Abstract
Purpose
The risk factors of pseudomembranous colitis (PMC) are well known. However, there have been no studies of PMC after gastrointestinal operation. The aim of this study was to evaluate the risk factors and to establish the guiding principles for PMC after gastrointestinal operation.
Methods
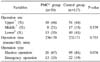
We performed a retrospective study of 39 PMC patients after gastrointestinal operation from January 2004 to December 2008. A control group of one hundred and seventeen matched to a PMC group by date of operation was chosen in a random fashion. Preoperative, operative, and postoperative factors of PMC were evaluated.
Results
The incidence of PMC after gastrointestinal operation was 0.63%. On univariate analysis, among preoperative factors, albumin, PT-INR and neutropenia were significant risk factors for PMC. There was no difference in the operative factors. Among postoperative factors, duration of cephalosporin, aminoglycoside, H2 blocker administration were significant risk factors for PMC after gastrointestinal operation. And transfusion, duration of NPO, length of stay in intensive care unit (ICU) and postoperative intraabddominal abscess, pneumonia were also significant risk factors. On multivariate analysis, the independent risk factors for PMC after gastrointestinal operation were duration of aminoglycoside administration, transfusion volume and length of stay in ICU. When period of study was divided by three months, incidence of PMC at a specific period was high. After limiting of prophylactic antibiotics, incidence of PMC fell to 0.36%.
Figures and Tables
Fig. 1
Overall incidence of pseudomembranous colitis. Arrow = prophylactic antibioticslimiting point.

References
1. Crabtree T, Aitchison D, Meyers BF, Tymkew H, Smith JR, Guthrie TJ, et al. Clostridium difficile in cardiac surgery: risk factors and impact on postoperative outcome. Ann Thorac Surg. 2007. 83:1396–1402.
2. Greenstein AJ, Byrn JC, Zhang LP, Swedish KA, Jahn AE, Divino CM. Risk factors for the development of fulminant Clostridium difficile colitis. Surgery. 2008. 143:623–629.
3. Lee KS, Shin WG, Jang MK, Kim HS, Park CJ, Lee JY, et al. Who are susceptible to pseudomembranous colitis among patients with presumed antibiotic-associated diarrhea? Dis Colon Rectum. 2006. 49:1552–1558.
4. Kyne L, Sougioultzis S, McFarland LV, Kelly CP. Underlying disease severity as a major risk factor for nosocomial Clostridium difficile diarrhea. Infect Control Hosp Epidemiol. 2002. 23:653–659.
5. Aslam S, Hamill RJ, Musher DM. Treatment of Clostridium difficile-associated disease: old therapies and new strategies. Lancet Infect Dis. 2005. 5:549–557.
6. Elliott B, Chang BJ, Golledge CL, Riley TV. Clostridium difficile-associated diarrhoea. Intern Med J. 2007. 37:561–568.
7. Surawicz CM, McFarland LV. Pseudomembranous colitis: causes and cures. Digestion. 1999. 60:91–100.
8. Kawamoto S, Horton KM, Fishman EK. Pseudomembranous colitis: spectrum of imaging findings with clinical and pathologic correlation. Radiographics. 1999. 19:887–897.
9. Fishman EK, Kavuru M, Jones B, Kuhlman JE, Merine DS, Lillimoe KD, et al. Pseudomembranous colitis: CT evaluation of 26 cases. Radiology. 1991. 180:57–60.
10. Ash L, Baker ME, O'Malley CM Jr, Gordon SM, Delaney CP, Obuchowski NA. Colonic abnormalities on CT in adult hospitalized patients with Clostridium difficile colitis: prevalence and significance of findings. AJR Am J Roentgenol. 2006. 186:1393–1400.
11. Kirkpatrick ID, Greenberg HM. Evaluating the CT diagnosis of Clostridium difficile colitis: should CT guide therapy? AJR Am J Roentgenol. 2001. 176:635–639.
12. Hsieh MM, Everhart JE, Byrd-Holt DD, Tisdale JF, Rodgers GP. Prevalence of neutropenia in the U.S. population: age, sex, smoking status, and ethnic differences. Ann Intern Med. 2007. 146:486–492.
13. Delmée M. Laboratory diagnosis of Clostridium difficile disease. Clin Microbiol Infect. 2001. 7:411–416.
14. Cloud J, Kelly CP. Update on Clostridium difficile associated disease. Curr Opin Gastroenterol. 2007. 23:4–9.
15. McFarland LV, Surawicz CM, Stamm WE. Risk factors for Clostridium difficile carriage and C. difficile-associated diarrhea in a cohort of hospitalized patients. J Infect Dis. 1990. 162:678–684.
16. Dharmarajan T, Sipalay M, Shyamsundar R, Norkus E, Pitchumoni C. Co-morbidity, not age predicts adverse outcome in Clostridium difficile colitis. World J Gastroenterol. 2000. 6:198–201.
17. Hashimoto M, Sugawara Y, Tamura S, Kaneko J, Matsui Y, Togashi J, et al. Clostridium difficile-associated diarrhea after living donor liver transplantation. World J Gastroenterol. 2007. 13:2072–2076.
18. Kent KC, Rubin MS, Wroblewski L, Hanff PA, Silen W. The impact of Clostridium difficile on a surgical service: a prospective study of 374 patients. Ann Surg. 1998. 227:296–301.
19. Kurd MF, Pulido L, Joshi A, Purtill JJ, Parvizi J. Clostridium difficile infection after total joint arthroplasty: who is at risk? J Arthroplasty. 2008. 23:839–842.
20. Bauer MP, Goorhuis A, Koster T, Numan-Ruberg SC, Hagen EC, Debast SB, et al. Community-onset Clostridium difficile-associated diarrhoea not associated with antibiotic usage--two case reports with review of the changing epidemiology of Clostridium difficile-associated diarrhoea. Neth J Med. 2008. 66:207–211.
21. Morris AM, Jobe BA, Stoney M, Sheppard BC, Deveney CW, Deveney KE. Clostridium difficile colitis: an increasingly aggressive iatrogenic disease? Arch Surg. 2002. 137:1096–1100.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download