greater susceptibility to the development of a thyroid neoplasm [12-14].
The rate of thyroiditis in papillary thyroid cancer in this study was 25.3%, similar to other reports. Several studies have reported higher rates of younger patients and the female gender having papillary thyroid cancer with thyroiditis In this study, the papillary-thyroid-cancer patients with thyroiditis showed greater female predominance in the univariate and multivariate analysis, but no association was found with younger patients.
It was not clear if the presence of thyroiditis altered the biologic effect of papillary thyroid cancer. In this study, the presence of thyroiditis seemed to lessen the invasive potential of papillary thyroid cancer. There was less extrathyroid extension and less lymphovascular and perineural invasion in papillary thyroid cancer with thyroiditis. The presence of thyroiditis with papillary thyroid cancer was associated with less lymph node metastasis upon presentation. Several articles have reported that papillary thyroid cancer with thyroiditis is associated with a lower tumor stage and better prognosis [4,10]. A controversy still exists, however, over the prognosis of patients with papillary thyroid cancer with thyroiditis. Singh et al. [4] reported that the patients with papillary thyroid cancer with Hashimoto's thyroiditis in their study had good overall survival, based on the meta-analysis results. In that study, however, there was no change in the disease-free survival among the papillary-thyroid-cancer patients with coexisting Hashimoto thyroiditis. To predict the prognosis, several classifications have been developed for prognostication [15-18]. In this study, prognostic factors such as the extent of the tumor and lymph node metastasis were associated with the patients without thyroiditis (group II). The presence of distant metastasis was also found only in group II. The lung was the only site of distant metastasis. The patient's age and tumor size were not significantly different between the two groups. These findings show that patients with papillary thyroid cancer with thyroiditis are more likely to have better prognosis, although the recurrence rate is not different. The result of the study is limited due to the short follow-up period, which was not sufficient to reliably predict the patient's prognosis.
Several studies reported that the treatment of papillary thyroid cancer is not influenced by the presence of thyroiditis [4,9]. The extent of operation ranged from lobectomy to total thyroidectomy. In this study, total thyroidectomy was performed more often in the cases with thyroiditis, regardless of the preoperative thyroid function. As many patients with thyroiditis have other symptoms, such as compression and neck pain, these patients prefer to have total thyroidectomy [9]. There is no consensus about the effectiveness of TSH suppression for decreasing the risk of recurrence after lobectomy [10]. In this study, all the patients who underwent lobectomy did not take levothyroxine after the procedure. Among the patients who underwent lobectomy, more than half (52.6%) developed hypothyroidism and had to take T4 to control their hormone levels. In particular, thyroid lobectomy is a sufficient treatment for papillary thyroid microcarcinoma [10]. After lobectomy, however, many patients in this study developed hypothyroidism and eventually took medication. Additionally, Hashimoto thyroiditis is associated with an increased risk of developing papillary thyroid cancer [4,11,19]. Therefore, there is no reason to leave the other side of the thyroid gland. Total thyroidectomy is also recommended for patients with severe thyroiditis with diffuse enlargement and severe symptoms such as compression or neck pain. Although thyroiditis is confirmed from the results of the postoperative biopsy, there is no need for completion thyroidectomy because such procedure is required when the patient needs radioactive iodine therapy. Among the patients with lobectomy in this study, however, one patient wanted completion thyroidectomy due to severe neck pain. The inflammation and associated fibrosis in thyroiditis result in thyroid gland enlargement and adhesions to the surrounding muscles. This makes dissection more difficult, and complications can occur unexpectedly. McManus et al. [9] reported that 18% of the patients with thyroiditis in their study had transient complications, while 3% had permanent complications. Other studies have reported, however, that the rate of complications was not higher in the patients with Hashimoto's thyroiditis [4,20]. In this study, the complications were not different in the patients with thyroiditis.
In conclusion, according to the American Thyroid Association guideline [10], thyroid lobectomy for papillary thyroid microcarcinoma may be a sufficient treatment. As such, lobectomy is currently increasingly being performed. The surgeon, however, must consider the postoperative thyroid function, the patient's symptoms, and the potential recurrence in the remnant thyroid gland. It is suggested in this study that the presence of thyroiditis is associated with less central-lymph-node metastasis. Therefore, thyroiditis with papillary thyroid cancer has good prognosis. Regardless of the preoperative thyroid function, however, many patients develop hypothyroidism after lobectomy, and take levothyroxine. Additionally, remnant thyroid with thyroiditis can be associated with an increased risk of developing cancer, but as the study period was too short, there was no patient in this study who was reported to have developed cancer in the remnant thyroid gland. Total thyroidectomy should be carefully considered for patients with suspected high risk of postoperative hypothyroidism for patients who have thyroiditis with papillary thyroid cancer, and surgery can be performed with a low risk of complications.
Figures and Tables
References
1. Dailey ME, Lindsay S, Skahen R. Relation of thyroid neoplasms to Hashimoto disease of the thyroid gland. AMA Arch Surg. 1955. 70:291–297.
2. Chesky VE, Hellwig CA, Welch JW. Cancer of the thyroid asociated with Hashimoto's disease: an analysis of forty-eight cases. Am Surg. 1962. 28:678–685.
3. Ott RA, Calandra DB, McCall A, Shah KH, Lawrence AM, Paloyan E. The incidence of thyroid carcinoma in patients with Hashimoto's thyroiditis and solitary cold nodules. Surgery. 1985. 98:1202–1206.
4. Singh B, Shaha AR, Trivedi H, Carew JF, Poluri A, Shah JP. Coexistent Hashimoto's thyroiditis with papillary thyroid carcinoma: impact on presentation, management, and outcome. Surgery. 1999. 126:1070–1076.
5. Kebebew E, Treseler PA, Ituarte PH, Clark OH. Coexisting chronic lymphocytic thyroiditis and papillary thyroid cancer revisited. World J Surg. 2001. 25:632–637.
6. Cipolla C, Sandonato L, Graceffa G, Fricano S, Torcivia A, Vieni S, et al. Hashimoto thyroiditis coexistent with papillary thyroid carcinoma. Am Surg. 2005. 71:874–878.
7. Tamimi DM. The association between chronic lymphocytic thyroiditis and thyroid tumors. Int J Surg Pathol. 2002. 10:141–146.
8. Shih ML, Lee JA, Hsieh CB, Yu JC, Liu HD, Kebebew E, et al. Thyroidectomy for Hashimoto's thyroiditis: complications and associated cancers. Thyroid. 2008. 18:729–734.
9. McManus C, Luo J, Sippel R, Chen H. Should patients with symptomatic Hashimoto's thyroiditis pursue surgery? J Surg Res. 2011. 170:52–55.
10. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.
11. Repplinger D, Bargren A, Zhang YW, Adler JT, Haymart M, Chen H. Is Hashimoto's thyroiditis a risk factor for papillary thyroid cancer? J Surg Res. 2008. 150:49–52.
12. Wirtschafter A, Schmidt R, Rosen D, Kundu N, Santoro M, Fusco A, et al. Expression of the RET/PTC fusion gene as a marker for papillary carcinoma in Hashimoto's thyroiditis. Laryngoscope. 1997. 107:95–100.
13. Larson SD, Jackson LN, Riall TS, Uchida T, Thomas RP, Qiu S, et al. Increased incidence of well-differentiated thyroid cancer associated with Hashimoto thyroiditis and the role of the PI3k/Akt pathway. J Am Coll Surg. 2007. 204:764–773.
14. McLeod MK, East ME, Burney RE, Harness JK, Thompson NW. Hashimoto's thyroiditis revisited: the association with thyroid cancer remains obscure. World J Surg. 1988. 12:509–516.
15. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 2010. 7th ed. New York: Springer.
16. Cady B, Rossi R. An expanded view of risk-group definition in differentiated thyroid carcinoma. Surgery. 1988. 104:947–953.
17. Hay ID, Grant CS, Taylor WF, McConahey WM. Ipsilateral lobectomy versus bilateral lobar resection in papillary thyroid carcinoma: a retrospective analysis of surgical outcome using a novel prognostic scoring system. Surgery. 1987. 102:1088–1095.
18. DeGroot LJ, Kaplan EL, McCormick M, Straus FH. Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metab. 1990. 71:414–424.
19. Holm LE, Blomgren H, Lowhagen T. Cancer risks in patients with chronic lymphocytic thyroiditis. N Engl J Med. 1985. 312:601–604.
20. American Thyroid Association Surgery Working Group. American Association of Endocrine Surgeons. American Academy of Otolaryngology-Head and Neck Surgery. American Head and Neck Society. Carty SE, Cooper DS, et al. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid. 2009. 19:1153–1158.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download