Abstract
Purpose
This study was aimed to investigate the clinical and epidemiological characteristics of the patients with acute bronchiolitis who visited in 146 Emergency Departments (EDs) in Korea in 2012.
Methods
We used the NEDIS (National Emergency Department Information System) database to obtain all children with acute bronchiolitis who visited ED under the age of 3 between January 1, 2012 and December 31, 2012.
Results
Totally 18,313 children with acute bronchiolitis were enrolled at this study. The male to female ratio was 1.55:1 and mean age was 10 months. The peak proportion was 17.3% in November during the whole year. The most common chief complaints were fever (38.5%), cough (37.4%), dyspnea (9.5%), gastrointestinal symptom (6.7%), and wheezing (2.5%). The most common accompanying disease was pneumonia (13.3%). The rate of hospital admission and intensive care unit admission were 34.5% and 0.3%, respectively. A predictor for admission via ED was respiratory difficulty.
Figures and Tables
Fig. 1
Number of children brought to an Emergency Department with acute bronchiolitis by age group in 2012.
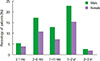
Fig. 2
Monthly distribution of Emergency Department visits for bronchiolitis according to age group in 2012.
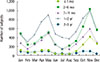
Fig. 3
Chief complains of acute bronchiolits in children at Emergency Department presentation in 2012. GI, gastrointestinal; Sx., symptom; URI, upper respiratory tract infection.

Fig. 4
Admission rate of the ward and ICU in children brought to an Emergency Department with acute bronchiolitis by age group in 2012. ICU, intensive care unit.
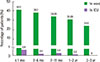
Fig. 5
Monthly trends in the percentage of ward and ICU admission rate of children brought to Emergency Department with acute bronchiolitis in 2012. ICU, intensive care unit.
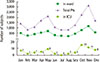
Table 1
Combined disease of acute bronchiolitis who visited Emergency Department in 2012 (n=18,313)

Table 2
Outcomes for children with acute bronchiolitis who visited Emergency Department in 2012

Table 3
Clinical characteristics of intensive care unit admitted children with acute bronchiolitis who visited Emergency Department in 2012

Table 4
Univariate associations between patients features and hospital admission for acute bronchiolitis patients who visited Emergency Department in 2012

References
1. American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics. 2006; 118:1774–1793.
2. Wright RB, Pomerantz WJ, Luria JW. New approaches to respiratory infections in children. Bronchiolitis and croup. Emerg Med Clin North Am. 2002; 20:93–114.

3. Gadomski A. Bronchiolitis dilemma: a happy wheezer and his unhappy parent. Contemp Pediatr. 2002; 19:40–59.
4. Yusuf S, Caviness AC, Adekunle-Ojo AO. Risk factors for admission in children with bronchiolitis from pediatric emergency department observation unit. Pediatr Emerg Care. 2012; 28:1132–1135.

5. Bialy L, Foisy M, Smith M, Fernandes RM. The Cochrane library and the treatment of bronchiolitis in children: an overview of reviews. Evid Based Child Healt. 2011; 6:258–275.

6. Robbins JM, Kotagal UR, Kini NM, Mason WH, Parker JG, Kirschbaum MS. At-home recovery following hospitalization for bronchiolitis. Ambul Pediatr. 2006; 6:8–14.

7. Mulholland EK, Olinsky A, Shann FA. Clinical findings and severity of acute bronchiolitis. Lancet. 1990; 335:1259–1261.

8. Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, Anderson LJ. Bronchiolitis-associated hospitalizations among US children, 1980-1996. JAMA. 1999; 282:1440–1446.

9. Wang EE, Law BJ, Boucher FD, Stephens D, Robinson JL, Dobson S, et al. Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) study of admission and management variation in patients hospitalized with respiratory syncytial viral lower respiratory tract infection. J Pediatr. 1996; 129:390–395.

10. Christakis DA, Cowan CA, Garrison MM, Molteni R, Marcuse E, Zerr DM. Variation in inpatient diagnostic testing and management of bronchiolitis. Pediatrics. 2005; 115:878–884.

11. Kneyber MC, Brandenburg AH, de Groot R, Joosten KF, Rothbarth PH, Ott A, et al. Risk factors for respiratory syncytial virus associated apnoea. Eur J Pediatr. 1998; 157:331–335.

12. Shaw KN, Bell LM, Sherman NH. Outpatient assessment of infants with bronchiolitis. Am J Dis Child. 1991; 145:151–155.

13. Mansbach JM, Emond JA, Camargo CA Jr. Bronchiolitis in US emergency departments 1992 to 2000: epidemiology and practice variation. Pediatr Emerg Care. 2005; 21:242–247.
14. Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr. Temporal trends in emergency department visits for bronchiolitis in the United States, 2006 to 2010. Pediatr Infect Dis J. 2014; 33:11–18.

15. World Health Organization. International classification of disease (ICD-9). Geneva: World Health Organization;1975.
16. Pelletier AJ, Mansbach JM, Camargo CA Jr. Direct medical costs of bronchiolitis hospitalizations in the United States. Pediatrics. 2006; 118:2418–2423.

17. Kim HJ, Jung YM, Park SK, Park HJ, Shin MJ, Kang SC. The statistical observations for pediatric inpatients (1971-1990). J Korean Pediatr Soc. 1993; 36:615–625.
18. Park HY, Lee NY, Lee JS, Jung EH, Lee SJ, Ahn KM, et al. An epidemiological study of acute viral lower respiratory tract infections in hospitalized children from 1996 to 2002 in Seoul, Korea. Pediatr Allergy Respir Dis. 2003; 13:216–226.
19. Kwon JH, Chung YH, Lee NY, Chung EH, Ahn KM, Lee SI. An Epidemiological study of acute viral lower respiratory tract infections in hospitalized children from 2002 to 2006 in Seoul, Korea. Pediatr Allergy Respir Dis. 2008; 18:26–36.
20. Lim JS, Woo SI, Kwon HI, Baek YH, Choi YK, Hahn YS. Clinical characteristics of acute respiratory tract infections due to 13 respiratory viruses detected by multiplex PCR in children. Korean J Pediatr. 2010; 53:373–379.

21. Lee SJ, Shin EW, Park EY, Oh PS, Kim KN, Yoon HS, et al. Epidemiology and clincal analysis of acute viral respiratory tract infections in children (September, 1998-May, 2003). Korean J Pediatr. 2005; 48:266–275.
22. Moon JH, Suh KJ, Chung EH, Shin MY, Lee JS, Park YM, et al. Epidemiology of acute viral lower respiratory tract infection in hospitalized children in two different areas of Korea. Korean J Pediatr Infect Dis. 2002; 9:193–200.

23. Sarnaik AP, Heidemann SM. Respiratory pathophysiology and regulation. In : Kliegman RM, Stanton B, St. Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia: Elsevier Saunders;2011. p. 1419.
24. Lowell DI, Lister G, Von Koss H, McCarthy P. Wheezing in infants: the response to epinephrine. Pediatrics. 1987; 79:939–945.

25. Wang EE, Milner RA, Navas L, Maj H. Observer agreement for respiratory signs and oximetry in infants hospitalized with lower respiratory infections. Am Rev Respir Dis. 1992; 145:106–109.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download