Abstract
Purpose
This study was performed to evaluate the current status of food allergy (FA) and to analyze the relationship between allergy to individual foods and other allergic diseases in elementary school children.
Methods
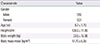
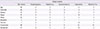
We performed a questionnaire survey for FA, asthma, allergic rhinitis, and atopic dermatitis using International Study of Asthma and Allergies in Childhood questionnaires. A total of 1,929 students in 3 elementary schools were enrolled.
Results
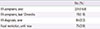
A total of 324 students (16.8%) had ever suffered from FA symptoms more than once. Only 64 out of 324 students (19.8%) were diagnosed with FA by doctors. The presence of soy allergy was associated with the increased risk of bronchial asthma (adjusted odds ratio [aOR], 5.90; 95% confidence interval [CI], 1.87 to 18.59). The presence of egg (aOR, 1.91; 95% CI, 1.04 to 3.52) and wheat allergy (aOR, 5.45; 95% CI, 1.94 to 15.36) were associated with the increased prevalence of allergic rhinitis. The allergic symptoms to fruits/tomato was associated with the increased risk of allergic rhinoconjunctivitis symptoms (aOR, 2.98; 95% CI, 1.18 to 7.47). The allergic symptoms to egg (aOR, 2.29; 95% CI, 1.22 to 4.29), wheat (aOR, 4.91; 95% CI, 1.86 to 12.95), and shrimp/crab (aOR, 2.48; 95% CI, 1.37 to 4.49) were associated with the presence of atopic dermatitis.
Conclusion
The prevalence of FA of elementary school students in Bucheon-city was 16.8%. A significant positive association between the suspected foods and the other allergic diseases was found. Soy allergy was significantly correlated to having bronchial asthma and fruits/tomato allergy correlated with allergic rhinoconjunctivitis.
Figures and Tables
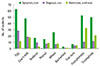
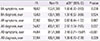
Fig. 1
The number of students with food allergic symptoms, diagnosis, and present restriction for suspected foods.
References
1. Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006; 368:733–743.

2. Lee HB, Shin SA, Oh JW. New patterns of childhood asthma pevalence in six Asian countries: comparison of ISAAC phases I and III. Pediatr Allergy Respir Dis. 2008; 18:70–77.
3. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Pediatr Allergy Respir Dis. 2008; 18:15–25.

4. Hong SJ. Korean ISAAC Study Group of Korean Association of Allergy and Respiratory Diseases: report of Korean ISAAC epidemiologic study for asthma and allergic diseases in children. Pediatr Allergy Respir Dis. 2007; 17:1 Suppl. S55–S66.
5. Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011; 128:e9–e17.

6. Amin AJ, Davis CM. Changes in prevalence and characteristics of IgE-mediated food allergies in children referred to a tertiary care center in 2003 and 2008. Allergy Asthma Proc. 2012; 33:95–101.

7. Bock SA, Munoz-Furlong A, Sampson HA. Further fatalities caused by anaphylactic reactions to food, 2001-2006. J Allergy Clin Immunol. 2007; 119:1016–1018.

8. Oh JW, Pyun BY, Choung JT, Ahn KM, Kim CH, Song SW, et al. Epidemiological change of atopic dermatitis and food allergy in school-aged children in Korea between 1995 and 2000. J Korean Med Sci. 2004; 19:716–723.

9. Seo WH, Jang EY, Han YS, Ahn KM, Jung JT. Management of food allergies in young children at a child care center and hospital in Korean. Pediatr Allergy Respir Dis. 2011; 21:32–38.

10. Chung SJ, Han YS, Chung SW, Ahn KM, Park HY, Lee SI, et al. Marasmus and Kwashiorkor by nutritional ignorance related to vegetarian diet and infants with atopic dermatitis in South Korea. Korean J Nutr. 2004; 37:540–549.
11. Barth GA, Weigl L, Boeing H, Disch R, Borelli S. Food intake of patients with atopic dermatitis. Eur J Dermatol. 2001; 11:199–202.
12. Park SJ, Lee JS, Ahn K, Chung SJ. The comparison of growth and nutrient intakes in children with and without atopic dermatitis. Korean J Community Nutr. 2012; 17:271–279.

13. Sicherer HS, Munoz-Furlong A, Murphy R, Wood RA, Sampson HA. Symposium: pediatric food allergy. Pediatrics. 2003; 111:1591–1594.

15. Zheng T, Yu J, Oh MH, Zhu Z. The atopic march: progression from atopic dermatitis to allergic rhinitis and asthma. Allergy Asthma Immunol Res. 2011; 3:67–73.

16. Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med. 1995; 332:133–138.
17. Klinnert MD, Nelson HS, Price MR, Adinoff AD, Leung DY, Mrazek DA. Onset and persistence of childhood asthma: predictors from infancy. Pediatrics. 2001; 108:E69.

18. Arshad SH, Kurukulaaratchy RJ, Fenn M, Matthews S. Early life risk factors for current wheeze, asthma, and bronchial hyperresponsiveness at 10 years of age. Chest. 2005; 127:502–508.

19. Kusunoki T, Morimoto T, Nishikomori R, Heike T, Fujii T, Nakahata T. Allergic status of schoolchildren with food allergy to eggs, milk or wheat in infancy. Pediatr Allergy Immunol. 2009; 20:642–647.

20. Ministry for Health, Welfare and Family Affairs. Korea Center for Disease Control and Prevention. Korea national health and nutrition examination surveys phase IV (first year, 2007). Cheongwon: 2007 Korea national health statistics:Korea Center for Disease Control and Prevention;2008.
21. Jung YH, Ko H, Kim HY, Seo JH, Kwon JW, Kim BJ, et al. Prevalence and risk factors of food allergy in preschool children in Seoul. Korean J Asthma Allergy Clin Immunol. 2011; 31:177–183.
22. Lee JB, Rha YH, Choi SH. A questionnaire survey of care-givers' understanding of atopic dermatitis. Korean J Asthma Allergy Clin Immunol. 2009; 29:179–185.
23. Bircher AJ, Van Melle G, Haller E, Curty B, Frei PC. IgE to food allergens are highly prevalent in patients allergic to pollens, with and without symptoms of food allergy. Clin Exp Allergy. 1994; 24:367–374.

24. Amlot PL, Kemeny DM, Zachary C, Parkes P, Lessof MH. Oral allergy syndrome (OAS): symptoms of IgE-mediated hypersensitivity to foods. Clin Allergy. 1987; 17:33–42.

25. Fleischer DM, Perry TT, Atkins D, Wood RA, Burks AW, Jones SM, et al. Allergic reactions to foods in preschool-aged children in a prospective observational food allergy study. Pediatrics. 2012; 130:e25–e32.

26. Oh JW. Allergic diseases in childhood and food additives. Pediatr Allergy Respir Dis. 2010; 20:212–218.
27. Simons FE. Anaphylaxis: recent advances in assessment and treatment. J Allergy Clin Immunol. 2009; 124:625–636.

28. Sicherer SH, Mahr T. American Academy of Pediatrics Section on Allergy and Immunology. Management of food allergy in the school setting. Pediatrics. 2010; 126:1232–1239.

29. Eigenmann PA, Sicherer SH, Borkowski TA, Cohen BA, Sampson HA. Prevalence of IgE-mediated food allergy among children with atopic dermatitis. Pediatrics. 1998; 101:E8.

30. Novembre E, de Martino M, Vierucci A. Foods and respiratory allergy. J Allergy Clin Immunol. 1988; 81(5 Pt 2):1059–1065.

31. Yu J. Allergic March: progression from atopic dermatitis to asthma. Korean J Asthma Allergy Clin Immunol. 2012; 32:137–143.
32. Ahn K. Food allergy: diagnosis and management. Korean J Asthma Allergy Clin Immunol. 2011; 31:163–169.
33. Huang SW. Follow-up of children with rhinitis and cough associated with milk allergy. Pediatr Allergy Immunol. 2007; 18:81–85.

34. Sahin-Yilmaz A, Nocon CC, Corey JP. Immunoglobulin E-mediated food allergies among adults with allergic rhinitis. Otolaryngol Head Neck Surg. 2010; 143:379–385.

35. Tan TN, Lim DL, Lee BW, Van Bever HP. Prevalence of allergy-related symptoms in Singaporean children in the second year of life. Pediatr Allergy Immunol. 2005; 16:151–156.

36. Sicherer SH. Is food allergy causing your patient's asthma symptoms? J Respir Dis. 2000; 21:127–136.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download