Abstract
Purpose
Atopic dermatitis (AD) is an inflammatory skin disease, significantly affecting the quality of life. Using AD as a model system, we tested a successive identification of AD-associated microbes, followed by a culture-independent serum detection of the identified microbe.
Methods
A total of 43 genomic DNA preparations from washing fluid of the cubital fossa of 6 healthy controls, skin lesions of 27 AD patients, 10 of which later received treatment (post-treatment), were subjected to high-throughput pyrosequencing on a Roche 454 GS-FLX platform.
Results
Microbial diversity was decreased in AD, and was restored following treatment. AD was characterized by the domination of Staphylococcus, Pseudomonas, and Streptococcus, whereas Alcaligenaceae (f), Sediminibacterium, and Lactococcus were characteristic of healthy skin. An enzyme-linked immunosorbent assay (ELISA) showed that serum could be used as a source for the detection of Staphylococcus aureus extracellular vesicles (EVs). S. aureus EV-specific immunoglobulin G (IgG) and immunoglobulin E (IgE) were quantified in the serum.
Atopic dermatitis (AD) is a recurrent, chronic inflammatory skin disease which is characterized by itching and xerosis, and is closely associated with immunoglobulin E (IgE)-mediated sensitization to allergens.12 Skin barrier dysfunction, allergic or microbial skin colonization, and decreased innate immune responses are considered significant causes for AD.34 The prevalence of AD is increasing in developed countries, with incidence rates reaching up to 30% in children and up to 10% in adults.567 The skin microbiome has also been implicated in the pathogenesis of AD. For example, a localized pathogen and a constituent of general skin microbiota, Staphylococcus aureus (S. aureus) were shown to be involved in the local skin inflammation,189 and its exotoxin acted as a superantigen that induced T-cell and IgE responses.11011 The lack of studies concerning the skin microbiome has precluded a deep understanding of the effect of skin bacteria.
Traditional 16S ribosomal RNA (rRNA) gene sequence analysis has recently expanded into a metagenomic analysis, where a massively parallel high-throughput next-generation DNA sequencing of variable (V) regions of bacterial gene coding for 16S rRNA, a 16S metagenomic sequencing, can potentially identify and classify an unprecedented number of skin microbiota in a culture-independent manner.12 The introduction of metagenomics also provided key information about the types of microbes and the composition of microbiota on normal healthy skin. For example, whereas healthy saliva shows high alpha diversity and low beta diversity, the antecubital fossa region of the skin has high beta diversity and intermediate level of alpha diversity, implicating that the microbiome composition of normal subjects' skin shows one of the highest level of variations among individuals.13
The microbiome study regarding AD has always been of great interest, since a large portion of child population is susceptible to this disease caused by physical pain and emotional stress. Of the cultivatable microorganisms, S. aureus has been consistently reported to be associated with AD, including a report that confirmed that severe AD showed a positive correlation with reduced skin bacterial diversity and that Staphylococcus was the most dominant bacterium found in the antecubital crease, contributing to the reduction of microbial diversity in AD and to the positive partial correlation to disease severity.10
Extracelluar vesicles (EVs) are nanometer-sized membrane vesicles derived from prokaryotes, archaea, and eukaryotes, and function not only intercellular signaling mediators using enclosed proteins, nucleic acids, and lipids but also as a source of novel biomarkers in the diagnosis and prognosis of disease.1415 Most importantly, EVs can be purified from body fluids, including plasma and urine, thereby providing an excellent tool to probe the effect of bacterial infection on a systemic level.16 We also previously reported that S. aureus-derived EVs induced AD-like inflammation in the skin and were causally related to the pathogenesis of AD.1718
Here, we analyzed the bacterial communities in skin washing fluid from AD patients and normal controls by 16S metagenomic sequencing to define the microbial composition contributing to AD and to evaluate its changes following eczema treatment. Furthermore, we tested systemic bacterial presence through detecting S. aureus-derived EVs in AD patients using an enzyme-linked immunosorbent assay (ELISA)-based method to probe the relationship between the presence of S. aureus in the skin and the EV-specific immunoglobulin G (IgG) in the serum of AD patients.
This study was approved by the ethics committee of Soonchunhyang University Hospital (approval number 2013-061) and was composed of 6 normal controls and 27 AD patients. Of the 27 AD patients, 10 were provided with skin washing fluid before and after AD treatment. Therefore, total of 43 metagenomic sequencing data were generated from 33 study subjects. Patients with aggravated AD according to the Hanifin and Rajka AD diagnostic criteria19 were enrolled at the Pediatric Allergy and Respiratory Center of Soonchunhyang University Hospital. Informed consent forms were obtained from the participants and their parents. Patients who had other skin diseases or had received topical/oral/injectable antibiotics within the previous 14 days were excluded. Normal control subjects consisted of children who had no previous skin diseases, including AD, or any other allergic or significant underlying diseases, and had no medication history. AD treatment included wet dressing and treatment with topical corticosteroids, antihistamines, and antibiotics.
Saline-soaked gauzes were placed on the skin lesions, mainly the cubital fossae of AD patients, before and after treatment for 10-15 minutes. The retrieved gauzes were stored in containers filled with saline solution. For the control group, saline-soaked gauzes were placed on the cubital fossa and were processed in the same way.
White blood cells, eosinophil count, total IgE, and eosinophil cationic protein (ECP) were measured in AD patients. Laboratory tests were not performed in normal controls. AD severity was measured by the SCORing Atopic Dermatitis (SCORAD) index.20
Bacterial DNAs were purified from skin washing fluid using PowerWater® DNA Isolation Kit (MO BIO Laboratories, Carlsbad, CA, USA). Libraries were prepared according to the Rapid Library Preparation Method Manual for GS FLX plus series (Roche, Branford, CT, USA). Libraries were quantified using Quant-iT PicoGreen dsDNA Assay Kit (Thermo Fisher Scientific, Waltham, MA, USA). The emPCR, corresponding to clonal amplifications of the purified libraries, was carried out using the GS-FLX plus emPCR Kit (Roche). Briefly, libraries were immobilized onto DNA capture beads, added to a mixture of amplification mix and oil, and were vigorously shaken on a TissueLyser II (Qiagen, Valencia, CA, USA) to create “micro-reactors” containing both amplification mix and a single bead. Emulsion was dispensed into a 96-well plate and the PCR amplification program was run according to the manufacturer's recommendation. Then, 20 ng aliquot of each sample DNA was used for a 50 µL PCR reaction. Universal primers 27F (5′-GAGTTTGATCMTGGCTCAG-3′), 518R (5′-WTTACCGCGGCTGCTGG-3′) were used for the amplification of variable regions 1 through 3 (V1–V3) of bacterial 16S rRNA genes. The FastStart™ High Fidelity PCR System (Roche) was used for the following PCR conditions: 94℃ for 3 minutes followed by 35 cycles of 94℃ for 15 seconds, 55℃ for 45 seconds, and 72℃ for 1 minute, followed by a final elongation step at 72℃ for 8 minutes. The PCR products were purified using Agencourt AMPure XP system (Beckman Coulter Inc., Brea, CA, USA).
Sequencing was performed on a Genome Sequencer FLX plus System (Roche) at Macrogen (Seoul, Korea). Following PCR amplification, the emulsion was chemically broken, and the beads carrying the amplified DNA libraries were recovered and washed by filtration. Positive beads were purified using the biotinylated primer A (complementary to adaptor A), which binds to streptavidin-coated magnetic beads. The DNA library beads were separated from the magnetic beads by melting the double-stranded amplification products. The sequencing primer was then annealed to the amplified single-stranded DNA. Finally, beads carrying amplified single-stranded DNA were counted with a Particle Counter (Beckman Coulter Inc.). Each sample was loaded in 1 region of a 70-75 mm PicoTiter plate (Roche) fitted with an 8-lane gasket.
Analysis and interpretation of NGS data were carried out at MD Healthcare (Seoul, Korea). The high-quality sequencing reads were selected after checking the read length (≥300 bp) and the quality score (average Phred score ≥20). Operational Taxonomy Units (OTUs) were clustered by using sequence clustering algorithms UCLUST.21 Subsequently, taxonomy assignment against the 16sRNA sequence database in GreenGenes 8.15.13 was carried out by using QIIME.22 Based on the sequence similarities, all 16sRNA sequences were assigned to the following taxonomic levels: species (s), ≥97% similarity; genus (g),
≥94% similarity; family (f), ≥90% similarity; order (o), ≥85% similarity; class (c), ≥80% similarity; and phylum (p), ≥75% similarity. The bacterial composition at the genus level was plotted in the heatmap if a genus cluster shows significantly different composition between 2 groups (≥2-fold change in composition between the AD and control groups). In case clusters could not be assigned at the genus level due to the lack of sequences or redundant sequences in the database, the taxon was assigned at the higher level, which is indicated in the parenthesis.
For the measurement of specific IgG and IgE levels, 1.25 µg of S. aureus exotoxin B and 100 ng of S. aureus EV were coated on a polystyrene plate (Corning Inc., Corning, NY, USA), respectively. After overnight incubation, bovine serum albumin (1% weight per volume in phosphate-buffered saline [PBS]) was used to block non-specific bindings for 1 hour at room temperature prior to the addition of a 1:1,000 dilution of serum. Horseradish peroxidase-conjugated secondary antibody was added and incubated for 1 hour, and the absorbance was measured in a VersaMax™ ELISA Microplate Reader (Molecular Devices, Sunnyvale, CA, USA). IgG and IgE levels were measured using human IgG and IgE ELISA kits (Bethyl Laboratories, Montgomery, TX, USA for each), according to the manufacturer's instructions.
Thirty-three subjects were enrolled, including 27 AD patients and 6 normal controls. The mean age of the AD patients and controls was 91 and 83 months, respectively. Eighteen AD patients and 4 normal controls were male (both 66.7%). Mean eosinophil count and ECP level were 877 per µL and 66.4 µg/µL, respectively, in the peripheral blood of patients. Of the 26 AD patients who were positive for IgE response to allergens, 17 were IgE-positive specifically for house dust mites. Mean SCORAD index was significantly decreased from 72.5±19.9 before treatment to 41.4±16.2 after treatment (P<0.001) among patients, implicating the effectiveness of used treatment (Table 1). Microbial 16S rRNA gene (V1-V3 regions)-based metagenomic sequencing was performed on 6 controls and 27 patients, of which 10 were further subjected to metagenome analysis following AD treatment (materials and methods).
A total of 18 bacterial genera showed differential compositions (≥2-fold change) between AD patients and normal controls from a metagenomic analysis of skin washing fluid (Fig. 1). In AD patients, Staphylococcus accounted for the highest proportion of microorganisms at 66.2%, followed by Pseudomonas (11.6%), Streptococcus (6.19%), and Acinetobacter (1.21%). Each of the genera Lactobacillus, Xanthomonadaceae (f), Leuconostoc, Alcaligenaceae (f), Lactococcus, Rhizobiales (o), and Methylobacterium accounted for more than 1% of microbial compositions. On the other hand, the most dominant microorganism in the skin of normal controls was Alcaligenaceae (f) at 40.4%, which was a drastic increase from 0.03% in AD patients. The next highest proportions of normal microbiota were Sediminibacterium (13.2%) and Lactococcus (3.9%), whose proportions were drastically decreased to 0% and 0.3%, respectively in AD patients. Overall, for the bacterial genera that showed differential compositions between the 2 groups, normal skin washing fluid showed 18 bacterial types with varying compositions from 0.22% for Staphylococcus (f) to 40.36% for Alcaligenaceae (f), whereas skin washing fluids from AD patients showed only 11 detectable microbial compositions, showing greatly decreased microbial diversity.
Staphylococcaceae, Pseudomonadaceae and Streptococcaceae (f), Bacillales and Pseudomonadales (o), Bacilli (c), and Firmicutes (p) were the dominant microarganims in AD patients. On the contrary, Alcaligenaceae (f), Burkholderiales (o), Betaproteobacteria (c), and Proteobacteria (p) composed the major bacteria in the washing fluid of normal controls (Supplementary Fig. 1). At the genus level, the major composition of Staphylococcus was followed by Pseudomonas and Streptococcus in AD patients, whereas Alcaligenaceae and Sediminibacterium were more frequent in controls (Supplementary Fig. 2).
Further analysis confirmed the major Staphylococcus species as S. aureus, in AD patients, with relatively minor prevalence of S. haemolyticus and S. epidermidis (Supplementary Fig. 3).
Treatment of AD patients with wet dressing or other anti-inflammatory drugs (materials and methods) brought into alleviation of symptoms together with changes in bacterial compositions. The proportion of Staphylococcus significantly decreased from 38.8% to 5.7% of the total microbiota following treatment. At the same time, increasing proportions were observed for Alicyclobacillus (2.21% to 6.03%), Propionibacterium (2.24% to 4.62%), and Streptococcus (0.47% to 6.47%, Fig. 2). At a phylum level, Firmicutes and Actinobacteria showed opposite pattern in composition, with Fumicutes being decreased and Actinobacteria showing increase in composition following treatment (Fig. 3). Microorganisms that belonged to the class of Bacilli (c), Bacillales (o) and Staphylococcaceae (f) dominated before treatment and decreased after treatment, whereas Propionibacteriales (o), Lactobacillales (o), Alicyclobacillaceae, Propionibacteriaceae, and Streptococcaceae (f) increased after treatment. At the genus level, Staphylococcus was reduced, while Alicyclobacillus, Propionibacterium, and Streptococcus were increased, and bacterial diversity was restored after treatment compared to before treatment (Fig. 4).
Previous results showed that AD patients had lower microbial diversity as measured by the Shannon-Weiner index and also by Simpson index.21 We tested if changes in microbial diversity can be observed among normal subjects, AD patients, and patients who received eczema treatment (Table 2). The Shanon index was significantly lower in AD patients (2.4±1.6) than in normal controls (4.8±1.2). A subpopulation of patients who received treatment showed recovery in microbiota diversity as shown with an increase in the Shanon index from 3.2±1.2 to 5.4±1.7 (Table 3).
We previously showed that there was a causal relationship between S. aureus-derived EV and the pathogenesis of AD,17 and there was also a report showing that S. aureus was the major bacterium found in the skin of AD patients.9 Therefore, we tested if the S. aureus-derived EVs could be detected in the serum through measuring EV-specific IgE in the serum, also using S. aureus exotoxin B as a positive experimental control.
The levels of exotoxin-specific IgG and IgE were significantly higher in AD patients: 65.9±66.0 µg/mL for IgG and 1.2±0.3µg/mL for IgE in controls and 220.8±188.5 µg/mL for IgG and 3.4±4.6 µg/mL for IgE in AD patients (P=0.008 and P=0.047, respectively). EV-specific IgG and IgE levels were also significantly higher in AD patients: 21.7±48.4 µg/mL for IgG and 3.1±0.5 µg/mL for IgE in controls and 144.4±93.3 µg/mL for IgG and 6.9±3.9 µg/mL for IgE in AD patients (P=0.001) (Fig. 5). These results confirm that serum can be used to detect the presence of S. aureus, the most dominant microorganism associated with AD.
Microorganisms contribute to diverse human pathogeneses, not by their presence, but by their imbalance in the composition of microbiota. In contrast to the conventional culture-based assays, metagenome analysis makes it possible to identify and count relative abundance of all species present.12 In this report, we compared the bacterial compositions between normal subjects and AD patients, and also between pre- and post-treatment groups of AD patients.
The most dominant microorganisms in the skin of normal control were Alcaligenaceae (f) (40.4%), followed by Sediminibacterium (13.2%) and Lactococcus (3.9%). However, in AD patients, the proportion of Alcaligenaceae (f) was drastically reduced to 0.03% and Lactococcus and Sediminibacterium were also reduced to less than 1%. On the contrary, we showed that Staphylococcus became the most dominant bacteria in AD patients at 66.2%, which was in accordance with the results of a previous report.5 Higher compositions of other bacteria in AD patients, including Pseudomonas (11.6%) and Streptococcus (6.19%) were also observed. Therefore, 2 different microbial signatures represented the 2 states of normal controls and AD patients. Drago et al.23 also reported that Firmicutes and Staphylococcaceae were the most abundant phylum and family, respectively, and S. aureus accounted 73% of total staphylococci load in the skin of AD patients. However, unlike our study, they failed to show the different microbial composition between AD patients and normal controls except higher frequency of S. aureus. Seite et al.24 also revealed that Staphylococcus, Propionibacterium, and Streptococcus were abundant in the lesional skin of AD patients. In contrast, S. epidermidis was the most common among the Staphylococcus species.
The increased prevalence of Streptococcus, Propionibacterium, and Corynebacterium after AD treatment was reported earlier.10 In our study, Alicyclobacillus, Propionibacterium, and Streptococcus were increased after treatment.
Changes in microbial compositions between normal controls and AD patients were also illustrated by decreased microbial diversity. Recovery of the bacterial diversity after AD treatment was also observed. In this case, Alicyclobacillus (from 2.21% to 6.03% post-treatment), Propionibacterium (2.24% to 4.62%), and Streptococcus (0.47% to 6.47%) were all increased after AD treatment, which was also in line with the result of a previous report,10 where the increases in the microbial compositions of Streptococcus, Propionibacterium, and Corynebacterium after eczema treatment were documented. However, the bacterial composition of patients following treatment was not identical with that of normal controls, implying that the AD treatment causes increased diversity, but the treatment does not necessarily restore the microbial composition to the original state of normal controls. AD patients are vulnerable to S. aureus infection and colonization. S. aureus colonization occurs in 90% of AD patients but in only 10% of normal subjects.19 In the current study, we showed that Staphylococcus was dominant in skin washing fluid from AD patients compared with normal controls. In AD patients, the dominance of Staphylococcus was significantly reduced following treatment, contributing to the greater microbial diversity. This may suggest that the decreased microbial diversity due to the dominance of Staphylococcus is one of the major factors that represent AD. Even though it is not known whether the increase in Propionibacterium and Corynebacterium is the result of the decrease in Staphylococcus and vice versa, the combined decrease in S. aureus and increases in Streptococcus, Propionibacterium, and Corynebacterium might be utilized as an indicator of recovery from deterioration of AD.
Bacterial membrane vesicles with active biomolecules are extracellularly released into human biofluids and can function as carriers of signaling molecules between microorganisms and host cells or among themselves.25 These EVs also provide excellent sources for a non-invasive diagnosis of diseases associated with the presence of microorganisms, since they are readily recovered from blood, urine, and other biofluids.26 Previous results revealed that S. aureus-derived EVs induced skin barrier disruption and cause AD-like skin inflammation.17 This is consistent with an ELISA performed in this study, in which EV-specific IgG and IgE increased 2-fold in AD patients compared with normal controls. We showed compositional changes in patients with AD and its treatment by high throughput 16S rRNA metagenomic analysis and also showed that the most dominant S. aureus in AD can be detected by the presence of its EV in patients' serum.
Since EVs are produced from all forms of life and present in diverse body fluids, such as plasma, serum, saliva, urine, breast milk, and ascites,27 the combined approach of metagenomic sequencing analyses of patients' body fluids and EV-based microbe detection provide a novel approach for a quick and efficient diagnossisof human diseases.
Figures and Tables
Fig. 1
Comparison of bacterial composition in the skin washing fluid of AD patients (case) and normal controls. (A, B) In the skin washing fluid of patients, Staphylococcus accounted for the majority of bacteria, followed by Pseudomonas and Streptococcus in the heatmap. In normal controls, Staphylococcus, Pseudomonas, and Streptococcus were hardly detected, whereas Sediminibacterium, Alcaligenaceae (f) were predominant. AD, atopic dermatitis; f, family.

Fig. 2
Changes in the bacterial proportion of skin washing fluid in patients with AD before and after treatment. (A, B) The proportion of Staphylococcus decreased after treatment. Increasing proportions following treatment were evident for Alicyclobacillus, Propionibacterium, and Streptococcus. AD, atopic dermatitis.

Fig. 3
Bacterial community analysis of skin washing fluid of AD patients with before and after treatment according to the phylogenetic hierarchy of phylum, class, order, and family. (A) In AD patients, Firmicutes was dominant before treatment and decreased following treatment, with Actinobacteria being increased after treatment. (B) Bacilli dominated before treatment and decreased after treatment, with Actinobacteria being increased after treatment at the class level. (C) Bacillales were dominant before treatment and decreased after treatment, with Propionibacteriales and Lactobacillales being increased after treatment at the order level. (D) Staphylococcaceae was dominant before treatment and was decreased after treatment, with Alicyclobacillaceae, Propionibacteriaceae and Streptococcaceae increased after treatment at the family level. AD, atopic dermatitis.

Fig. 4
Bacterial community analysis of skin washing fluid of AD patients with before and after treatment in the genus level. (A, B) Staphylococcus was reduced, while Alicyclobacillus, Propionibacterium, and Streptococcus were increased and bacterial diversity was restored after treatment compared to that before treatment. AD, atopic dermatitis.

Fig. 5
SEB-specific IgG and IgE and S. aureus EV-specific IgG and IgE levels. (A, B) SEB-specific IgG and IgE levels were significantly higher in the serum of AD patients compared with that of normal controls. (C, D) S. aureus EV-specific IgG and IgE levels were significantly higher in the serum of AD patients compared with those of normal controls. SEB, S. aureus exotoxin B; IgG, immunoglobulin G; IgE, immunoglobulin E; EV, extracellular vesicle; AD, atopic dermatitis.

Table 1
Clinical characteristics of the AD patients and normal controls
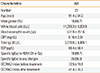
Table 2
Microbial diversities in AD patients and normal controls
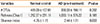
| Variables | Normal control | AD (pre-treatment) | P value |
|---|---|---|---|
| # OTUs | 419.00±107.81 | 330.33±156.11 | 0.202 |
| Richness (Chao1) | 1,252.37±231.11 | 1,033.11±375.22 | 0.185 |
| Shannon index | 4.75±1.15 | 2.44±1.61 | 0.003 |
ACKNOWLEDGMENTS
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI13C0040 and HI14C2628). Also, this work was supported by the National Research Foundation of Korea grant funded by the Ministry of Education, Science & Technology (NRF-2010-0028684, NRF-2014-R1A1A1005144) and the Soonchunhyang University Research Fund.
References
1. Sabin BR, Peters N, Peters AT. Chapter 20: atopic dermatitis. Allergy Asthma Proc. 2012; 33:Suppl 1. S67–S69.
2. Lee JH, Son SW, Cho SH. A comprehensive review of the treatment of atopic eczema. Allergy Asthma Immunol Res. 2016; 8:181–190.
3. Leung DY, Boguniewicz M, Howell MD, Nomura I, Hamid QA. New insights into atopic dermatitis. J Clin Invest. 2004; 113:651–657.
4. Pyun BY. Natural history and risk factors of atopic dermatitis in children. Allergy Asthma Immunol Res. 2015; 7:101–105.
5. Bieber T. Atopic dermatitis. N Engl J Med. 2008; 358:1483–1494.
6. Ahn K. The prevalence of atopic dermatitis in Korean children. Allergy Asthma Immunol Res. 2016; 8:1–2.
7. Lee JH, Han KD, Kim KM, Park YG, Lee JY, Park YM. Prevalence of atopic dermatitis in Korean children based on data from the 2008–2011 Korean National Health and Nutrition Examination Survey. Allergy Asthma Immunol Res. 2016; 8:79–83.
8. Niebuhr M, Langnickel J, Draing C, Renz H, Kapp A, Werfel T. Dysregulation of toll-like receptor-2 (TLR-2)-induced effects in monocytes from patients with atopic dermatitis: impact of the TLR-2 R753Q polymorphism. Allergy. 2008; 63:728–734.
9. Wollenberg A, Feichtner K. Atopic dermatitis and skin allergies - update and outlook. Allergy. 2013; 68:1509–1519.
10. Kong HH, Oh J, Deming C, Conlan S, Grice EA, Beatson MA, et al. Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res. 2012; 22:850–859.
11. Breuer K, Wittmann M, Bösche B, Kapp A, Werfel T. Severe atopic dermatitis is associated with sensitization to staphylococcal enterotoxin B (SEB). Allergy. 2000; 55:551–555.
12. Chen YE, Tsao H. The skin microbiome: current perspectives and future challenges. J Am Acad Dermatol. 2013; 69:143–155.
13. Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012; 486:207–214.
14. EL Andaloussi S, Mäger I, Breakefield XO, Wood MJ. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov. 2013; 12:347–357.
15. Pyun BY. Extracellular vesicle: an unknown environmental factor for causing airway disease. Allergy Asthma Immunol Res. 2016; 8:179–180.
16. Shin TS, Kim JH, Kim YS, Jeon SG, Zhu Z, Gho YS, et al. Extracellular vesicles are key intercellular mediators in the development of immune dysfunction to allergens in the airways. Allergy. 2010; 65:1256–1265.
17. Hong SW, Kim MR, Lee EY, Kim JH, Kim YS, Jeon SG, et al. Extracellular vesicles derived from Staphylococcus aureus induce atopic dermatitis-like skin inflammation. Allergy. 2011; 66:351–359.
18. Hong SW, Choi EB, Min TK, Kim JH, Kim MH, Jeon SG, et al. An important role of α-hemolysin in extracellular vesicles on the development of atopic dermatitis induced by Staphylococcus aureus. PLoS One. 2014; 9:e100499.
19. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh). 1980; 92:44–47.
20. Severity scoring of atopic dermatitis: the SCORAD index. Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology. 1993; 186:23–31.
21. Edgar RC. Search and clustering orders of magnitude faster than BLAST. Bioinformatics. 2010; 26:2460–2461.
22. Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010; 7:335–336.
23. Drago L, De Grandi R, Altomare G, Pigatto P, Rossi O, Toscano M. Skin microbiota of first cousins affected by psoriasis and atopic dermatitis. Clin Mol Allergy. 2016; 14:2.
24. Seite S, Flores GE, Henley JB, Martin R, Zelenkova H, Aguilar L, et al. Microbiome of affected and unaffected skin of patients with atopic dermatitis before and after emollient treatment. J Drugs Dermatol. 2014; 13:1365–1372.
25. Choi Y, Park H, Park HS, Kim YK. Extracellular vesicles, a key mediator to link environmental microbiota to airway immunity. Allergy Asthma Immunol Res. 2017; 9:101–106.
26. Kim JH, Lee J, Park J, Gho YS. Gram-negative and gram-positive bacterial extracellular vesicles. Semin Cell Dev Biol. 2015; 40:97–104.
27. Campos JH, Soares RP, Ribeiro K, Andrade AC, Batista WL, Torrecilhas AC. Extracellular vesicles: role in inflammatory responses and potential uses in vaccination in cancer and infectious diseases. J Immunol Res. 2015; 2015:832057.
SUPPLEMENTARY MATERIALS
Supplementary Fig. 1
Bacterial community analysis of skin washing fluid of AD patients and normal controls according to the phylogenetic hierarchy of phylum, class, order, and family. (A) Firmicutes were dominant and Proteobacteria were minor in AD patients. Conversely, in control participants, Proteobacteria were dominant, with minor contributions from Firmicutes or Bacteroidetes and relative bacterial diversity was maintained. (B) At the class level, Bacilli were dominant in AD patients, whareas Betaproteobacteria predominated in controls. (C) At the order level, Bacillales were dominant in AD patients, whereas Burkholderiales were dominant in the controls. (D) At the family level, Staphylococcaceae were dominant in composition, followed by Pseudomonadaceae and Streptococcaceae in AD patients, whereas Alcaligenaceae were predominant in controls. AD, atopic dermatitis.
Supplementary Fig. 2
An analysis of bacterial community in the skin washing fluid of AD patients and normal controls at a genus level. (A, B) Staphylococcus predominated and was followed by Pseudomonas and Streptococcus in AD patients. Alcaligenaceae and Sediminibacterium were more frequent in controls. AD, atopic dermatitis.
Supplementary Fig. 3
Species analysis of Staphylococcus genus. (A) Most of the Staphylococcal genus in AD patients were S. aureus, with a minority being S. haemolyticus and S. epidermidis. (B) Identification of OTU7176 as Staphylococcus aureus. (C) Identification of OTU2247 as Staphylococcus haemolyticus. (D) Identification of OTU6527 as Staphylococcus epidermidis. AD, atopic dermatitis; OTU, Operational Taxonomy Unit.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download