Abstract
Retro-rectal cystic hamartoma (tailgut cyst), is an uncommon congenital developmental lesion, generally located in the retro-rectal space. Its diagnosis and approach is challenging because the retropelvic space is not familiar. We report a 51-year-old woman who presented with paresthesia and pain in perianal area. The magnetic resonance image showed high signal intensity on the T1-weighted image and iso to high signal intensity on the T2-weighted image of the retropelvic space and CT showed sacral bony defect. We chose the posterior approach for removal of the tailgut cyst. Histopathology exam of the retropelvic cyst revealed a multiloculated cyst containing abundant mucoid material lined by both squamous and glandular mucinous epithelium. The patient has recovered nicely with no recurrence. Tailgut cyst needs complete surgical excision for good prognosis. So, a preoperative high-resolution image and co-operation between neurosurgen and general surgeon would help to make safe and feasible diagnosis and surgical access.
Retro-rectal cystic hamartoma, also known as tailgut cyst, is an uncommon congenital developmental lesion, generally located in the retro-rectal space [1]. The position and rarity of it makes it difficult to diagnose and often leads to a misdiagnosis [2]. In addition, in women, the symptoms can mimic gynecological pathology and biopsy during the diagnosis can sometimes cause further harm [3]. Thus, preoperative MRI or CT is important for accurate diagnosis and appropriate surgical planning. We herein introduce a case demonstrating a successful total removal of a retrorectal mass using the posterior midline approach.
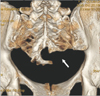
A 51-year-old woman was referred to our neurosurgery department from gynecology and general surgery due to paresthesia and pain in perianal area. By then, her symptoms had persisted for 2 months. Previously, she had been examined in general surgery and in gynecology. After the gynecologist confirmed an abnormal mass in the retrorectal space by pelvic MRI and CT, she was admitted to our department for surgery. There were no abnormal findings by digital rectal examination or on perianal skin. Pelvic CT showed a bony defect on the lower sacral bone near the cyst (Fig. 1). Pelvic MRI with gadolinium enhancement showed high signal intensity on the T1-weighted image and iso to high signal intensity on the T2-weighted image. The size of the mass was about 6 cm, of which was a multilobulated mass on the sacrococcygeal area. The uterus was enlarged and heterogeneously enhanced (Fig. 2). Surgery was performed with the patient in prone position under general anesthesia. After making a 10-cm long midline skin incision, 3 cm distant from the anus, we exposed the lamina by dissecting the soft tissue. The bony defect was palpable above the cyst wall. The additional laminectomy was performed to take the large mass out. While performing a careful cyst dissection, we realized that the demarcation of the cyst was good, and there was no evidence of cyst rupture. The cyst contained soft suctionable yellowish material of creamy consistency. A small incision was made on the cyst wall, and the cystic contents were aspirated with a syringe. After the cyst wall was sutured, marginal cyst dissection was performed although part of the cyst wall was stuck to other tissue. The contents were removed with no significant spillage into the retropelvic cavity. Complete excision of the retro-rectal tumor (which was fixed to the apex of the coccyx) using posterior midline approach was performed (Fig. 3). Histopathology exam of the retropelvic cyst revealed a multiloculated tailgut cyst containing abundant mucoid material lined by both squamous and glandular mucinous epithelium (Fig. 4). The patient has hence recovered nicely and showed no evidence of recurrence.
Tailgut cyst, also known as retrorectal cyst hamartoma, is a rare congenital lesion that most often occurs in the retro-rectal space. Cases of such retrorectal lesion is estimated at 1 in 40,000 bases [4]. The retrorectal space is a space bound anteriorly by the mesorectum and posteriorly by the sacrum. The superior border is formed by peritoneal reflection and the inferior border is formed by the rectosacral fascia. The lateral borders of the retrorectal space are formed by the uterus, the iliac vessels, the sacral nerve roots and the lateral stalks of the rectum [5]. This space contains loose connective tissue, the middle sacral, iliolumbar and middle hemorrhoid vessels, branches of sympathetic and parasympathetic nervous systems, and lymphatics [6]. Most origins of these are known as congenital and neurogenic (approximately 60%), which form aberrant remnants of postanal primitive gut on the incomplete embryogenesis [7]. It is more common among middle-aged women.
The most common symptoms of tailgut cyst are pain and constipation followed by rectal fullness and difficulty in passing urine. Other symptoms are constipation, low abdominal pain, and swelling on the coccyx or gluteal area. In general, there were no skin defects or other abnormal signs except for mild swelling, and a palpable nontender mass on the retrorectal space was found during the digital rectal exam. The rectosigmoidoscopy showed no fistula between the gut and retropelvic space although huge mucosa were occasionally elevated. Because the diagnosis is usually slow and difficult until its size grows larger and the incidence of retrorectal lesions occurs, the possibility of tailgut cyst is very rarely considered [8]. The common misdiagnosis includes chordomas, anterior sacral meningoceles, developmental cyst consisting of enteric duplication cyst, dermoid cysts, epidermoid cysts, and teratomas. Half of tailgut cysts are diagnosed only incidentally and require high-resolution imaging tools, such as pelvic MRI or 3 dimensional-CT as well as preoperative gynecologic evaluation [7]. A pelvic CT helps to distinguish cysts from solid contents and to evaluate sacral bone abnormalities and the relationship between organs and muscles. A pelvic MRI could confirm accompaniment with tethered cord and meningocele. In female patients, a gynecologist should first rule out anorectal or other organ abnormalities. Some articles reported the availability of preoperative biopsy, but most other cases were obtained by the histologic diagnosis through the operative field. This is because needle biopsies carry the risk of bleeding, infection, and dissemination of cells into the peritoneal cavity. In addition, there are some reports of meningitis via the rupture of cysts.
The golden standard of treating tailgut cyst is complete surgical excision. If removed incompletely, the risk of hemorrhage, infection, malignant degeneration, and compressing nearby organs remains [1]. A careful approach makes a successful surgical treatment of the retrorectal tumor. In consideration of its location and the relationship with the adjacent organs, the approach should be decided accordingly. In cases where the mass is located below S3 or sacral promontory and can be palpated on rectal examination, the posterior approach is recommended. If it is above S3 or small (<8 cm) and is a benign tumor, the anterior approach is recommended. If there is a large lesion in the intermediate position, it may require both the anterior and posterior approach. The anterior approach gives a good view of pelvic structures, iliac vessel and ureter, and the posterior approach is convenient for masses of posterior-caudal type. In our case, because the mass was located on the posterocaudal retropelvic space and accompanied with sacral bony deformity, the posterior approach was chosen to remove it completely. Most cases of tailgut cyst are treated from a posterior approach. There have been some reported cases of the multiple tailgut cysts in the retro-rectal area, which were treated by transanal approach using the reconstruction of the rectal wall [9]. And for minimal invasive surgery, there are cases of the laparoscopic approach and trans-anal endoscopic microsurgery with low morbidity [7].
Histopathology findings of tailgut cyst are stratified squamous and columnar epithelium and dense fibrous connective tissue with a large area of hyperplastic smooth muscle bundles and linear deposition of calcium salts. Tailgut cysts with neuroendocrine tumors have been rarely reported. The main cystic component and presacral location suggest a higher probability of a tailgut cyst, but if it has some solid portion, progressive neurologic symptoms and swelling of local lymph nodes, it might be a malignant transformation from the epithelial cells of the tailgut cyst [10]. Tailgut cyst is a rare retropelvic mass. It needs complete surgical excision for good prognosis. Therefore, preoperative high-resolution imaging and co-operation between gynecologist and general surgeon would help to make safe and feasible diagnoses and surgical access.
Figures and Tables
Fig. 2
Pelvic MRI with gadolinium enhancement showing Iso to high signal intensity on T2-weighted image (A: sagittal, B: axial). Size of mass was about 6 cm, of which the multilobulated mass was on sacrococcygeal area (red arrow). Uterus was enlarged and heterogeneously enhanced.
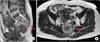
Fig. 3
(A) After sacral laminectomy, cyst demonstrating well-marginated and capsulated, connected with some dural ends. Small incision was made on cyst wall, and cystic contents were aspirated with syringe. (B) Cyst contained soft suction-able yellowish material of creamy consistency. After cyst wall was sutured, marginal cyst dissection was performed although part of cyst wall adhered to other tissue. Contents were removed with no significant spillage into retropelvic cavity.

Fig. 4
Histopatholgic photomicrographs of tailgut cyst showing smooth muscle proliferation (A) and abundant mucoid material lined by both squamous and glandular mucinous epithelium (B). And cystic wall was lined with transition zone of keratinized squamous, and glandular epithelium, columnar cell involving intracytoplasmic mucin on hematoxylin-eosin stained sections (×100).

References
1. Lim SW, Huh JW, Kim YJ, Kim HR. Laparoscopy-assisted resection of tailgut cysts: report of a case. Case Rep Gastroenterol. 2011; 5:22–27.
2. Lin C, Jin K, Lan H, Teng L, Lin J, Chen W. Surgical management of retrorectal tumors: a retrospective study of a 9-year experience in a single institution. Onco Targets Ther. 2011; 4:203–208.
3. Neale JA. Retrorectal tumors. Clin Colon Rectal Surg. 2011; 24:149–160.
4. Jao SW, Beart RW Jr, Spencer RJ, Reiman HM, Ilstrup DM. Retrorectal tumors. Mayo Clinic experience, 1960-1979. Dis Colon Rectum. 1985; 28:644–652.
5. Hassan I, Wietfeldt ED. Presacral tumors: diagnosis and management. Clin Colon Rectal Surg. 2009; 22:84–93.
6. Ghosh J, Eglinton T, Frizelle FA, Watson AJ. Presacral tumours in adults. Surgeon. 2007; 5:31–38.
7. Rosa G, Lolli P, Vergine M, El-Dalati G, Malleo G. Surgical excision of developmental retrorectal cysts: results with longterm follow-up from a single institution. Updates Surg. 2012; 64:279–284.
8. Charalampakis V, Stamatiou D, Christo-doulakis M, Kafousi M, Chryssou E, de Bree E, et al. Large presacral tailgut cyst with a carcinoid tumor in a male: report of a case. Surg Today. 2014; 44:961–966.
9. Kildusis E, Samalavicius NE. Surgical management of a retro-rectal cystic hamartoma (tailgut cyst) using a trans-rectal approach: a case report and review of the literature. J Med Case Rep. 2014; 8:11.
10. Mitsuyama T, Kubota M, Nakamura Y, Yuzurihara M, Hoshi K, Okada Y. Neuroendocrine tumor arising from tailgut cyst with spinal cord tethering: case report and literature review. Spine J. 2015; 15:e1–e8.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download