Abstract
Recent studies have shown that high consumption of processed meat may be associated with increasing risk of metabolic syndrome, which have been suggested as a predictor of diabetes and cardiovascular disease. However, limited studies have investigated this association in Korean population. The purpose of this study was to investigate the cross-sectional association between processed meat/unprocessed (beef, pork, chicken) intakes and the prevalence of metabolic syndrome. Using data from 2007-2008 Korean National Health and Nutrition Examination Survey (KNHANES), we analyzed data including 5,545 men and women who were aged older than 20 years, and who were free of chronic disease such as hypertension, type 2 diabetes and cardiovascular disease. Subjects who frequently consumed processed meat tended to be younger and more likely to be current smokers. In addition, men were more likely to consume processed meat than women. Although higher processed/unprocessed meat intakes were significantly associated with the lower risk of metabolic syndrome in a crude model, these associations were no longer significant after adjustment for potential confounding factors. For example, comparing subjects in the highest intake quartile of processed meat with the lowest intake group, the multivariate-adjusted odds ratio (OR) of metabolic syndrome was 0.92 (95% CI: 0.58-1.46) for processed meat, 1.09 (95% CI: 0.76-1.56) for beef, 1.10 (95% CI: 0.74-1.62) for pork and 0.75 (95% CI: 0.51-1.12) for chicken. In conclusion, we found no evidence of any adverse effects of frequent processed or unprocessed meat intakes on the prevalence of metabolic syndrome among Korean adults at the exposure levels seen in this study.
Figures and Tables
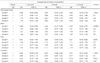
Table 4
General characteristics of subjects according to the frequency of processed meat intake (n=5,545)

Table 6
Dietary intakes according to the frequency of processed meat intake: The 24-hour recall data

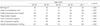
Table 7
Association between processed/unprocessed meat intakes and prevalence of metabolic syndrome
Model 1: Unadjustment, Model 2: Adjustment for age (year), sex and income (low, mid-low, mid-high, high), Model 3: Additional adjustment for alcohol consumption (never, ≤ 1/month, 2-4/month, 2-3/week, ≥ 4/week), smoking status (never, former, current), physical activity (low, moderate, active) and BMI (kg/m2), Model 4: Model 3 + Additional adjustment for total energy (kcal/day), fat (g/day), carbohydrate (g/day), fiber (g/day), Na (mg/day), Fe (mg/day), K (mg/day), vitamin A (µgRE/day), vitamin C (mg/day) intakes
References
1. Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation. 2008. 117(6):754–761.

2. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F. American Heart Association. National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005. 112(17):2735–2752.
3. McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, Ballantyne CM, Heiss G. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005. 28(2):385–390.

4. Bonora E, Targher G, Formentini G, Calcaterra F, Lombardi S, Marini F, Zenari L, Saggiani F, Poli M, Perbellini S, Raffaelli A, Gemma L, Santi L, Bonadonna RC, Muggeo M. The Metabolic Syndrome is an independent predictor of cardiovascular disease in Type 2 diabetic subjects. Prospective data from the Verona Diabetes Complications Study. Diabet Med. 2004. 21(1):52–58.

5. Korea Centers for Disease Control and Prevention. Korea Health Industry Development Institute. In-depth analysis on the 3rd Korea national health and nutrition examination survey. 2007.
6. Ministry of Health & Welfare, Korea Centers for Disease Control and Prevention. 2008 national health statistic: the 4th Korea national health and nutrition examination survey. 2008.
7. Rosell MS, Hellénius ML, de Faire UH, Johansson GK. Associations between diet and the metabolic syndrome vary with the validity of dietary intake data. Am J Clin Nutr. 2003. 78(1):84–90.

8. Esmaillzadeh A, Mirmiran P, Azizi F. Whole-grain consumption and the metabolic syndrome: a favorable association in Tehranian adults. Eur J Clin Nutr. 2005. 59(3):353–362.

9. Freire RD, Cardoso MA, Gimeno SG, Ferreira SR. Japanese-Brazilian Diabetes Study Group. Dietary fat is associated with metabolic syndrome in Japanese Brazilians. Diabetes Care. 2005. 28(7):1779–1785.

10. Mennen LI, Lafay L, Feskens EJM, Novak M, Lépinay P, Balkau B. Possible protective effect of bread and dairy products on the risk of the metabolic syndrome. Nutr Res. 2000. 20(3):335–347.

11. Azadbakht L, Esmaillzadeh A. Red meat intake is associated with metabolic syndrome and the plasma C-reactive protein concentration in women. J Nutr. 2009. 139(2):335–339.

12. Damião R, Castro TG, Cardoso MA, Gimeno SG, Ferreira SR. Japanese-Brazilian Diabetes Study Group. Dietary intakes associated with metabolic syndrome in a cohort of Japanese ancestry. Br J Nutr. 2006. 96(3):532–538.
13. Babio N, Sorlí M, Bulló M, Basora J, Ibarrola-Jurado N, Fernández-Ballart J, Martínez-González MA, Serra-Majem L, González-Pérez R, Salas-Salvadó J. Association between red meat consumption and metabolic syndrome in a Mediterranean population at high cardiovascular risk: Cross-sectional and 1-year follow-up assessment. Nutr Metab Cardiovasc Dis. 2010. [Epub ahead of print].

14. Yoon GS, Woo J. The perception and the consumption behavior for the meats in Koreans. J Korean Soc Food Sci Nutr. 1999. 28(1):246–256.
15. Ministry of Health & Welfare. The third Korea national health and nutrition examination survey (KNHANES III). 2006.
16. Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A, Nathan D, Palmer J, Rizza R, Saudek C, Shaw J, Steffes M, Stern M, Tuomilehto J, Zimmet P. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003. 26(11):3160–3167.

17. Wang Y, Beydoun MA, Caballero B, Gary TL, Lawrence R. Trends and correlates in meat consumption patterns in the US adult population. Public Health Nutr. 2010. 13(9):1333–1345.

18. Männistö S, Kontto J, Kataja-Tuomola M, Albanes D, Virtamo J. High processed meat consumption is a risk factor of type 2 diabetes in the Alpha-Tocopherol, Beta-Carotene Cancer Prevention study. Br J Nutr. 2010. 103(12):1817–1822.

19. Fung TT, Schulze M, Manson JE, Willett WC, Hu FB. Dietary patterns, meat intake, and the risk of type 2 diabetes in women. Arch Intern Med. 2004. 164(20):2235–2240.

20. Kahn HS, Tatham LM, Heath CW Jr. Contrasting factors associated with abdominal and peripheral weight gain among adult women. Int J Obes Relat Metab Disord. 1997. 21(10):903–911.

21. Schulz M, Kroke A, Liese AD, Hoffmann K, Bergmann MM, Boeing H. Food groups as predictors for short-term weight changes in men and women of the EPIC-Potsdam cohort. J Nutr. 2002. 132(6):1335–1340.

22. Bes-Rastrollo M, Sánchez-Villegas A, Gómez-Gracia E, Martínez JA, Pajares RM, Martínez-González MA. Predictors of weight gain in a Mediterranean cohort: the Seguimiento Universidad de Navarra Study 1. Am J Clin Nutr. 2006. 83(2):362–370. quiz 394-395.

23. van Dam RM, Willett WC, Rimm EB, Stampfer MJ, Hu FB. Dietary fat and meat intake in relation to risk of type 2 diabetes in men. Diabetes Care. 2002. 25(3):417–424.

24. Feskens EJ, Virtanen SM, Räsänen L, Tuomilehto J, Stengård J, Pekkanen J, Nissinen A, Kromhout D. Dietary factors determining diabetes and impaired glucose tolerance. A 20-year follow-up of the Finnish and Dutch cohorts of the Seven Countries Study. Diabetes Care. 1995. 18(8):1104–1112.

25. Lee DH, Folsom AR, Jacobs DR Jr. Dietary iron intake and Type 2 diabetes incidence in postmenopausal women: the Iowa Women's Health Study. Diabetologia. 2004. 47(2):185–194.

26. Rajpathak S, Ma J, Manson J, Willett WC, Hu FB. Iron intake and the risk of type 2 diabetes in women: a prospective cohort study. Diabetes Care. 2006. 29(6):1370–1376.
27. Knight TM, Forman D, Al-Dabbagh SA, Doll R. Estimation of dietary intake of nitrate and nitrite in Great Britain. Food Chem Toxicol. 1987. 25(4):277–285.
28. Rajpathak SN, Crandall JP, Wylie-Rosett J, Kabat GC, Rohan TE, Hu FB. The role of iron in type 2 diabetes in humans. Biochim Biophys Acta. 2009. 1790(7):671–681.

29. Papakonstantinou E, Panagiotakos DB, Pitsavos C, Chrysohoou C, Zampelas A, Skoumas Y, Stefanadis C. Food group consumption and glycemic control in people with and without type 2 diabetes: the ATTICA study. Diabetes Care. 2005. 28(10):2539–2540.

30. Hua NW, Stoohs RA, Facchini FS. Low iron status and enhanced insulin sensitivity in lacto-ovo vegetarians. Br J Nutr. 2001. 86(4):515–519.

31. Tuomainen TP, Nyyssönen K, Salonen R, Tervahauta A, Korpela H, Lakka T, Kaplan GA, Salonen JT. Body iron stores are associated with serum insulin and blood glucose concentrations. Population study in 1,013 eastern Finnish men. Diabetes Care. 1997. 20(3):426–428.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download