Abstract
We report our case of laparoscopy-assisted distal gastrectomy with D1 + β lymph node dissection for a patient with early gastric cancer and laparoscopic cholecystectomy for gallstone with situs inversus totalis. A superficial elevated lesion was found on the lesser curvature of the antrum. The preoperative diagnosis was cStage IA (cT1, cN0, cH0, cP0, cM0). A 1 cm-sized gallstone was found in the fundus through upper abdominal ultrasound. A laparoscopy-assisted distal gastrectomy with standard D2 lymph node dissection for early gastric cancer and laparoscopic cholecystectomy was successfully performed by not shifting the monitor to the left and right and not changing operator's position without additional blood loss and time. The number of retrieved lymph nodes was 36. We have not found any abnormal course of blood vessels except for the right/left inversion. Billroth I reconstruction was performed through end-to-side anastomosis. Based on a histopathological examination, a 1.5 × 1.5 cm, submucosal (sm3), moderately differentiated adenocarcinoma (pT1, pN0, sH0, sP0, sM0, stage IA) was diagnosed. The postoperative course was favorable and the patient was discharged on postoperative day 7.
Situs inversus totalis (SIT) is a relatively rare condition found in 1 per 10,000 to 50,000 persons [1]. SIT is an autosomal recessive congenital defect in which the position of abdominal and/or thoracic organs is a "mirror image" of the normal one, in the sagittal plane. The surgical procedure for a patient with SIT was recently reported. Only 3 cases of laparoscopy-assisted distal gastrectomy (LADG) for gastric cancer combined with situs inversus have previously been reported [2-4], but 1 case [2] did not describe the extent of the lymphadenectomy and the other case [3] had D1 + β performed. Recently, a third case [4] has been reported in Korea. We report our experience in performing a LADG including a D1 + β lymph node dissection for a patient with early gastric cancer and laparoscopic cholecystectomy for gallstone with SIT in ordinary surgeon's position.
A 60-year-old man visited our clinic for operation of gastric cancer incidentally detected by the Nation Health Welfare program. SIT was diagnosed via chest radiography and abdominal computed tomography (CT). Upper endoscopy identified a superficial elevated lesion on the lesser curvature of the antrum (Fig. 1), and well-differentiated adenocarcinoma was diagnosed based on tissue biopsy. No other physical abnormalities were noted. Routine laboratory tests yielded normal results. Chest radiography showed dextrocardia from the posteroanterior view (Fig. 2). Abdominal CT showed that all organs inside the abdomen were inversely positioned (Fig. 3) without enlarged lymph node, distant metastasis and abnormal co urse of vascularity. Abdominal ultrasonography revealed a 1 cm-sized gallstone in the fundus of the gall bladder (Fig. 4).
A LADG and D1+β dissection and laparoscopic cholecystectomy were performed. The surgeon stood on the right side of the patient (usual side of surgery in our hospital). We did not change the operator's position in our case to prevent confusion of right and left hand roles. A 10-mm camera port was created 2 cm below the umbilicus by open technique, and pneumoperitoneum was induced by using pressure of up to 12 mmHg carbon dioxide. 4 trocars were inserted in the left and right subcostal area and lateral abdominal region for operator and assistor (Fig. 5).
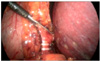
Laparoscopic view showed inversus of intraabdominal organ including stomach and spleen (Fig. 6). The gastrocolic ligament was along the border of the transverse colon using ultrasonic shears (Harmonic Ace, Ethicon Endo-Surgery Inc., Cincinnati, OH, USA). The position of the spleen was confirmed and the left gastroepiploic vessels located on the right side were ligated. In the pyloric region, the location of the pancreas was confirmed, and the area between this and the mesocolon was cut using ultrasonic shears to expose and ligate the right gastroepiploic vein located on the left side. The right gastroepiploic artery located on the left side bifurcating from the gastroduodenal artery was then confirmed and ligated (Fig. 7). Next, the lesser omentum was dissected, and the right gastric artery located on the left side bifurcating the proper hepatic artery was confirmed and ligated. The lymph node above the pancreas was dissected, and the coronary vein and left gastric artery located on the right side were ligated (Fig. 8). The perigastric lymph nodes were dissected along the lesser curvature up to the esophagogastric junction. Additional laparoscopic cholecystectomy was performed via antegrade method (Fig. 9). A 5-cm incision was made by right subcostal transverse incision. Through this minilaparotomy, the distal stomach was pulled out of the peritoneal cavity, and the distal two-thirds of the stomach was resected using a linear stapler. For Billroth I anastomosis, the duodenum was opened and the anvil of a circular stapler was inserted. The body of the circular stapler was introduced into the remnant stomach. Billroth I reconstruction was performed through end-to-side anastomosis (Fig. 10). After performing a stapling gastroduodenostomy, the opening in the remnant stomach was closed by an additional linear stapler. A closed suction drain was placed through the left upper trocar wound.
The operating time was 200 minutes and blood loss was 70 mL. No clear signs of abnormal bleeding were evident. The number of retrieved lymph nodes was 36. Based on a histopathological examination, a 1.5 × 1.5 cm, submucosal (sm3), moderately differentiated adenocarcinoma (pT1, pN0, sH0, sP0, sM0, stage IA) was diagnosed (Fig. 11). The postoperative course was favorable, and the patient was able to resume drinking water on postoperative day (POD) 3 and eating on POD 4. Thereafter, he was discharged on POD 7.
SIT is a relatively rare anomaly that occurs at an incidence of 1 in 10,000 to 50,000 of the population [1]. Recently, in patients with SIT, laparoscopic surgery has been performed, including a laparoscopic cholecystectomy, laparoscopic exploration of common bile duct, laparoscopic sigmoidectomy, laparoscopic sleeve gastrectomy [3] and LADG [2-4]. In addition, there was a report of a simultaneous operation of LADG and laparoscopic cholecystectomy [5].
Only 3 cases of LADG for gastric cancer combined with situs inversus have previously been reported. In Japan, 2 reports mentioned LADG for gastric cancer. However, 1 case [2] did not describe the extent of the lymphadenectomy and another case [3] D1 + β was performed by shifting the monitor to the right from the left. In other words, the surgeon stood on the left side of the patient (opposite the usual side for surgery). Recently, a third case has been added to this list in Korea [4].
In the present surgery, the surgeon and assistant stood on the ordinary sides of surgery. However, 2 previously reported cases were performed by standing opposite the standard side of surgery. Previous authors mentioned that they did not find any difficulties due to performing the operation in a mirror image point of view. In addition, they declared that the mirror image positions were the key to performing the operation smoothly. In our case, operative procedures were not different to ordinary procedures, basically. However, the "mirror-image" confused the operator's hands. Camera assistance did not provide difficulties because of no position change. However, the first assistant had difficulties in orientation of entire anatomy. Thus, we prepared a preliminary discussion for surgeon and first assistant. With team discussion, we believe that our operation was performed successfully. We experienced the ease of ordinary position, especially for righthanded surgeons. This point may be controversial among surgeons. Simultaneously, that may be a matter of surgeon preference.
SIT could be accompanied by cardiopulmonary malformation, including familial long QT syndrome [6], total esophageal duplication [7], agnathia [8], and several urologic anomalies [9]. And there is the likelihood of postoperative complications. As such, meticulous preoperative evaluation is mandatory. We identified the vascularity of the present patient through abdominal CT scanning and confirmed no evidence of abnormal vascular malformation. To prevent surgery-related complications such as intraoperative bleeding or pancreatic injury, confidence in vascular anatomy and procedural carefulness are mandatory. Therefore, we believe that our operation could be performed with sufficient retrieved lymph node and without additional blood loss and time.
There was a report of a case of atypical cholinesterase in SIT patients [10]. And, that patient had an anesthetic complication during appendectomy. Although this case is very rare, surgeons and anesthesiologists must be aware of this condition during operation. In addition, meticulous postoperative management is mandatory. Close monitoring of cardiopulmonary function for several days postoperative is recommended.
In summary, we experienced a case of gastric cancer and gallstone associated with SIT treated successfully by LADG and laparoscopic cholecystectomy.
Figures and Tables
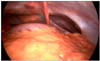
Fig. 1
Upper esophagogastroduodenoscopy showed slightly elevated lesion with central slightly depressed lesion in the lesser curvature of midantrum. Tissue biopsy showed well-differentiated tubular adenocarcinoma.
Fig. 3
Abdominal computed tomography showed that all intraabdominal organs were positioned inversely in a mirror image way.

Fig. 4
Abdominal ultrasonography showed single dependent echogenic foci with posterior acoustic shadowing consistent with gallstone.
Fig. 5
The sites of trocar placement. A trocar for camera was inserted into the subumbilical area by open technique.

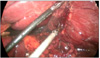
Fig. 7
Right gastroepiploic artery located on the left side was divided with double clips, allowing a dissection of station 6 lymph node.
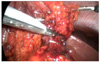
Fig. 8
Left gastric artery located on the right side was divided with double clips, allowing a dissection of station 9 lymph node.
References
1. Haruki T, Maeta Y, Nakamura S, Sawata T, Shimizu T, Kishi K, et al. Advanced cancer with situs inversus totalis associated with KIF3 complex deficiency: report of two cases. Surg Today. 2010. 40:162–166.
2. Yamaguchi S, Orita H, Yamaoka T, Mii S, Sakata H, Hashizume M. Laparoscope-assisted distal gastrectomy for early gastric cancer in a 76-year-old man with situs inversus totalis. Surg Endosc. 2003. 17:352–353.
3. Futawatari N, Kikuchi S, Moriya H, Katada N, Sakuramoto S, Watanabe M. Laparoscopy-assisted distal gastrectomy for early gastric cancer with complete situs inversus: report of a case. Surg Today. 2010. 40:64–67.
4. Kang BH, Lee SL, Hur H, Kim JY, Cho YK, Han SU. Laparoscopy assisted subtotal gastrectomy in gastric cancer patient with situs inversus in Korea. J Korean Surg Soc. 2010. 79:513–517.
5. Hiratsuka T, Ohta M, Sonoda K, Yamamura S, Nishizaki T, Matsusaka T, et al. Simultaneous operation of laparoscopy-assisted distal gastrectomy with laparoscopic cholecystectomy. Hepatogastroenterology. 2007. 54:1645–1647.
6. Corcos AP, Tzivoni D, Medina A. Long QT syndrome and complete situs inversus. Preliminary report of a family. Cardiology. 1989. 76:228–233.
7. Grewal HP, Leverment JN. Total oesophageal duplication associated with dextrocardia and situs inversus. Thorax. 1989. 44:1049–1050.
8. Stoler JM, Holmes LB. A case of agnathia, situs inversus, and a normal central nervous system. Teratology. 1992. 46:213–216.
9. Bertini JE Jr, Boileau MA. Renal cell carcinoma in a patient with situs inversus totalis. J Surg Oncol. 1987. 34:29–31.
10. Nayak R, Meck J, Hannallah M. Atypical cholinesterase in a patient with situs inversus totalis. Anesthesiology. 1995. 83:881.




 Citation
Citation Print
Print





 XML Download
XML Download