Abstract
Atopic dermatitis (AD) is one of the most common inflammatory allergic diseases with pruritic skin lesions particularly in infancy. It is considered to be the first step of atopic march and has variable disease courses. Many children with AD may resolve their AD symptoms with increasing age and may develop respiratory allergies such as asthma and rhinoconjunctivitis at certain ages. Natural course of AD has been supported by many cross-sectional and longitudinal studies in many countries. In general, atopic dermatitis tends to be more severe and persistent in young children, particularly if they have some risk factors including genetic factors. It appears that approximately 40%-70% of childhood AD will get resolved when they reach the age of 6-7 years. However, it is also observed that over half of the children with AD developed respiratory allergy during late childhood.
Atopic dermatitis (AD) is the most common chronic inflammatory skin diseases in infancy and childhood,1 and often manifests variable disease course among individual patients.
It has been noted that the cumulative prevalence of AD has been increasing in recent years up to 8%-30% of children throughout the world, and the increasing tendency has been keenly observed in Korea.2,3,4,5,6
The prevalence of AD by International Study of Asthma and Allergies in Childhood (ISAAC) in Korea which performed every 5 years since 1995 have shown that the cumulative prevalence of AD in Korean elementary school children has been increased continuously from 19.7% in 1995 to 35.6% in 2010.7
There are many reports regarding the increased risk of developing asthma after AD in early childhood and over half of the children with eczema developed asthma in late childhood.
Therefore, a great number of patients and parents wonder whether AD, once developed, persists throughout the patient's entire life or it can be cured.
Important aspects and also a grave concern of the natural history of AD are the number and chances of patients who will outgrow their disease and progress to allergic march.
Many cross-sectional and longitudinal studies support that the AD as a possible first step to the atopic march. The Tucson Children's Respiratory Study found that eczema during the first year of life is an independent risk factor for persistent wheezing and 18% of children with wheezing at 6 years of age had experienced eczema before 2 years of age.6 The cohort study followed the subjects who reached up to 22 years of age and found that childhood asthma is strongly associated with eczema, whereas adult-onset asthma is not.8 In a German Multicenter Atopy Study, it was revealed that disease severity and atopic sensitization are the major determinants of increased risk of subsequent wheeze or bronchial hyperreactivity.9
The risk of developing asthma was higher in children with eczema, and an early onset of eczema was associated with increased risk of sensitization to inhalant allergens.
AD frequently first occurs at young age and follows a chronic relapsing course as they grow up.7,10 AD is observed primarily during infancy as reported that 45% of AD begin their first symptoms within the first 6 months after birth, 60% during the first year of age and 85% before 5 years of age.9 The incidence and prevalence of AD decreases as patients get older. The Korean National Health Insurance Corporation reported that 26.5% of infants under 2 years old were diagnosed with AD and the rate was reduced dramatically through age from 11.6% in 3 years old to 4.6% in 19 years old according to the report in 2008.7
Until the early 1990s, AD was known as a disease that occurs primarily in infancy and disappears around at 2 to 3 years of age.11 However, it was reported later by another birth cohort study with 1,314 children from birth to 7 years of age that 43.2% of children who had suffered their first AD symptoms within 2 years after birth showed complete remission and 18.7% of the patients experienced continuous symptoms until the age of 3.9
According to the Korea ISAAC study performed in 2010, the prevalence of AD diagnosed ever and symptoms within the last 12 months in 6 to 7 year-old children were 35.6% and 20.6%, respectively. With these findings, we presumed that rather strange but over 40% of the children who had suffered AD during their younger age period tend to show their AD symptoms disappeared.
Less than half of the patients with AD have complete resolution by 7 years of age and only 60% of them have resolution by adulthood, which indicates the chronic nature of AD.12,13
In a high risk cohort study performed in Canada, two-thirds of children developed AD during their first 2 years of life and only 42% of them had persistent AD symptoms at the age of 7 years.14 Another study also reported 37% of children who had early-onset AD continued to have AD at the age of 7 years.9
Hua et al.15 reported the duration of the disease and remission rate of AD in their retrospective population based on birth cohort study with 1,404 child with early-onset AD (onset of disease in the first 2 years of life). They reported that 48.7% had disease duration less than 4 years but 30.2% of patients were still having AD even after 8 years of age. They reported that the remission rate in their study was 69.8%.
Meanwhile, a recent Korean study revealed that 70.6% of children who developed AD under 1 year old showed complete remission of AD by 5 years old.16 In a high risk cohort study, it was reported that one-third of children who had developed AD symptoms after the age of 2 years were mostly non-atopic and not associated with increased risk of respiratory allergy at the age of 7 years.14
Long-term follow-up study up to 20 years with 252 children aged between 6 to 36 months showed that AD completely disappeared in 60.5% of patients at around 6 years old.8 In addition, age of recovery from AD was higher in severe AD cases than in mild or moderate AD cases. Asthma and rhinoconjunctivitis were noted in 34.1% and 57.6% of patients with AD, respectively. Furthermore, children with hen's egg sensitization showed a longer persistence and initial severity and hen's egg sensitization were significantly related to the development of asthma.
A study reported in Taiwan showed that boys may have a longer disease course and a lower remission rate compared to girls among children with early-onset AD.15 In addition, the early-onset age group (under age 1 year) showed a shorter disease course and a higher remission rate than the late-onset age group (between 1 to 2 years old). However, previous studies demonstrated that earlier onset of AD have a lower remission rate.15
As a natural course of AD, it is impossible to find definitive answer or correct information at the moment. Nevertheless, at least we can find certain patterns of possibility that about half of the children with early-onset AD may recover from their AD symptoms before they enter elementary school (Table).
Many studies on AD development showed that boys more frequently develop AD than girls during infancy and that there is a switch to girl predominance in adolescence.19,20
Genetic factors and atopic sensitization were major determinants of prognosis of AD.8 Parental history of atopic disease, feeding type, presence of siblings, socioeconomic status and several environmental factors including indoor and outdoor exposure to allergens,21,22 and environmental tobacco smoke,23,24 have a relevant influence on the outcomes of AD in infancy.
Peters et al.25 studied the course of AD over puberty and risk factors with respect to incidence, recurrence and persistence of AD until adolescence. They reported that probability of the incidence, recurrence and persistence of adolescent AD ranged from 0.14%, 9.3%, and 28.3% without any risk factors they assessed, respectively, and up to 21.4%, 81.7%, and 87.6% with all risk factors, respectively. In particular, parental history of AD and/or rhinitis and allergen sensitization during early school ages were the most relevant childhood predictors for the course of AD over puberty.
It is widely known that early AD is associated with positive skin test reactivity to food and inhalant allergens.21,26,27,28 However, another study reported that skin test positivity to house dust mites at 7 years of age was not associated with the time of AD developed; however, skin test positivity for cat and fungal allergens were significantly associated with persistent AD.14
Children with AD who were sensitized to common environmental allergens presented by the age of 2 to 4 years were at a higher risk for progressing to respiratory allergy than those without allergen sensitization.29 Approximately 70% of children with severe AD develop asthma compared with 20%-30% of children with mild AD.30
Many studies have suggested that food allergy is a strong risk factor for the development of other allergic diseases in late childhood.31 Comorbidity with food allergy significantly lowers the onset age of AD.31 Family history of AD can also be a significant risk factor for the development of AD. Regarding factors associated with the improvement and recurrence of AD, early-onset AD has a higher probability of improvement than late-onset AD, and psychological stress and sleep disturbance tend to contribute to significantly higher recurrence rates.
Filaggrin (FLG) is a protein that facilitates epidermal terminal differentiation and formation of the skin barrier that is the uppermost layer of the epidermis. This insoluble skin barrier has key function to protect against environmental agents and prevent epidermal water loss.34 In normal skin, upon terminal differentiation of keratinocytes, the FLG, products of degradation, aggregate keratin filaments and flatten keratinocytes to form an effective barrier to external allergens.35
Many reports strongly support the hypothesis that AD patients tend to have skin barrier defects,36,37 and there is a link of AD to the chromosome locus on 1q21, which contains the epidermal differentiation complex where FLG resides.38 Palmer et al.,39 first reported that loss-of-function mutations of FLG leads to impaired barrier function which manifests as a typical symptoms of AD. They also found that there is a causal relationship between AD and heterozygous carriers of 2 null FLG mutations, with a relative risk of 13.4.
Many cohort studies on FLG mutations in AD reported approximately 25% to 50% of AD patients have FLG mutations.40 So far, more than 40 FLG mutations have been reported, and the frequency and prevalent FLG mutations are different among countries.41
Significant associations were observed for both R501X and 2282del4 mutations and AD among European American subjects, but the frequency of R501X mutations was 3 times higher for AD eczema herpeticum than for AD without eczema herpeticum.42 In addition, the FLG mutation studies performed in Asian countries including Japan, China, Taiwan, and Korea reported that only 2 identical mutations (R501X and E2422X) were found in both European and Asian people.43,44,45,46
In a study of Korean people, the FLG null mutation E2422X was not detected in any patients with AD or control subjects. R501X null mutation was detected in only 1 child with AD (0.1%). Children with AD had 3321delA deletion significantly more frequently (2.4%) than the control subjects (0.0%, P<0.001). Children with AD also had a significantly higher combined allele frequency of the 3 FLG null mutations (2.6%) than the controls (0.0%, P<0.001). The 3321delA null mutation was not significantly associated with AD severity (P=0.842). When the patients with AD were divided into allergic AD and non-allergic AD groups, these 2 groups did not differ in terms of the frequency of 3321delA.47
FLG mutations seem likely to play a role in chronicity of the disease and IgE sensitization in patients with AD. Recent studies have shown that patients with early-onset AD and FLG mutations have a tendency to have persistent disease into adulthood.48
FLG mutations are currently considered a major risk factor for AD, particularly in patients who have onset of AD at 2 years or younger.49 Meta analysis of FLG mutation studies on AD with R501X and 2282del4 found an overall OR of 4.78 from the case control studies and a summary OR of 1.99 from the family studies.50 Since each population is likely to have a unique set of FLG mutations, we should obtain information on prevalent FLG mutations from each population.
Since vitamin D is required for normal keratinocyte proliferation, differentiation and function, disturbed or insufficient vitamin D metabolism could directly influence keratinocytes and their intrinsic functions.51,52,53
After Wang et al.54 demonstrated that vitamin D plays an important role in antimicrobial cutaneous immunity, other groups confirmed the direct connection between vitamin D metabolism and cutaneous innate defense function.55,56 A recent study by a Japanese working group of AD reported that patients with AD have low vitamin D serum levels which correlate with low serum levels of cathelicidin peptide.57 Both cathelicidin and defensins are well known antimicrobial peptide gene families in skin and activated by skin inflammation, skin infection and UVB irradiation.58
There are some studies that have revealed an increasing prevalence of community-associated methicillin-resistant S. aureus (MRSA) among patients with AD and the role of vitamin D in the immunopathogenesis of AD. Another study showed that serum levels of 25(OH)D were lower in the MRSA group, without statistical significance.35
The relationship between serum vitamin D levels and AD has not yet been completely identified; thus, this issue still controversial. It could be only a conjecture, but Vitamin D might have an important role in antimicrobial cutaneous immunity in AD.
Obesity has been shown to have several effects on the immune system that might modulate the severity of atopic diseases.59 However, an association between obesity and AD has not yet been well established.
A previous retrospective case-control pediatric cohort study demonstrated that obesity persisting more than 5 years and starting early in life (before 5 years of age) are associated with increased risk for AD and AD severity.60 Therefore, intervention for weight loss might be an important strategy for the treatment of AD in children.
AD generally tends to be more severe and persistent in young children, particularly if they have some risk factors, including genetic factors. Approximately 40%-70% of childhood AD cases will resolve by the time they reach the age of 6-7 years. However, we also observed that over half of the children with AD developed respiratory allergy, such as asthma and rhinoconjunctivitis during late childhood. Therefore, an early interventional strategy to reduce the persistence rate of AD and prevent atopic march will be a key homework for all allergists.
Figures and Tables
Table
Summary of age and rate of resolution of atopic dermatitis in each country
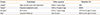
| Country | Study design | Follow-up period | Resolution (%) |
|---|---|---|---|
| Canada13 | High-risk birth cohort with intervention | Birth to 7 years of age | 58% |
| Taiwan14 | Population based birth cohort | Birth to 10 years of age | 69.8% |
| Germany9 | Birth cohort | Birth to 7 years of age | 43.2% at the age of 3 years |
| Italy16 | Long-term follow-up | Over 20 years | 60.5% at the age of 6 years |
References
1. Leung DY, Bieber T. Atopic dermatitis. Lancet. 2003; 361:151–160.
2. Bieber T. Atopic dermatitis. N Engl J Med. 2008; 358:1483–1494.
3. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006; 368:733–743.
4. Williams H, Stewart A, von Mutius E, Cookson W, Anderson HR. International Study of Asthma and Allergies in Childhood (ISAAC) Phase One and Three Study Groups. Is eczema really on the increase worldwide? J Allergy Clin Immunol. 2008; 121:947–954.e15.
5. Oh JW, Pyun BY, Choung JT, Ahn KM, Kim CH, Song SW, et al. Epidemiological change of atopic dermatitis and food allergy in school-aged children in Korea between 1995 and 2000. J Korean Med Sci. 2004; 19:716–723.
6. Lee JH, Kim EH, Cho J, Kim HY, Suh J, Ahn K, et al. Comparison of prevalence and risk factors of atopic dermatitis by physical examination and questionnaire survey in elementary school children. Pediatr Allergy Respir Dis. 2011; 21:186–196.
7. Lee SI, Kim J, Han Y, Ahn K. A proposal: Atopic Dermatitis Organizer (ADO) guideline for children. Asia Pac Allergy. 2011; 1:53–63.
8. Ricci G, Patrizi A, Baldi E, Menna G, Tabanelli M, Masi M. Long-term follow-up of atopic dermatitis: retrospective analysis of related risk factors and association with concomitant allergic diseases. J Am Acad Dermatol. 2006; 55:765–771.
9. Illi S, von Mutius E, Lau S, Nickel R, Grüber C, Niggemann B, et al. Multicenter Allergy Study Group. The natural course of atopic dermatitis from birth to age 7 years and the association with asthma. J Allergy Clin Immunol. 2004; 113:925–931.
10. Kay J, Gawkrodger DJ, Mortimer MJ, Jaron AG. The prevalence of childhood atopic eczema in a general population. J Am Acad Dermatol. 1994; 30:35–39.
11. Rudolph AM. Rudolph's pediatrics. 19th ed. Norwalk (CT): Appleton and Lange;1991.
12. Spergel JM, Paller AS. Atopic dermatitis and the atopic march. J Allergy Clin Immunol. 2003; 112:S118–S127.
13. Spergel JM. From atopic dermatitis to asthma: the atopic march. Ann Allergy Asthma Immunol. 2010; 105:99–106.
14. Carlsten C, Dimich-Ward H, Ferguson A, Watson W, Rousseau R, Dybuncio A, et al. Atopic dermatitis in a high-risk cohort: natural history, associated allergic outcomes, and risk factors. Ann Allergy Asthma Immunol. 2013; 110:24–28.
15. Hua TC, Hwang CY, Chen YJ, Chu SY, Chen CC, Lee DD, et al. The natural course of early-onset atopic dermatitis in Taiwan: a population-based cohort study. Br J Dermatol. 2014; 170:130–135.
16. Chung Y, Kwon JH, Kim J, Han Y, Lee SI, Ahn K. Retrospective analysis of the natural history of atopic dermatitis occurring in the first year of life in Korean children. J Korean Med Sci. 2012; 27:723–728.
17. Rystedt I. Long term follow-up in atopic dermatitis. Acta Derm Venereol Suppl (Stockh). 1985; 114:117–120.
18. Rystedt I. Prognostic factors in atopic dermatitis. Acta Derm Venereol. 1985; 65:206–213.
19. Hagendorens MM, Bridts CH, Lauwers K, van Nuijs S, Ebo DG, Vellinga A, et al. Perinatal risk factors for sensitization, atopic dermatitis and wheezing during the first year of life (PIPO study). Clin Exp Allergy. 2005; 35:733–740.
20. Girolomoni G, Abeni D, Masini C, Sera F, Ayala F, Belloni-Fortina A, et al. The epidemiology of atopic dermatitis in Italian schoolchildren. Allergy. 2003; 58:420–425.
21. Capristo C, Romei I, Boner AL. Environmental prevention in atopic eczema dermatitis syndrome (AEDS) and asthma: avoidance of indoor allergens. Allergy. 2004; 59:Suppl 78. 53–60.
22. Harris JM, Williams HC, White C, Moffat S, Mills P, Newman Taylor AJ, Cullinan P. Early allergen exposure and atopic eczema. Br J Dermatol. 2007; 156:698–704.
23. Kimata H. Cessation of passive smoking reduces allergic responses and plasma neurotrophin. Eur J Clin Invest. 2004; 34:165–166.
24. Arruda LK, Solé D, Baena-Cagnani CE, Naspitz CK. Risk factors for asthma and atopy. Curr Opin Allergy Clin Immunol. 2005; 5:153–159.
25. Peters AS, Kellberger J, Vogelberg C, Dressel H, Windstetter D, Weinmayr G, et al. Prediction of the incidence, recurrence, and persistence of atopic dermatitis in adolescence: a prospective cohort study. J Allergy Clin Immunol. 2010; 126:590–595.e1-3.
26. Bergmann RL, Edenharter G, Bergmann KE, Forster J, Bauer CP, Wahn V, et al. Atopic dermatitis in early infancy predicts allergic airway disease at 5 years. Clin Exp Allergy. 1998; 28:965–970.
27. Gustafsson D, Sjöberg O, Foucard T. Development of allergies and asthma in infants and young children with atopic dermatitis--a prospective follow-up to 7 years of age. Allergy. 2000; 55:240–245.
28. Jøhnke H, Norberg LA, Vach W, Høst A, Andersen KE. Patterns of sensitization in infants and its relation to atopic dermatitis. Pediatr Allergy Immunol. 2006; 17:591–600.
29. Novembre E, Cianferoni A, Lombardi E, Bernardini R, Pucci N, Vierucci A. Natural history of "intrinsic" atopic dermatitis. Allergy. 2001; 56:452–453.
30. Zheng T, Yu J, Oh MH, Zhu Z. The atopic march: progression from atopic dermatitis to allergic rhinitis and asthma. Allergy Asthma Immunol Res. 2011; 3:67–73.
31. Kijima A, Murota H, Takahashi A, Arase N, Yang L, Nishioka M, Yamaoka T, Kitaba S, Yamauchi-Takihara K, Katayama I. Prevalence and impact of past history of food allergy in atopic dermatitis. Allergol Int. 2013; 62:105–112.
32. Marenholz I, Kerscher T, Bauerfeind A, Esparza-Gordillo J, Nickel R, Keil T, et al. An interaction between filaggrin mutations and early food sensitization improves the prediction of childhood asthma. J Allergy Clin Immunol. 2009; 123:911–916.
33. Filipiak-Pittroff B, Schnopp C, Berdel D, Naumann A, Sedlmeier S, Onken A, et al. Predictive value of food sensitization and filaggrin mutations in children with eczema. J Allergy Clin Immunol. 2011; 128:1235–1241.e5.
34. Candi E, Schmidt R, Melino G. The cornified envelope: a model of cell death in the skin. Nat Rev Mol Cell Biol. 2005; 6:328–340.
35. Min TK, Yang HJ, Lee HW, Pyun BY. Correlation between serum 25-hydroxyvitamin D levels and methicillin - resistant Staphylococcus aureus skin colonization in atopic dermatitis. Allergy Asthma Respir Dis. 2013; 1:138–143.
36. Aalto-Korte K. Improvement of skin barrier function during treatment of atopic dermatitis. J Am Acad Dermatol. 1995; 33:969–972.
37. Hata M, Tokura Y, Takigawa M, Sato M, Shioya Y, Fujikura Y, Imokawa G. Assessment of epidermal barrier function by photoacoustic spectrometry in relation to its importance in the pathogenesis of atopic dermatitis. Lab Invest. 2002; 82:1451–1461.
38. Compton JG, DiGiovanna JJ, Johnston KA, Fleckman P, Bale SJ. Mapping of the associated phenotype of an absent granular layer in ichthyosis vulgaris to the epidermal differentiation complex on chromosome 1. Exp Dermatol. 2002; 11:518–526.
39. Palmer CN, Irvine AD, Terron-Kwiatkowski A, Zhao Y, Liao H, Lee SP, et al. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet. 2006; 38:441–446.
40. Irvine AD, McLean WH. Breaking the (un)sound barrier: filaggrin is a major gene for atopic dermatitis. J Invest Dermatol. 2006; 126:1200–1202.
41. Akiyama M. FLG mutations in ichthyosis vulgaris and atopic eczema: spectrum of mutations and population genetics. Br J Dermatol. 2010; 162:472–477.
42. Gao PS, Rafaels NM, Hand T, Murray T, Boguniewicz M, Hata T, Schneider L, Hanifin JM, Gallo RL, Gao L, Beaty TH, Beck LA, Barnes KC, Leung DY. Filaggrin mutations that confer risk of atopic dermatitis confer greater risk for eczema herpeticum. J Allergy Clin Immunol. 2009; 124:507–513. 513.e1–513.e7.
43. Hamada T, Sandilands A, Fukuda S, Sakaguchi S, Ohyama B, Yasumoto S, McLean WH, Hashimoto T. De novo occurrence of the filaggrin mutation p.R501X with prevalent mutation c.3321delA in a Japanese family with ichthyosis vulgaris complicated by atopic dermatitis. J Invest Dermatol. 2008; 128:1323–1325.
44. Chen H, Ho JC, Sandilands A, Chan YC, Giam YC, Evans AT, Lane EB, McLean WH. Unique and recurrent mutations in the filaggrin gene in Singaporean Chinese patients with ichthyosis vulgaris. J Invest Dermatol. 2008; 128:1669–1675.
45. Hsu CK, Akiyama M, Nemoto-Hasebe I, Nomura T, Sandilands A, Chao SC, Lee JY, Sheu HM, McLean WH, Shimizu H. Analysis of Taiwanese ichthyosis vulgaris families further demonstrates differences in FLG mutations between European and Asian populations. Br J Dermatol. 2009; 161:448–451.
46. Kang TW, Lee JS, Oh SW, Kim SC. Filaggrin mutation c.3321delA in a Korean patient with ichthyosis vulgaris and atopic dermatitis. Dermatology. 2009; 218:186–187.
47. Yu HS, Kang MJ, Jung YH, Kim HY, Seo JH, Kim YJ, Lee SH, Kim HJ, Kwon JW, Kim BJ, Yu J, Hong SJ. Mutations in the Filaggrin are Predisposing Factor in Korean Children With Atopic Dermatitis. Allergy Asthma Immunol Res. 2013; 5:211–215.
48. Barker JN, Palmer CN, Zhao Y, Liao H, Hull PR, Lee SP, Allen MH, Meggitt SJ, Reynolds NJ, Trembath RC, McLean WH. Null mutations in the filaggrin gene (FLG) determine major susceptibility to early-onset atopic dermatitis that persists into adulthood. J Invest Dermatol. 2007; 127:564–567.
49. Stemmler S, Parwez Q, Petrasch-Parwez E, Epplen JT, Hoffjan S. Two common loss-of-function mutations within the filaggrin gene predispose for early onset of atopic dermatitis. J Invest Dermatol. 2007; 127:722–724.
50. van den Oord RA, Sheikh A. Filaggrin gene defects and risk of developing allergic sensitisation and allergic disorders: systematic review and meta-analysis. BMJ. 2009; 339:b2433.
51. Lehmann B. Role of the vitamin D3 pathway in healthy and diseased skin--facts, contradictions and hypotheses. Exp Dermatol. 2009; 18:97–108.
52. Bikle DD, Pillai S, Gee E, Hincenbergs M. Regulation of 1,25-dihydroxyvitamin D production in human keratinocytes by interferon-gamma. Endocrinology. 1989; 124:655–660.
53. Bikle DD. Vitamin D regulated keratinocyte differentiation. J Cell Biochem. 2004; 92:436–444.
54. Wang TT, Nestel FP, Bourdeau V, Nagai Y, Wang Q, Liao J, Tavera-Mendoza L, Lin R, Hanrahan JW, Mader S, White JH. Cutting edge: 1,25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J Immunol. 2004; 173:2909–2912.
55. Gombart AF, Borregaard N, Koeffler HP. Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly up-regulated in myeloid cells by 1,25-dihydroxyvitamin D3. FASEB J. 2005; 19:1067–1077.
56. Schauber J, Gallo RL. Antimicrobial peptides and the skin immune defense system. J Allergy Clin Immunol. 2008; 122:261–266.
57. Kanda N, Hau CS, Tada Y, Sato S, Watanabe S. Decreased serum LL-37 and vitamin D3 levels in atopic dermatitis: relationship between IL-31 and oncostatin M. Allergy. 2012; 67:804–812.
58. Roider E, Ruzicka T, Schauber J. Vitamin d, the cutaneous barrier, antimicrobial peptides and allergies: is there a link? Allergy Asthma Immunol Res. 2013; 5:119–128.
59. Martín-Romero C, Santos-Alvarez J, Goberna R, Sánchez-Margalet V. Human leptin enhances activation and proliferation of human circulating T lymphocytes. Cell Immunol. 2000; 199:15–24.
60. Silverberg JI, Kleiman E, Lev-Tov H, Silverberg NB, Durkin HG, Joks R, et al. Association between obesity and atopic dermatitis in childhood: a case-control study. J Allergy Clin Immunol. 2011; 127:1180–1186.e1.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download