Abstract
Purpose
Mycoplasma pneumoniae (MP) is a major cause of community-acquired pneumonia in children. Since 2000, emerging macrolide-resistant MP has been reported. Three epidemics of MP pneumonia have occurred in Korea during the past 10 years: 2006–2007, 2011, and 2015. We investigated the differences in MP pneumonia of each epidemic in terms of clinical, laboratory, and radiologic perspectives.
Methods
We retrospectively analyzed 529 medical records of children (1–18 years of age) who were admitted and diagnosed with MP pneumonia at Kangbuk Samsung Hospital during the past 3 epidemic periods. We compared the clinical, laboratory, and radiologic characteristics of MP pneumonia among individual epidemics and between children younger and older than 6 years of age.
Results
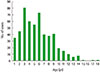
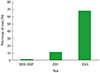
The mean age of the patients was 5.7 years old, which had increased by each epidemic and showed the highest (6.3 years old) in 2015 compared to previous epidemics. Among 3 epidemics, there were no sex differences. The duration of fever after admission and hospitalization, and the percentage of lobar pneumonia and use of systemic steroids increased significantly in 2015 epidemic. Since 2006, the mean levels of erythrocyte sedimentation rate and lactate dehydrogenase had increased and in 2015 it marked the highest. Children older than 6 years showed a higher proportion of lobar pneumonia and pleural effusion as well as longer duration of fever (before and after admission) and hospitalization days than those younger than 6 years.
Figures and Tables
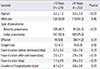
Table 1
Comparison of demographic data, duration of fever and hospitalization among 3 recent epidemics

Table 2
Comparison of the type of pneumonia and complications among 3 recent epidemics

Table 3
Multiple linear regression analysis of laboratory findings among 3 recent epidemics

Table 4
Comparison of clinical characteristics by the age of 6 years
References
1. Waites KB, Talkington DF. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev. 2004; 17:697–728.

2. Foy HM, Kenny GE, Cooney MK, Allan ID. Long-term epidemiology of infections with Mycoplasma pneumoniae. J Infect Dis. 1979; 139:681–687.

3. Hauksdottir GS, Love A, Sigurdardottir V, Jonsson T. Outbreaks of Mycoplasma pneumoniae infections in Iceland 1987 to 1997: a ten and a half years review. Eur J Epidemiol. 1999; 15:95–96.
4. Ito I, Ishida T, Osawa M, Arita M, Hashimoto T, Hongo T, et al. Culturally verified Mycoplasma pneumoniae pneumonia in Japan: a long-term observation from 1979-99. Epidemiol Infect. 2001; 127:365–367.

5. Lind K, Jensen JS, Clyde WA Jr. A seroepidemiological study of Mycoplasma pneumoniae infections in Denmark over the 50-year period 1946-1995. Eur J Epidemiol. 1997; 13:581–586.
6. Pönkä A. Occurrence of serologically verified Mycoplasma pneumoniae infections in Finland and in Scandinavia in 1970-1977. Scand J Infect Dis. 1980; 12:27–31.

7. Rastawicki W, Kałuzewski S, Jagielski M. Occurrence of serologically verified Mycoplasma pneumoniae infections in Poland in 1970-1995. Eur J Epidemiol. 1998; 14:37–40.
8. Ma YJ, Wang SM, Cho YH, Shen CF, Liu CC, Chi H, et al. Clinical and epidemiological characteristics in children with community-acquired mycoplasma pneumonia in Taiwan: a nationwide surveillance. J Microbiol Immunol Infect. 2015; 48:632–638.

9. Sztrymf B, Jacobs F, Fichet J, Hamzaoui O, Prat D, Avenel A, et al. Mycoplasma-related pneumonia: a rare cause of acute respiratory distress syndrome (ARDS) and of potential antibiotic resistance. Rev Mal Respir. 2013; 30:77–80.
10. Wang RS, Wang SY, Hsieh KS, Chiou YH, Huang IF, Cheng MF, et al. Necrotizing pneumonitis caused by Mycoplasma pneumoniae in pediatric patients: report of five cases and review of literature. Pediatr Infect Dis J. 2004; 23:564–567.

11. Shen Y, Zhang J, Hu Y, Shen K. Combination therapy with immune-modulators and moxifloxacin on fulminant macrolide-resistant Mycoplasma pneumoniae infection: a case report. Pediatr Pulmonol. 2013; 48:519–522.

12. Katsushima Y, Katsushima F, Suzuki Y, Seto J, Mizuta K, Nishimura H, et al. Characteristics of Mycoplasma pneumoniae infection identified on culture in a pediatric clinic. Pediatr Int. 2015; 57:247–252.

13. Liu Y, Ye X, Zhang H, Xu X, Li W, Zhu D, et al. Antimicrobial susceptibility of Mycoplasma pneumoniae isolates and molecular analysis of macrolide-resistant strains from Shanghai, China. Antimicrob Agents Chemother. 2009; 53:2160–2162.

14. Xin D, Mi Z, Han X, Qin L, Li J, Wei T, et al. Molecular mechanisms of macrolide resistance in clinical isolates of Mycoplasma pneumoniae from China. Antimicrob Agents Chemother. 2009; 53:2158–2159.

15. Hong KB, Choi EH, Lee HJ, Lee SY, Cho EY, Choi JH, et al. Macrolide resistance of Mycoplasma pneumoniae, South Korea, 2000-2011. Emerg Infect Dis. 2013; 19:1281–1284.
16. Hsieh YC, Tsao KC, Huang CG, Tong S, Winchell JM, Huang YC, et al. pneumoniae. Pediatr Infect Dis J. 2012; 31:208–209.
17. Lee KY, Lee HS, Hong JH, Lee MH, Lee JS, Burgner D, et al. Role of prednisolone treatment in severe Mycoplasma pneumoniae pneumonia in children. Pediatr Pulmonol. 2006; 41:263–268.

18. Luo Z, Luo J, Liu E, Xu X, Liu Y, Zeng F, et al. Effects of prednisolone on refractory mycoplasma pneumoniae pneumonia in children. Pediatr Pulmonol. 2014; 49:377–380.

19. Wang M, Wang Y, Yan Y, Zhu C, Huang L, Shao X, et al. Clinical and laboratory profiles of refractory Mycoplasma pneumoniae pneumonia in children. Int J Infect Dis. 2014; 29:18–23.

20. Eun BW, Kim NH, Choi EH, Lee HJ. Mycoplasma pneumoniae in Korean children: the epidemiology of pneumonia over an 18-year period. J Infect. 2008; 56:326–331.

21. Kim EK, Youn YS, Rhim JW, Shin MS, Kang JH, Lee KY. Epidemiological comparison of three Mycoplasma pneumoniae pneumonia epidemics in a single hospital over 10 years. Korean J Pediatr. 2015; 58:172–177.

22. Kim NH, Lee JA, Eun BW, Shin SH, Chung EH, Park KW, et al. Comparison of polymerase chain reaction and the indirect particle agglutination antibody test for the diagnosis of Mycoplasma pneumoniae pneumonia in children during two outbreaks. Pediatr Infect Dis J. 2007; 26:897–903.

23. Yoo SJ, Oh HJ, Shin BM. Evaluation of four commercial IgG- and IgM-specific enzyme immunoassays for detecting Mycoplasma pneumoniae antibody: comparison with particle agglutination assay. J Korean Med Sci. 2007; 22:795–801.

24. Defilippi A, Silvestri M, Tacchella A, Giacchino R, Melioli G, Di Marco E, et al. Epidemiology and clinical features of Mycoplasma pneumoniae infection in children. Respir Med. 2008; 102:1762–1768.

25. Miyashita N, Kawai Y, Inamura N, Tanaka T, Akaike H, Teranishi H, et al. Setting a standard for the initiation of steroid therapy in refractory or severe Mycoplasma pneumoniae pneumonia in adolescents and adults. J Infect Chemother. 2015; 21:153–160.

26. Zhang Y, Zhou Y, Li S, Yang D, Wu X, Chen Z. The clinical characteristics and predictors of refractory Mycoplasma pneumoniae pneumonia in children. PLoS One. 2016; 11:e0156465.

27. Kawamata R, Yokoyama K, Sato M, Goto M, Nozaki Y, Takagi T, et al. Utility of serum ferritin and lactate dehydrogenase as surrogate markers for steroid therapy for Mycoplasma pneumoniae pneumonia. J Infect Chemother. 2015; 21:783–789.

28. Choi SH, Park EY, Jung HL, Shim JW, Kim DS, Park MS, et al. Serum vascular endothelial growth factor in pediatric patients with community-acquired pneumonia and pleural effusion. J Korean Med Sci. 2006; 21:608–613.

29. Shin JH, Shim JW, Kim DS, Shim JY. TGF-beta effects on airway smooth muscle cell proliferation, VEGF release and signal transduction pathways. Respirology. 2009; 14:347–353.

30. Yamazaki T, Kenri T. Epidemiology of Mycoplasma pneumoniae infections in Japan and therapeutic strategies for macrolide-resistant M. pneumoniae. Front Microbiol. 2016; 7:693.

31. Maroushek SR. Principles of antimycobacterial therapy. In : Kliegman RM, Stanton BF, St Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier;2015. p. 1439–1444.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download