Abstract
Purpose
Despite recommendations for introducing student internships (SI) in undergraduate medical education in Korea, the feasibility of surgical SIs has not been demonstrated in the Korean context. We thus identified tasks that could be performed by surgical student interns in a Korean education hospital.
Methods
The opinions of surgery clerkship directors of medical schools nationwide, regarding the tasks, symptoms and signs, disease entities, and procedures that student interns could perform in their hospitals, were subjected to descriptive analysis.
Results
Out of the 41 medical schools in Korea, 32 responded. Five implemented an optimal-quality SI program. Two schools considered third-year clerkship as SI. The respondents replied that student interns could be involved in basic nonspecific tasks such as history taking, physical examination, medial recording, reporting patients' status, and assisting during surgery. However, more surgery-specific tasks such as perioperative management or caring for a patient with acute abdominal pain were considered difficult for student interns to encounter in the Korean context.
Student internship (SI) is a component of the clinical education program for fourth-year students offered by most medical schools in the United States [1]. Originally, the SI was initiated to compensate for the shortage of resident resources during World War II. In such a program, unlike the third-year clerkship, senior medical students served as interns with progressively graded clinical responsibility, which had originally been the role of residents [2].
Nowadays, the SI is considered as a program to prepare fourth-year students for the first year of postgraduation [3]. The SI offers greater and complex clinical exposure to student interns, which enhances their experience in handling physicians' tasks [4,5]. Thus, the SI integrates clinical knowledge, skills, and attitudes before graduation, and can reduce the transition gap from the third-year clerkship to the first year of postgraduation. It has been recommended that such SI programs should allow fourth-year students to replace the first postgraduate year completely, under the supervision of senior house staff [3].
Several studies have suggested that the SI should be incorporated into the undergraduate medical education in Korea [6,7]. The Korean Academy of Medical Sciences [7] pointed out that the current intern training system is inefficient and that the duration of residency training should be modified. The Academy had proposed the abolishment of the intern training system and that SI in the undergraduate curriculum could replace some part of the intern program [8]. Some schools have reported successful implementation of the SI program [9,10]. Thus, SI is expected to be established nationwide in the future.
However, whether SI is feasible in Korea, especially in the surgery department, has not been determined. SI has not yet gained popularity in Korea, and Korean patients and health care professionals are not accustomed to a system in which medical students take up the role of an intern [9]. Furthermore, previous articles about SI usually covered SI in only internal medicine [3,11,12,13,14]. Articles about SI in surgery [15,16] are rare and examined only a limited number of issues. In addition, the Korean Association of Medical Colleges (KAMC) and the Korean National Licensing Exam for Clinical Skills Exam announced the competencies that graduates need to achieve. However, there is as yet no nationwide study that explored if it is feasible for students to be in charge of such clinical tasks during a surgical SI program in the Korean context.
Surgical educators should prepare for the nationwide introduction of the SI program. When setting up SI in surgery, the features of surgery should be considered. To develop a program that is safe for both patients and students in Korea, we should understand which tasks student interns can perform in real surgical situations in Korea. To understand the circumstances in surgical education in Korean hospitals, we should first examine the current situation of hospitals. Each training hospital may have a different curriculum and training environment. Patients' problems and disease entities can differ according to the characteristics of the region or hospital system.
The present study therefore investigated which tasks surgical student interns could perform in a hospital in Korea, and discussed the requirements for the successful implementation of a surgical SI program.
We developed a questionnaire about the competencies that should be addressed in a surgical SI. We gathered potentially relevant competencies from competency based learning objectives of basic medical education published by the KAMC [17], objectives of the Korean National Licensing Exam for Clinical Skills Exam, the guide for the internal medicine subinternship curriculum [4], and from previous studies. KAMC's learning objectives are composed of general objectives and specific objectives. General objectives introduce general tasks that students have to perform after graduation. Specific objectives are described according to clinical presentation, which include common and important symptoms, and signs or laboratory findings that patients present to a doctor [18]. KAMC chose 104 clinical presentations as key objectives. KAMC's specific objectives include related diseases and procedural skills. The Korean National Licensing Exam's objectives for the skills exam are also composed of common symptoms, signs, and laboratory findings, which can be evaluated by objective structured clinical examination.
Competencies were categorized into four areas, which are similar to KAMC's learning objectives. The first area includes tasks that student interns can perform in surgery. The second area is related to the symptoms and signs that student interns can encounter while performing their duties. The third area pertains to disease entities for which student interns can provide medical care. The fourth area entails procedures that can be performed by student interns. The authors listed all of the competencies and rated their importance from 1 to 5 independently. The scores were summed and discussed in consensus meetings to reach an agreement on items. Total concurrency was achieved after three consensus meetings. The survey finally contained 46 items across the four topics.
The survey also examined the status of the existing SI program at the medical schools. The instruction about the definition and the roles of student interns is added to the survey. The questionnaire asked respondents to rate the degree of possibility that student interns could practice in their education hospital. We used a five-point Likert-type scale (1, impossible; 2, rarely possible; 3, neutral; 4, possible; and 5, absolutely possible). We required respondents to add free-text responses. This tool was not pilot-tested in advance.
In October 2012, we mailed a written survey to clerkship directors of the surgical department at 41 medical schools in Korea. We asked the recipients to complete the questionnaire if they were in charge of the surgical undergraduate or clerkship education at their departments. If not, we asked them to forward the survey to the most appropriate faculty. Some of the medical schools were affiliated with multiple clinical sites; therefore, we required respondents to answer questions based on the overall medical school environment.
We sent another mail in November 2012 to the department of surgery in medical schools that had not responded. We contacted nonrespondents up to four times by e-mail, regular mail, fax, and telephone.
We summarized the responses from the SI section using descriptive statistics. The survey had a Cronbach α reliability coefficient of 0.933. Statistics were computed using IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA). We interpreted possibility ratings of 1 and 2 as "tasks are impossible for student interns," and ratings of 3, 4, and 5 as "tasks are possible for student interns."
Out of the 41 medical schools, 32 responded to the survey. Among them, seven (21.9%) were national schools and 25 (78.1%) were private. Fourteen schools (43.8%) were located in Seoul, Incheon, and Gyeonggi-do. Eight schools (25.0%) were located in Gangwon-do and Chuncheong-do. Eight other schools (25.0%) that responded were located in Gyeongsang-do, and two others (6.3%) in Jeolla and Jeju-do.
Five schools (15.6%) replied that the SI program already existed and that the roles of student interns are different from those of clinical clerkships. Four (12.5%) reported that their SI program was offered to fourth-year students, but that it is the same as the clinical clerkship for third-year medical students. Two schools answered that they did not have SI programs, but that they considered their third-year medical students as student interns. The other 21 schools reported that they did not have any SI programs in the third or final year.
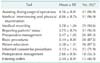
Among the 10 items, the respondents thought that it was highly possible for student interns to carry out tasks such as assisting in surgical operations (96.9%), medical interviewing and physical examination as an attending doctor (96.9%), and medical recording (90.6%), and reporting patients' status (90.6%). On the other hand, few respondents identified the tasks of postoperative management (56.3%) and entering orders (46.9%) as possible (Table 1).
One respondent emphasized the importance of physical examination such as breast or anorectal exams. He insisted that it is the duty of student interns to conduct full physical examinations on patients.
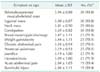
Among the 12 items, the respondents thought that it was highly possible for student interns to encounter skin/subcutaneous/skeletal mass (93.8%), inguinal mass (93.8%), constipation (93.8%), and neck mass (90.6%). They thought acute abdominal pain and burn/cold injury were less possible to be examined by student interns (Table 2).
Other than these, the respondents recommended abdominal distension, vomiting, claudication, and soft tissue infection in their free responses.
Respondents thought that skin tumor, hernia, benign breast diseases, neck or thyroid tumor, acute appendicitis, and benign anal diseases were highly suitable diseases for student interns to provide medical care. They also responded positively towards gallstones or chronic cholecystitis, and acute cholecystitis (Table 3). Some of the respondents recommended that diverticulitis and ischemic colitis could be added as suitable diseases for student interns. One respondent commented that there are many cancer patients in most Korean university hospitals and that we therefore need to provide opportunities for the students to work with patients with cancer.
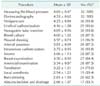
Among the 16 items, respondents thought it was highly possible for student interns to perform tasks such as measuring blood pressure (100%), checking the electrocardiogram (100%), dressing wounds (96.9%), venipuncture (93.8%), nasogastric tube insertion (93.8%), and urethral catheterization (90.6%). Local anesthesia (59.4%) and abscess incision and drainage (53.1%) were thought to be less possible (Table 4).
Some of the respondents recommended central venous catheterization and aseptic preparation of the operation field, including scrubbing, gowning, gloving, and draping. Some suggested that we should divide skills into basic skills without supervision and advanced skills with supervision needed.
This study is the first such nationwide study in Korea. We tried to investigate the Korean surgical context and surgical educators' perspectives. Students' experience in surgery is expected to be different from those in internal medicine. Clinical practice in surgery includes participation in operations and perioperative care. Competent procedural skills and prompt decision-making are needed while managing surgical patients. This study can be helpful for educators who wish to introduce an SI program in their institution, which previously had no such program.
The present study showed that 21 schools did not have any SI programs in surgery. The questionnaire in this study did not ask whether these schools had an SI program or why they did not implement SI in surgery. However, it is reasonable to assume that their surgical departments were not required to have SI programs because their medical schools did not encourage such programs.
This study revealed that there is a misconception about SI. Only five schools offered the SI program to final-year students. Some schools did not discriminate between SI and clinical clerkships. These findings indicate that the role of student interns is unclear. When establishing an SI program in a medical school and hospital, it is desirable to share the definition and explicit role of student interns with all members in the medical schools and hospitals. The SI is often termed as "subinternship," but the term "subintern" creates further confusion about the role of student interns. The term "subintern" may indicate being "subordinate to an intern," which is incorrect. The actual role of a student intern is a student physician in charge. Therefore, we think "student interns" or "student physicians in charge" are more suitable compared to "subintern."
In studies conducted in the United States, student interns in surgery cited patient and perioperative care events as the most frequent critical incidents [15]. These are surgery-specific tasks that surgical educators should offer to surgical student interns. However, our results showed that it is less possible for Korean student interns to perform surgery-specific tasks in an SI. Among the tasks given to students, while it was considered acceptable for them to assist in a surgery, it was reported as inappropriate to involve them in postoperative care. This means that even though students could choose a surgical SI in order to prepare to be surgeons, they would not be able to experience enough relevant activities during the SI. Students can experience activities such as history taking, physical examination, and reporting a patient's status during an SI in other departments such as internal medicine or pediatrics. Studies have found that students desired to improve their skills related to basic surgical patient care and knowledge in the field of surgery, and that surgical SI influences many students when they choose a specialty [16]. Therefore, an SI program in surgery should provide surgery-specific tasks to student interns.
We recommend 12 tasks for surgical student interns: (1) surgical patient encounters such as history taking, physical examination, and patient education; (2) medical recording; (3) reporting a patient's status; (4) preoperative management; (5) entering orders; (6) obtaining informed consent; (7) performing basic procedures; (8) assisting surgeries in the operation theatre; (9) prevention and early detection of surgical complications; (10) working in the night duty; (11) personal and professional development; and (12) team work. Breast and anorectal exam is an essential part of the physical examination conducted in surgery. Therefore, we suggest not avoiding these examinations. Some faculties and residents encourage their student interns to review textbooks or join a journal club, but it is desirable to allow student interns to perform more practical tasks in the surgical field.
Among the symptoms, signs and diseases, acute abdomen and heat/cold injuries are surgery-specific areas. However, our study revealed that it was less possible for student interns to encounter them. We recommend that surgical educators include abdominal pain, neck mass, abdominal or inguinal mass, anorectal symptoms, breast symptoms, and soft tissue infections as major symptoms and signs that student interns encounter in surgery. We think that student interns should be able to care for cancer patients unless these patients are expected to have severe surgical complications. We expect that student interns can manage basic gastrointestinal cancer, thyroid neoplasm, hernia, benign anorectal diseases, breast neoplasm, and soft tissue abscess without complications as a primary charge.
Our study also revealed that it was highly possible for students to perform technical skills rather than other tasks. This implies that the Korean hospital context favors technical skill performance of the students. Lindeman reported that most surgery student interns evaluated technical skills education as helpful [16]. We recommend that the training of student interns focuses on technical skills related with surgical procedures. Surgery-specific skills training such as wound dressing, sutures, local anesthesia, and abscess incision and drainage is meaningful for student interns in surgery.
Societal and system support should take precedence in order for SI to take root in Korea. Kim [19] emphasized the limitation of legal practice in clinical practice for student interns, even though he confirmed the logistical authorization of medical student's active participation in clinical practice for their learning. Student interns' ordering is expected to be the most difficult part to establish when considering the Korean clinical context. Therefore, we think that the legal regulations should be modified first. To improve patient safety, it could be helpful to verify if the student is competent enough to encounter a patient as a student intern before entering an SI program.
In addition, to ensure appropriate implementation of SI in surgery, curriculum improvement and perception change of educators and students is necessary. We should focus more on educational continuity from undergraduate education through graduate medical education. Clinical clerkship in the third year should allow medical students to participate in their practice more actively, to guarantee patient safety during their SI. Preclerkship curriculum should support students in honing their ability to care for patients safely. During the SI, educators should support students in integrating their clinical experience and competencies in an individualized manner. Assessment and evaluation should also be improved. Cacamese et al. [20] reported grade inflation in internal medicine SI. In addition, student interns should be treated as students, not employees. SI directors have to understand what student interns are, and what duties they should perform. Medical schools and departments of surgery should support subinternship directors in their coordination of the SI program in surgery [21].
This study has some limitations. First, the questionnaire that was developed for this study was not piloted. Second, we restricted our methodology to a survey, and did not include complementary tools such as interviews. Therefore, we could not explore the underlying background or obstacles more specifically. Third, we performed the survey nationally, but nine schools did not respond to the survey despite repeated attempts. Fourth, we cannot verify whether the respondents had adequate knowledge of the definition of SI or concept of curriculum.
In conclusion, it is necessary to determine a specific role for student interns, encourage student interns to perform surgeryspecific tasks, provide societal and system support, and conduct curriculum renovation to establish the SI program.
Figures and Tables
References
1. Fagan MJ, Curry RH, Gallagher SJ. The evolving role of the acting internship in the medical school curriculum. Am J Med. 1998; 104:409–412.
2. Ludmerer K. Time to heal: American medical education from the turn of the century to the era of managed care. New York: Oxford University Press;1999.
3. Sidlow R. The structure and content of the medical subinternship: a national survey. J Gen Intern Med. 2001; 16:550–553.
4. Reddy S, Faga MJ, Mechaber AJ, Green EH, Sidlow R. Internal Medicine Subinternship Curriculum [Internet]. Alexandria (VA): Alliance for Academic Internal Medicine;c2015. cited 2015 Mar 17. Available from: http://connect.im.org/p/cm/ld/fid=373.
5. Green EH, Fagan MJ, Reddy S, Sidlow R, Mechaber AJ. CDIM Subinternship Task Force. Advances in the Internal medicine subinternship. Am J Med. 2002; 113:769–773.
6. Ko YW, Kim KM, Kim KS, Kim SD, Kim JK, Bae JY, et al. A study on development of compulsory clinical training program for quality improvement of medical physicians. Seoul: Ministry of Health Welfare;2004.
7. Wang GC, Kim DH, Kim SH, Park WB, Ahn DS, Yu KH, et al. A study on reformation of post-graduate medical education system in Korea. Seoul: Korean Academy of Medical Sciences;2010.
8. Kim JH, Jung SS, Lee IK, Song BJ, Moon JH, Jang YS, et al. Status and prospect of workforce requirement for surgery in republic of Korea. J Korean Surg Soc. 2011; 81:363–373.
9. Roh HR, Chae G, Yang JH. Implementation of student internship with intern-level responsibility. Korean J Med Educ. 2007; 19:47–57.
10. Park GH, Lee YD, Oh JH, Choi IS, Lim YM, Kim YI. Program development of student internship (subinternship) in Gachon Medical School. Korean J Med Educ. 2003; 15:113–130.
11. Sidlow R, Mechaber AJ, Reddy S, Fagan M, Marantz PR. The internal medicine subinternship: a curriculum needs assessment. J Gen Intern Med. 2002; 17:561–564.
12. Green EH, Hershman W, Sarfaty S. The value of the subinternship: a survey of fourth year medical students. Med Educ Online. 2004; 9:7.
13. Aiyer MK, Vu TR, Ledford C, Fischer M, Durning SJ. The subinternship curriculum in internal medicine: a national survey of clerkship directors. Teach Learn Med. 2008; 20:151–156.
14. Harrell HE, Aiyer MK, Appel JL, Gliatto P, Dhaliwal G, Sweet M. Primer to the Internal Medicine Subinternship. A guide produced by the clerkship Directors in Internal Medicine [Internet]. Alexandria(VA): Alliance for Academic internal Medicine;2015. cited 2015 Mar 17. Available from: http://connect.im.org/p/cm/ld/fid=666.
15. Valentino J, Blue AV, Donnelly MB, Stratton TD. The most valuable critical incidents in a 4th-year acting internship in surgery. Teach Learn Med. 1999; 11:75–79.
16. Lindeman BM, Lipsett PA, Alseidi A, Lidor AO. Medical student subinternships in surgery: characterization and needs assessment. Am J Surg. 2013; 205:175–181.
17. Korean Association of Medical Colleges. Learning outcomes of basic medical education: clinical competency-centered. Seoul: Academia;2012.
18. Mandin H, Harasym P, Eagle C, Watanabe M. Developing a "clinical presentation" curriculum at the University of Calgary. Acad Med. 1995; 70:186–193.
19. Kim YI. Medical practice by medical students. Korean J Med Educ. 1992; 4:34–38.
20. Cacamese SM, Elnicki M, Speer AJ. Grade inflation and the internal medicine subinternship: a national survey of clerkship directors. Teach Learn Med. 2007; 19:343–346.
21. Clerkship Directors in Internal Medicine Subinternship Task Force. Aiyer M, Appel J, Fischer M, Fitz M, Vu TR, et al. The role of the internal medicine subinternship director in the 21st century. Am J Med. 2008; 121:733–737.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download