Abstract
Purpose
This study was conducted to evaluate the association between AR and mental health status in the general Korean adult population and to investigate the relative burden of AR on mental health using the Allergic Rhinitis and Its Impact on Asthma (ARIA) classification.
Methods
A cross-sectional study was performed by using data from 11,154 individuals, 19 years old or older in the Korean National Health and Nutrition Examination Survey 2011-2012. Univariate analysis was conducted in the healthy AR groups with weighted prevalence of demographic characteristics, socioeconomic status, and comorbid diseases. Subanalysis that classified AR severity according to the ARIA classification was carried out to evaluate the relationship of AR severity with mental health. The odds ratios (ORs) for each component representing mental health status were estimated by multiple logistic regression analysis with confounder adjustment.
Results
Univariate analysis with the chi-square test after adjustment for age, sex, body mass index, smoking status, alcohol use status, and exercise status, components representing mental health status showed a linear relationship with the severity of AR according to the ARIA classification. Stress, depressive mood, suicidal thoughts, and psychological consultation factors were correlated with AR after adjustment for demographic characteristics and socioeconomic status. Even after adjustment for comorbid allergic diseases, the correlation remained significant with stress, depressive mood, and psychological consultation factors (OR [95% CI]; 1.227 [1.042, 1.445], 1.368 [1.095, 1.71], 1.804 [1.096, 2.969], respectively).
Conclusions
Patients with AR appear to be at higher risk of mental disorders in the general Korean adult population. Moreover, persistent or severe AR was correlated with poor mental health. Therefore, better control of AR may be conducive to better mental health, and more attention should be paid to the psychological status of AR patients.
Allergic rhinitis (AR) is one of the most common chronic diseases and impairs sufferers' quality of life, sleep, and work performance.1 The incidence of AR was 12% in the European Community Respiratory Health Survey Worldwide.2 The prevalence of allergies was 23.5% of the general US population in the NHANES 2005-2006,3 and in an Asia-Pacific Survey the AR prevalence ranged from 2.5% to 13.2%.4 Over the last decade, an increasing prevalence of AR has become a worldwide trend,56 including Korea.7 AR is associated with physical, emotional, social impairments and difficulties at work or school.89101112 There are several reports describing the association between allergies and depressive disorder/anxiety/sleep disturbance/suicide risk.131415 From 2006 through 2010, the suicide rate in Korea has increased from 21.8 per 100,000 to 31.2 per 100,000, which is the highest among the Organization for Economic Cooperation and Development countries in 2011.16 The increasing prevalence of AR and growing concern about mental health should be regarded as serious public health issues in Korea. There have been no studies reporting association between AR and mental health in the Korea population.
We therefore assessed the relationship between AR and mental health using the Fifth Korean National Health and Nutrition Examination Survey (KNHANES), including subanalysis according to the Allergic Rhinitis and Its Impact on Asthma (ARIA) criteria.
KNHANES V (2011-2012) was a nationwide non-institutionalized civilian population-based survey in South Korea. The protocol was approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention (2011-02CON-06-C, 2012-01EXP-01-2C), and all individuals signed informed consent forms. Stratified multistage cluster random sampling designed by the rolling-survey sampling method was used in the survey.17 Therefore, the rolling samples collected are the probabilities that represent the Korean general population, which are independent of and homogeneous to each other. In 2011-2012, weighted 15,308 individuals participated in the otorhinolaryngologic surveys. Among the 15,308 participants, we excluded the following participants: those younger than 19 years (n=3,717) and those who did not completely answer questions about rhinitis symptoms, mental health, sociodemographic factors, and comorbid diseases (n=1,705). Thus, the final total number of weighted participants (n=11,154; unweighted n=23,893,740) was eligible for our study (Fig. 1).
The questionnaires were administered face to face by the physicians or interviewers. Age was clustered into 7 subgroups by 10-year periods. Body mass index (BMI) was calculated by dividing body weight in kilograms by the square of height in meters. BMI and sleep time were compared by using mean values. Current cigarette smokers were categorized as "yes" for participants who had smoked more than 100 cigarettes during their lifetime and current smoking state. The amount of pure alcohol consumed (in grams per day) was estimated by the average quantity of alcoholic beverages consumed and the frequency of alcohol consumption. Participants who drank more than 30 g/day were categorized as heavy drinkers.18 Participants who commit to moderate physical activity at least 5 days per week for more than 30 minutes each day and/or strenuous physical activity for more than 20 minutes per session at least 3 days per week were classified as the regular exercise group.19 Residency was categorized into urban and rural areas according to the official address of the subjects. The category of 'low income' corresponded to the lowest quartile of annual household income. The education level of the subject was classified as high if the participant finished education beyond middle school (higher than the ninth grade). Marital status was divided into single or married.
Since prevalence based on symptoms alone may represent an overestimation,20 the self-report rhinitis measure used in our study can be considered to be physician-diagnosed AR. The following question was used to assess physician-diagnosed AR for each participant: "Have you been diagnosed with AR by a doctor?"19 Physician-diagnosed depression was also determined by using similar questions: "Have you been diagnosed with depression by a doctor?" Stress levels assessed by the questionnaire were categorized into low (none or small amount) or high (some or extreme). A separate set of questionnaires assessed participants for the presence of depressive symptoms and suicidal thoughts. We asked about depressive symptoms: "During the past year, have you felt feelings of sadness or hopelessness that persisted for at least 2 weeks and that disrupted your social life?" (yes/no). For suicidal thoughts, participants were asked, "During the past year, have you ever felt that you were willing to die?" (yes/no). For psychological consultation, "During the past year, have you ever received any consultation through interview, telephone, or online because of psychological problems" (yes/no). We also used the EuroQol 5-Dimension (EQ-5D) that has been widely used for the measurement of general health-related quality of life. The EQ-5D records the level of self-reported problems evaluated in 5 dimensions (i.e., mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). For each dimension, participants chose 1 of the 3 levels of severity (1, no problem; 2, some/moderate problems; 3, severe/extreme problems). We used the anxiety/depression dimension of the EQ-5D to evaluate mental health.
Statistical analyses were performed by using Statistical Analysis Software (SAS) version 9.3 (SAS Institute, Cary, NC, USA). To calculate unbiased national estimates representing the general Korean population, we used KNHANES sample weights accounting for the complex sampling design to each participant.21 We measured the mean±SE or the proportion (SE). For the differences between general characteristics of AR and healthy participants, continuous variables were tested with the t test using the SURVEYREG procedure, while categorical variables were tested with the Rao-Scott chi-square test using the SURVEYFREQ procedure. The weighted prevalence of AR was calculated in the Korean population after adjustment for strata and after clustering at the primary sampling unit level. Using multiple logistic regression analysis with the SURVEYLOGISTIC procedure, we tested the correlation between AR and mental health after adjustment for confounding factors. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated after adjustment for potential confounders. Adjusted confounding factors were age, sex, BMI, smoking status, alcohol use status, and exercise status (model 1); age, sex, BMI, smoking status, alcohol use status, exercise status, region of residence, income, education, and marital status (model 2); and age, sex, BMI, smoking status, alcohol use status, exercise status, region of residence, income, education, marital status, asthma, and atopic dermatitis (model 3). A P value of <0.05 was considered statistically significant.
A total of weighted 11,154 participants (unweighted n= 23,893,740) were included in the study, and the general characteristics of this study population are presented in Table 1. Of these 11,154 participants, 1,467 (unweighted n=3,518,737) were diagnosed with AR. In univariate analysis, the significantly higher AR prevalence was found in demographic characteristics, socioeconomic status, and comorbid diseases, including age (P<0.0001), sex (P<0.001), BMI (P<0.0001), sleep (P<0.0001), current cigarette smoker (P=0.00001), urban residency (P=0.0144), high education level (P<0.0001), low income (P<0.0001), married state (P<0.0001), asthma (P<0.0001), and atopic dermatitis (P<0.0001). Thus, demographic characteristics, socioeconomic status, and comorbid diseases had the possibility of acting as potential confounders.
Among components explaining mental health, AR prevalence was high only in stress component (P<0.001). This result could be explained by the age factor. Fig. 2 shows the prevalence of AR and mental health characteristics stratified by age among the KNHANES (2011-2012) population aged ≥19 years. As age increased, AR prevalence decreased (P for trend<0.0001), while mental health components except stress component showed an increasing trend. Therefore, univariate analysis resulted in a weak relationship between AR and mental health without adjusting for potential confounders, such as age.
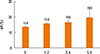
To assess the relationship between AR and 6 components for evaluating mental health, the prevalence of AR was analyzed depending on numbers of components (Fig. 3). In categories with components, the prevalences of AR were 13.8% (0.6), 15.8% (1.0), 16.6% (1.6), and 19.8% (4.5) (P for trend=0.0048).
Among 1,467 AR participants, 1,209 were further tested for subanalysis according to the ARIA guidelines. Subanalysis was performed on AR participants reporting at least 1 subjective allergic symptom, such as sneezing, watery rhinorrhea, nasal obstruction, or itching, without fever or sore throat during the last year. The participants without AR were defined as healthy. According to the ARIA guidelines, the prevalences of intermittent mild, intermittent moderate/severe, persistent mild, and persistent moderate/severe AR were 44.1% (1.9), 26.1% (1.9), 11.3% (1.2), and 18.4% (1.6), respectively. The values of mental health components were higher in the moderate/severe AR group than in the mild AR group and also in the persistent AR group than in the intermittent AR group. After adjustment for age, sex, BMI, smoking status, alcohol use status, and exercise status, all components had a significant P for trend (Table 2).
In multiple logistic regression analysis after adjusting for demographic confounding factors, the odds ratios for stress and suicidal thoughts remained significantly higher in participants with AR. After adjustment for socioeconomic status, borderline results about depressive mood showed more changes in model 2 than in model 1. In model 3, regardless of adjustment for comorbid diseases, there remained significant associations between AR and 3 components of mental health: stress, depressive mood, and psychological consultation components (Table 3).
In this study, we sought to determine whether mental health would correlate with AR in a Korean adult population, which has not yet been addressed in previous studies. Asian countries, including Korea, have undergone rapid westernization and economic development during the past 2 decades. In rapidly changing environments, mental health is of increasing clinical concern. As the prevalence of both AR and mental health-related problems has increased, economic consequences of comorbid depression, anxiety, and AR haves more frequently been reported.22 Relationships between AR and depressive disorders have been described in several reports. However, our cohort taken from a nationally representative sampling of the population represents the general Korean adult population. In addition, mental health was assessed using multidimensional questionnaire about depressive state, physician-diagnosed depression, and anxiety/depression aspect of EQ-5D. Furthermore, subanalysis of AR according to the ARIA guidelines was carried out to evaluate the association of AR severity with mental health. To estimate the exact effect of AR on mental health, we made 3 models to adjust for potential confounders, including demographic characteristics, socioeconomic status, and comorbid diseases. The significance still remained even after adjustment for potential confounding factors.
Tonelli et al.23 studied this association in the aspects of molecular biology, psychoneuroimmunology, and pharmacogenetics. They suggested that intranasal immune challenge could directly influence biochemical responses of the central nervous system, which may lead to psychological disorders. Psychological disorders in allergic patients have been proposed to affect AR, consequently enhancing and prolonging AR symptoms.2425 Postolache et al.14 hypothesized that allergens could trigger suicide in patients who have triple vulnerability to suicide, mood disorders, and allergic sensitization probably via the presence of cytokines. In a physiological aspect, the role of nasal obstruction and its impairing effects on the quality of sleep subsequently result in negative effects on psychiatric symptoms.2627 Also, AR-related disturbances in cognitive function and their subsequent effect on psychological well-being were reported. 2829 Another plausible explanation is that shared genetic risk of both allergies and depression may contribute to this phenomenon of comorbid AR and depression.30
In our study, stress, depressive mood, suicidal thoughts, and psychological consultation factors were correlated with AR after adjustment for demographic characteristics and socioeconomic status. Even after adjustment for comorbid allergic diseases (i.e., asthma and atopic dermatitis), the correlation remained significant with stress, depressive mood, and psychological consultation factors. Thus, our results support the association between AR and poor mental health state. Moreover, mental health components showed a linear the relationship with the severity of AR.
Our study has several limitations. Due to the cross-sectional nature of the collected data, temporal relationships among the conditions cannot be determined. However, the results may be reliable because this is a nationwide population-based study. In addition, the study is also subjected to recall bias because diagnoses of the conditions were self-reported. Even if there are several shortcomings, this study is the first to assess complex relationships between AR and mental health in the general Korean adult population.
This nationwide population-based study indicates that patients with AR appear to be at higher risk of various types of mental health disorders. Moreover, persistent or severe AR was correlated with poor mental health. Therefore, better control of AR may be conducive to better mental health. However, a large number of these patients were not diagnosed or treated for psychological disorders. Thus, more attention should be paid to the psychological status of AR patients, and appropriate treatment should be provided to improve their symptoms.
Figures and Tables
Table 1
General characteristics of the total study population

Table 2
Prevalence and ORs of mental health components in each ARIA group of the AR patients

Table 3
Relationship between allergic rhinitis and mental health using multiple logistic regression analysis

The values represent the multivariate-adjusted odds ratios (95% confidence intervals).
*P<0.05 for the test; †Model 1: Adjusted for age, sex, BMI, smoking status, alcohol use status, and exercise status; ‡Model 2: Adjusted for age, sex, BMI, smoking status, alcohol use status, exercise status, region of residence, income, education, and marital status; §Model 3: Adjusted for age, sex, BMI, smoking status, alcohol use status, exercise status, region of residence, income, education, marital status, asthma, and atopic dermatitis.
References
1. Dykewicz MS, Hamilos DL. Rhinitis and sinusitis. J Allergy Clin Immunol. 2010; 125:S103–S115.
2. Radon K, Gerhardinger U, Schulze A, Zock JP, Norback D, Toren K, et al. Occupation and adult onset of rhinitis in the general population. Occup Environ Med. 2008; 65:38–43.
3. Salo PM, Calatroni A, Gergen PJ, Hoppin JA, Sever ML, Jaramillo R, et al. Allergy-related outcomes in relation to serum IgE: results from the National Health and Nutrition Examination Survey 2005-2006. J Allergy Clin Immunol. 2011; 127:1226–1235.e7.
4. Katelaris CH, Lai CK, Rhee CS, Lee SH, Yun WD, Lim-Varona L, et al. Nasal allergies in the Asian-Pacific population: results from the Allergies in Asia-Pacific Survey. Am J Rhinol Allergy. 2011; 25:S3–S15.
5. Arnedo-Pena A, García-Marcos L, Blanco-Quirós A, Martínez Gimeno A, Aguinaga Ontoso I, González Díaz C, et al. Time trends in prevalence of symptoms of allergic rhinitis in 13-14 year-old schoolchildren in 8 areas of Spain between 1993-1994 and 2001-2002 according to the International Study of Asthma and Allergies in Childhood (ISAAC). Med Clin (Barc). 2004; 123:490–495.
6. Lee SL, Wong W, Lau YL. Increasing prevalence of allergic rhinitis but not asthma among children in Hong Kong from 1995 to 2001 (Phase 3 International Study of Asthma and Allergies in Childhood). Pediatr Allergy Immunol. 2004; 15:72–78.
7. Lee H, Kim GS. Geographical and sociodemographic risk factors for allergic diseases in korean children. Asian Nurs Res. 2011; 5:1–10.
8. Bousquet J, Bullinger M, Fayol C, Marquis P, Valentin B, Burtin B. Assessment of quality of life in patients with perennial allergic rhinitis with the French version of the SF-36 Health Status Questionnaire. J Allergy Clin Immunol. 1994; 94:182–188.
9. Juniper EF. Quality of life in adults and children with asthma and rhinitis. Allergy. 1997; 52:971–977.
10. Juniper EF. Measuring health-related quality of life in rhinitis. J Allergy Clin Immunol. 1997; 99:S742–S749.
11. Meltzer EO, Nathan RA, Seiner JC, Storms W. Quality of life and rhinitic symptoms: results of a nationwide survey with the SF-36 and RQLQ questionnaires. J Allergy Clin Immunol. 1997; 99:S815–S819.
12. Spector SL. Overview of comorbid associations of allergic rhinitis. J Allergy Clin Immunol. 1997; 99:S773–S780.
13. Leynaert B, Neukirch C, Liard R, Bousquet J, Neukirch F. Quality of life in allergic rhinitis and asthma. A population-based study of young adults. Am J Respir Crit Care Med. 2000; 162:1391–1396.
14. Postolache TT, Komarow H, Tonelli LH. Allergy: a risk factor for suicide? Curr Treat Options Neurol. 2008; 10:363–376.
15. Sansone RA, Sansone LA. Allergic rhinitis: relationships with anxiety and mood syndromes. Innov Clin Neurosci. 2011; 8:12–17.
16. Park JE, Lee JY, Jeon HJ, Han KH, Sohn JH, Sung SJ, et al. Age-related differences in the influence of major mental disorders on suicidality: a Korean nationwide community sample. J Affect Disord. 2014; 162:96–101.
17. Johnston R, Brady HE. The rolling cross-section design. Elect Stud. 2002; 21:283–295.
18. Choi JY, Ha HS, Kwon HS, Lee SH, Cho HH, Yim HW, et al. Characteristics of metabolically obese, normal-weight women differ by menopause status: the Fourth Korea National Health and Nutrition Examination Survey. Menopause. 2013; 20:85–93.
19. Cheng HM, Kim S, Park GH, Chang SE, Bang S, Won CH, et al. Low vitamin D levels are associated with atopic dermatitis, but not allergic rhinitis, asthma, or IgE sensitization, in the adult Korean population. J Allergy Clin Immunol. 2014; 133:1048–1055.
20. Nathan RA, Meltzer EO, Seiner JC, Storms W. Prevalence of allergic rhinitis in the United States. J Allergy Clin Immunol. 1997; 99:S808–S814.
21. Choi CJ, Seo M, Choi WS, Kim KS, Youn SA, Lindsey T, et al. Relationship between serum 25-hydroxyvitamin D and lung function among Korean adults in Korea National Health and Nutrition Examination Survey (KNHANES), 2008-2010. J Clin Endocrinol Metab. 2013; 98:1703–1710.
22. Cuffel B, Wamboldt M, Borish L, Kennedy S, Crystal-Peters J. Economic consequences of comorbid depression, anxiety, and allergic rhinitis. Psychosomatics. 1999; 40:491–496.
23. Tonelli LH, Holmes A, Postolache TT. Intranasal immune challenge induces sex-dependent depressive-like behavior and cytokine expression in the brain. Neuropsychopharmacology. 2008; 33:1038–1048.
24. Kiecolt-Glaser JK, Heffner KL, Glaser R, Malarkey WB, Porter K, Atkinson C, et al. How stress and anxiety can alter immediate and late phase skin test responses in allergic rhinitis. Psychoneuroendocrinology. 2009; 34:670–680.
25. Tonelli LH, Katz M, Kovacsics CE, Gould TD, Joppy B, Hoshino A, et al. Allergic rhinitis induces anxiety-like behavior and altered social interaction in rodents. Brain Behav Immun. 2009; 23:784–793.
26. Fang BJ, Tonelli LH, Soriano JJ, Postolache TT. Disturbed sleep: linking allergic rhinitis, mood and suicidal behavior. Front Biosci (Schol Ed). 2010; 2:30–46.
27. Léger D, Annesi-Maesano I, Carat F, Rugina M, Chanal I, Pribil C, et al. Allergic rhinitis and its consequences on quality of sleep: an unexplored area. Arch Intern Med. 2006; 166:1744–1748.
28. Kremer B, den Hartog HM, Jolles J. Relationship between allergic rhinitis, disturbed cognitive functions and psychological well-being. Clin Exp Allergy. 2002; 32:1310–1315.
29. Wilken JA, Berkowitz R, Kane R. Decrements in vigilance and cognitive functioning associated with ragweed-induced allergic rhinitis. Ann Allergy Asthma Immunol. 2002; 89:372–380.
30. Wamboldt MZ, Hewitt JK, Schmitz S, Wamboldt FS, Räsänen M, Koskenvuo M, et al. Familial association between allergic disorders and depression in adult Finnish twins. Am J Med Genet. 2000; 96:146–153.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download