INTRODUCTION
Most cases of gallbladder perforation present as a complication of acute cholecystitis with or without cholelithiasis, and its incidence has been reported to range from 2% to 11% in acute cholecystitis.(1,2) Without these causes, generally, gallbladder perforation is caused by iatrogenic or traumatic causes but there are rare cases of idiopathic gallbladder perforation without a causative factor.(3) Accidental gallbladder perforation during a laparoscopic cholecystectomy is the most common cause of iatrogenic gallbladder perforation, which has been reported in up to 32% of laparoscopic cholecystectomies.(4,5) With the exception of these intraoperative accidents, iatrogenic gallbladder perforation is quite rare, and several cases have been reported previously as a complication of a percutaneous liver biopsy, percutaneous kidney biopsy, percutaneous transhepatic cholangiography or gastric endoscopic mucosal resection (EMR) etc.(6-9)
We present a very rare case of iatrogenic gallbladder perforation during gastric EMR without evidence of a perforation of the stomach. The gallbladder perforation was missed preoperatively and a definite diagnosis was made during surgery.
CASE REPORT
A 55-year-old man was admitted to our hospital for gastric EMR of gastric polyps found incidentally. He had no history of medical or surgical illnesses. The physical examination was unremarkable and his vital signs were blood pressure, pulse rate and body temperature of 130/80 mmHg, 72 beats/min and 36.5℃, respectively. He had undergone a medical checkup one month prior to admission to our hospital. At that time, the laboratory findings showed all studies, including a complete blood cell count, electrolytes, coagulation times and urinalysis, were within the reference limits, except for the total bilirubin (2.0 mg/dl) and direct bilirubin (0.5 mg/dl). His hepatitis studies were negative and tumor the markers, carcinoembryonic antigen and alpha-fetoprotein, were normal. An ultrasonography study of the abdomen showed normal findings of the liver, gallbladder, pancreas and kidneys. An esophagogastroduodenoscopic examination revealed a 1 cm sized polyp with central erosion on the anterior wall of the distal body and a 0.8 cm sized polyp on the anterior wall of the antrum. Therefore, endoscopic biopsies were performed which revealed hyperplastic polyps.
After obtaining informed consent, he underwent gastric EMR. Firstly, the margin around the polyp of the antrum was marked with a needle knife using a coagulation current. Epinephrine-mixed saline was injected beneath the mucosa to elevate the lesion. The lesion was retracted with grasping forceps and excised by closing the snare and an electrosurgical current. Bleeding was noted at the polypectomy site and controlled without difficulty with 3 hemoclips (Fig. 1A). Secondly, the polyp of the distal body was excised using the same method without bleeding (Fig. 1B).
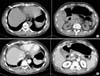
After the procedure, he complained of a severe epigastric and right upper quadrant (RUQ) pain, and physical examination showed RUQ and percussion tenderness. Immediately, the stomach was re-examined endoscopically but there was no evidence of a perforation of the stomach. The plain abdominal X-ray showed no intra-abdominal free air (Fig. 2). Nonenhanced computed tomography (CT) was performed and showed an air bubble abutting the wall of the gallbladder and a small quantity of fluid in the perihepatic space (Fig. 3A). He was treated with IV fluid and analgesics in the ward but his abdominal pain increased in intensity and became constant for 2 hours. A follow-up enhanced CT was performed, which revealed an increased fluid collection in the perihepatic space (Fig. 3B).
An emergency laparoscopic examination was performed under the impression of a perforation of the stomach. After general anesthesia, the endoscope was introduced into the peritoneal cavity through the infra-umbilical trocar, and revealed a small amount of bile in the perihepatic space. Three more trocars were inserted into the abdominal cavity and observed around the stomach, duodenum, and gallbladder. Bile leakage was noted through a pin point perforation of the body of the gallbladder, and no lesion of the stomach and duodenum was noted (Fig. 4A). An esophagogastroduodenoscopic examination was performed and no perforation was observed (Fig. 4B). The peritoneal cavity was filled with saline until the stomach was sunk under saline, and air was pushed in the stomach through a nasogastric tube, but no air leak was visible in the laparoscopic view. A laparoscopic cholecystectomy was performed easily and a closed-suction drain was placed in the subhepatic area. The resected gallbladder showed a normal-appearing mucosa with no stones. The postoperative period was uneventful and the patient was discharged on the 8th postoperative day. The microscopic findings of the gastric polyps were consistent with hyperplastic polyps.
DISCUSSION
EMR is a diagnostic and therapeutic procedure used widely for gastric polypoid lesions or some early gastric cancers. Major complications associated with gastric EMR include hemorrhage and perforation with a reported incidence of 1.5~25% and 0.06~5%, respectively.(10) However, injury to the neighboring organs is rare and most cases of gastric EMR associated perforations occur only in the wall of the stomach.
Hamaguchi et al.(9) reported a case of a gallbladder and stomach perforation during gastric EMR for gastric adenoma. They explained that the stomach and gallbladder might be in contact in the left lateral position during the procedure and the thickness of the gastric wall might be thinner considering the effects of a distention of the stomach. In addition, if a 4 mm-length needle knife is inserted into the stomach at a nearly perpendicular angle wall for marking, the needle could easily penetrate the stomach wall and reach the gallbladder, and a coagulation current might damage the stomach and gallbladder tissue. They concluded that the main reason for the perforation was current-induced tissue necrosis for marking the mucosa around a gastric lesion based on a histopathology examination of the perforated gastric wall.
However, in our case, the endoscopic and laparoscopic examination showed no evidence of a perforation of the stomach intraoperatively, even though an air bubble was present on the CT scan. Postoperatively, the perforation site of the resected and collapsed gallbladder could not be found in the gross and microscopic examination even by the pathologist. However, bile leakage through a pin-point perforation of the gallbladder was observed intraoperatively. Therefore, we suspect that the main reason for the perforation in our case was traumatic, i.e. the needle knife (the same type used in the case reported by Hamaguchi et al.(9), Olympus, Tokyo, Japan) (Fig. 5) used for marking or mucosal elevation might penetrate the stomach and gallbladder wall, but the perforation of the stomach wall might have sealed spontaneously.
Jeong et al.(10) classified a gastric perforation associated with gastric EMR into two types, "evident perforation" and "microperforation". They defined microperforation as follows: (1) no perforating defect of the gastric wall is observed during EMR; and (2) radiographic evidence of free air in the abdomen immediately after EMR. In addition, they reported an incidence of iatrogenic perforation and microperforation associated with gastric EMR of 4.16% (17/409 lesion) and 3.18% (evident perforation=4, microperforation =13), respectively. They suggested that microperforation of the gastric wall induced by gastric EMR can be managed successfully using a non-surgical approach, including fasting, nasogastric tube drainage and intravenous antibiotics. They also reported that 11 out of 13 microperforation patients recovered successfully with non-surgical management.
In our case, the stomach might have been perforated by the needle knife used for marking and sealed spontaneously, which is based on the findings of an air bubble on the CT scan and no evidence of a stomach perforation on the endoscopic and laparoscopic examination during surgery. If our patient had only such a perforation of the stomach without any other injury, he would have had no abdominal pain or required any further evaluation and treatment. However, he had suffered an injury to the gallbladder, bile accumulated gradually in the perihepatic space and his abdominal pain was aggravated. Therefore, an emergency operation was performed under the impression of a stomach perforation, but the gallbladder perforation was missed preoperatively and a definite diagnosis was made during surgery.
When a stomach perforation occurs and is observed during gastric EMR, it can be closed by applying endoscopic clips and managed conservatively. However, surgical management must be considered if a perforation is large and cannot be controlled with endoscopic management, and if clinical deterioration (e.g. hypotension, aggravation of abdominal pain) is observed during conservative management in a patient with a stomach perforation regardless of whether endoscopic management had been performed.(10) Our case complained of severe abdominal pain after the procedure but no evident perforation was observed during and after the procedure. However, a surgical approach was decided because that his pain had not improved but became aggravated and a follow-up CT scan revealed increased fluid collection in the perihepatic space.
Hamaguchi et al.(9) suggested that to avoid this complication, endoscopic ultrasonography should be performed before EMR to evaluate both the depth of the lesion as well as its relation to the surrounding organs. Our case was a gallbladder perforation that occurred during gastric EMR without evidence of a stomach perforation. Even if no perforation is observed during and after gastric EMR, the possibility of an injury to the neighboring organ and surgical approach must be considered if the patient reports unexplained severe and continuing pain.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download