Abstract
BACKGROUNDS/OBJECTIVES
The effects of malnutrition on growth of toddlers and preschoolers by socioeconomic status are not well known. This study aimed to examine the effects of dietary intake on growth outcomes in toddlers and preschoolers by household income level.
SUBJECTS/METHODS
The study population was a total of 1,687 children aged 1 to 5 years that participated in the KNHANES from 2009 to 2011. Growth of children was assessed by height for age (HFA) and weight for height (WFH). Children were classified into three groups according to children's HFA and WFH compared to the 10th and 90th percentiles of the 2007 Korean Children and Adolescent Growth Standard. Average monthly household income was divided into quartile groups. Dietary intake data were obtained by using the one day 24-hr recall method. Risks of inadequate intake of nutrients and unfavorable growth were estimated by using a multiple logistic regression model adjusted for sex, age, region, and energy intake.
RESULTS
The low HFA group (< 10th percentile) had significantly lower intakes of energy, carbohydrate, and thiamin as compared with the high group (≥ 90th percentile). For WFH status, vitamin C intake was lower in the low group than in the high group. Household income level was related to WFH status but not HFA. Children from lower income households were more likely to have high WFH than those from higher income households (P for trend = 0.038). Household income status was also significantly related with risk of inadequate intake of micronutrients such as thiamin (P for trend = 0.032) and vitamin C (P for trend = 0.002), showing higher odds of inadequate intakes in children from lower income households.
Growth is one relevant indicator of a child's nutritional status and is a tool for assessing health and well-being of children [1]. Generally, child growth status is based on length, height, weight, and age and is generally assessed based on the combined indicators of length/height for age (stunting), weight for length/height (wasting), and weight for age (under-weight) etc. [2]. One of the most important risk factors of growth failure is poor nutritional status, especially in early age. Adequate nutrition supply during childhood also strongly promotes cognitive achievement and prevents onset of chronic diseases in later life [3].
Given the growing burden of non-communicable diseases (NCDs) in both industrialized and developing countries, the double burden of malnutrition including under-nutrition and overweight has also increased worldwide [45]. Chronic under-nutrition during childhood could lead to increased risk of developing a thrifty phenotype resulting in adverse health outcomes later in life, especially if the growing child is exposed to over-nutrition [678]. Specifically, in early life, malnutrition problems such as obesity related to stunting are known to promote growth retardation [91011].
There are many studies that have demonstrated hunger and food insecurity as causes of malnutrition as well as an association with both overweight and growth failure. Recently, children from households with low economic status tend to be affected by food insecurity and are more likely to consume unhealthy foods [12] and be overweight [1314].
However, studies on the relationships among dietary intake, growth development, and overweight by socioeconomic status in toddlers and preschoolers are still limited. Therefore, this study aimed to examine the effect of dietary intake on growth status in toddlers and preschoolers by household income level using the cross-sectional surveys of the 2009-2011 Korea National Health and Nutrition Examination Survey (KNHANES).
This study used data from the KNHANES conducted by the Korean Ministry of Health and Welfare. This cross-sectional survey has been conducted periodically since 1998. The participants were recruited among non-institutionalized civilians, and a stratified, multistage probability sampling design was applied for the selection of household units. Detailed description of the survey has been reported elsewhere [15].
This study was based on data from a total of 1,870 children aged 1 to 5 years that participated in the surveys from 2009 to 2011. Those without complete information for all variables considered in this analysis were excluded: First, children without information on household income were excluded (16 cases excluded). Second, those without dietary intake and anthropometric data were excluded (167 cases excluded). Finally, an analytic data set on 1,687 eligible children was constructed to investigate the association between household income and nutrition and growth in young children.
Survey data included children's gender, age in months, household income, weight, height, and energy and nutrient intake. Socio-demographic data were collected by an interviewer-administered questionnaire. Average monthly household income was divided into quartile groups (low, mid-low, mid-high, or high). The anthropometric data were measured according to standardized protocol: each participant dressed in light clothing without shoes; weight was determined to the nearest 0.1 kg on a medical balance (GL-6000-20, CAS, Seoul, Korea); height was measured to the nearest 0.1 cm with a wall-mounted stadiometer (Seca 220, Seca, Hamburg, Germany). For growth assessment of children, growth indices of height for age (HFA) and weight for height (WFH) were used. Study children were classified into three groups according to children's HFA and WFH compared to the 10th and 90th percentiles of the 2007 Korean Children and Adolescent Growth Standard. Children with growth percentiles less than the 10th percentile were classified into the low group while those with growth percentiles equal to the 90th percentile or higher were in the high group. Unfavorable growth status was defined as low HFA, low WFH, or high WFH. Dietary intake data were obtained by using the one day 24-hr recall method. All participants were requested to maintain their usual diets, and experienced interviewers instructed participants to recall and describe every food and beverage consumed during the previous 24 hr. Food models and measuring bowls, cups, and spoons were used to assist estimation of portion sizes. Micronutrient intakes were compared to Estimated Average Requirement (EAR) and Recommended Nutrient Intake (RNI) to evaluate nutrient adequacy according to age and sex.
All estimates were produced to represent the Korean population using sample weight. Descriptive statistics were presented as percentage frequency or mean and standard error (SE). Analysis of covariance (ANCOVA) was applied using a multivariate regression model to control for confounding variable, age, in comparison with nutrient intake according to growth status. The risk estimates of inadequate nutrients below EAR and unfavorable growth status were presented as odds ratios (ORs) and 95% confidence intervals by household income levels. The logistic regression model was used for multivariate analysis to calculate ORs controlling for sex, age, region, and energy intake. Statistical significance was set at P < 0.05. Pooled weight was calculated to analyze the combined data set of the 2009-2011 KNHANES with consideration for the number of sample units. Taylor series method was applied to account for the multistage clustered sampling design. All analyses were performed by using SAS 9.3.
The general characteristics of the subjects are shown in Table 1. Average monthly household incomes in each income group were 1,135,838 won for low, 2,244,401 won for mid-low, 3,563,878 won for mid-high, and 9,686,570 won for high. The subjects were aged approximately 3 years, and the proportion of boys was 52.2%. About 69% of subjects were in the middle level of household income, and the proportion of those with low household income was relatively low at 9%. The mean value of total energy was 1,198.9 kcal, and the percentages of carbohydrates, protein, and fat from energy intake were 64.4%, 13.9%, and 21.7%, respectively. Lower percentage of RNI was measured for calcium at 85.6 ± 1.9%.
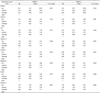
Nutrient intakes according to growth status are presented in Table 2. The nutrients showing significantly different intakes by HFA status were total energy, carbohydrates, and thiamin. The low HFA group had lower intakes of nutrients as compared with the high HFA group. In terms of WFH status, vitamin C intake was lower in the low group than high group (62.2 mg versus 80.3 mg). The percentage of RNI was different for thiamin between groups by HFA status (P = 0.033) as well as vitamin C between groups by WFH status (P = 0.036), which showed relatively lower intakes in the low than high group.
Table 3 presents the effects of household income on unfavorable growth status. Household income level was not related to low HFA. However, in terms of WFH, risk of high WFH was associated with lower household income status (P for trend = 0.038). Children in the lowest household income level were 2.34 times more likely to have high WFH than those from higher household income (95% confidence interval 1.15-4.75).
The effects of household income on inadequate nutrient intakes less than EAR are shown in Table 4. Household income level was not associated with energy intake (data not shown), whereas children from lower household income tended to have higher odds of inadequate nutrient intakes than those from higher household income. Lower household income status was significantly related to increased risk of inadequate protein (P for trend = 0.021), thiamin (P for trend = 0.018), and vitamin C (P for trend = 0.001) intakes. Logistic regression model adjusted for sex, age, and region shows similar risk estimation as the unadjusted model (data not shown). After controlling for energy intake, significance of risk for inadequate protein intake disappeared while those for thiamin (P for trend = 0.032) and vitamin C (P for trend = 0.002) remained.
There are avoidable differences in health status that are mostly due to living and working conditions, and inequalities cause prominent differences in quality of life among people. Therefore, the WHO commission on social determinants of health has recommended several principles to close the health gap within this generation, one of which is to improve daily living conditions from early life since experiences in early childhood lay foundations for health in later life [16]. The current study examined the effects of dietary intake on growth status by income level, a social determinant of health. Study results show that energy intake determined linear growth, and thin children had lower intakes of micronutrients such as vitamin C. Children from lower income households had higher risks of inadequate intake of micronutrients and overweight tendency.
In early childhood, adequate energy and nutrient intakes result in healthy growth and development of the brain, bones, and immune system. Traditional studies on malnutrition of children have focused on extreme cases, but mild malnutrition also deserves attention. If inadequate intake is not temporary but prolonged, then it may lead to poor physical and intellectual development [17].
Furthermore, many studies have showed that episodes of hunger and food insecurity, which are important causes of malnutrition, are associated with risk of overweight or obesity as well as stunting or wasting [181920], which is known as the double burden of malnutrition. The reasons have been explained by metabolic changes from chronic under-nutrition such as higher susceptibility to lower fat oxidation, higher central fat, and higher body fat gain [21]. Another explanation could be that hunger, which is a stressor, make one eat uninhibitedly or excessively to cope with stress [2223]. Further, those who are often hungry may purchase cheap and high energy-dense foods due to their limited economic resources, resulting in weight gain [424].
At the national level, double nutritional burden weighs heavily on middle income countries under rapid nutrition transition. While underweight remains a major nutritional and health problem, the burden of overweight is emerging in these countries [25]. Further, the double burden phenomenon is more apparent in populations of low socioeconomic status in industrialized countries [262728]. Many studies have showed that children in lower socioeconomic households consume more unhealthy foods [12293031], and this disparity among socioeconomic groups could widen the gap in health outcomes such as obesity [30].
Interestingly, the double burden is observed at an individual level. Stunting and obesity may coexist within a person in different stages of life (i.e. stunting in early life has been observed to be associated with obesity in later life.) [28] Several studies have suggested that risk of obesity in childhood according to socioeconomic status increases the risk of adolescent overweight and obesity and cannot be modified by socioeconomic status acquired in adulthood [323334]. The more prevalent type of double burden is overweight accompanied by under-nutrition of micronutrients, which is of concern since micronutrient deficiencies increase risk of chronic diseases [35].
Recently, problems associated with malnutrition have increased in Korea. Children from households of low economic status or food insecurity are more likely to consume unhealthy foods [12] and be overweight [1314]. Therefore, in future research, understanding the mechanism of their malnutrition with persistent monitoring of development outcomes for children, especially those in lower income households, is necessary to prevent further increases in health inequalities through nutritional disparity among different socioeconomic status groups.
There were several limitations in this study. First, this study used data from the KNHANES with one-day dietary intake. Thus, dietary intake data could not represent usual intakes and may actually misclassify the nutritional status of the subject. Although misclassification of the subject might weaken any association, it might not distort the direction of the association. Second, a causal relationship could not be established due to the nature of the cross-sectional study design of the KNHANES. Further, the observed associations may not be free from counter causality. Third, associations of socioeconomic status with nutritional status or growth were tested independently but did not guarantee nutritional status of the association between socioeconomic status and growth.
Nevertheless, to the best of our knowledge, this is the first study that evaluates the associations among socioeconomic status, nutritional status, and growth among Korean toddlers and preschoolers using population level data. The current study confirms that nutritional and health disparities exist in younger children and suggests that collective actions in public sector are required from early life in order to address health inequities beyond inequalities. Study results will shed light on intervention strategies to advocate healthy growth for children in all socioeconomic groups.
Figures and Tables
Table 2
Nutrient intakes according to growth status among children subjects aged 1 to 5 years (n = 1,687)1)

Table 3
Association of household income with unfavorable growth status among children aged 1 to 5 years (n = 1,687)1)

Notes
The present study was supported by the basic science research program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (No. 2013R1A1A1060704). The funder had no role in the design or analysis of the study or in the writing of this article.
References
1. World Health Organization (CH). Physical Status: the Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. Technical Report Series No. 854. Geneva: World Health Organization;1995.
2. WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006; 450:76–85.
3. Administrative Committee on Coordination/Subcommittee on Nutrition (CH). Ending Malnutrition by 2020: an Agenda for Change in the Millennium. Final Report to the ACC/SCN by the Commission on the Nutrition Challenges of the 21st Century. Geneva: Administrative Committee on Coordination/Subcommittee on Nutrition;2000.
4. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004; 79:6–16.

5. Food and Agriculture Organization of the United Nations (IT). The Double Burden of Malnutrition: Case Studies from Six Developing Countries. FAO Food and Nutrition Paper 84. Rome: Food and Agriculture Organization of the United Nations;2006.
6. Corvalán C, Kain J, Weisstaub G, Uauy R. Impact of growth patterns and early diet on obesity and cardiovascular risk factors in young children from developing countries. Proc Nutr Soc. 2009; 68:327–337.

7. Rolland-Cachera MF, Deheeger M, Maillot M, Bellisle F. Early adiposity rebound: causes and consequences for obesity in children and adults. Int J Obes (Lond). 2006; 30:Suppl 4. S11–S17.

8. Souganidis E. The importance of early nutritional intervention. How maternal and child undernutrition in early life can affect health in later years. Sight Life. 2011; 25:30–36.
9. Fernald LC, Neufeld LM. Overweight with concurrent stunting in very young children from rural Mexico: prevalence and associated factors. Eur J Clin Nutr. 2007; 61:623–632.

10. Popkin BM, Richards MK, Montiero CA. Stunting is associated with overweight in children of four nations that are undergoing the nutrition transition. J Nutr. 1996; 126:3009–3016.

11. Sawaya AL, Dallal G, Solymos G, de Sousa MH, Ventura ML, Roberts SB, Sigulem DM. Obesity and malnutrition in a Shantytown population in the city of São Paulo, Brazil. Obes Res. 1995; 3:Suppl 2. 107s–115s.

12. Kim K, Park SM, Oh KW. The impact of nutritional policy on socioeconomic disparity in the unhealthy food intake among Korean adolescents. Appetite. 2013; 71:388–395.

13. Oh SY, Hong MJ. Food insecurity is associated with dietary intake and body size of Korean children from low-income families in urban areas. Eur J Clin Nutr. 2003; 57:1598–1604.

14. Kim HR, Lee SH, Choi JM, Oh YI. Children's Obesity and Underweight among Low Income Families in Korea: Status, Implications and Policy Options. Seoul: Korea Institute for Health and Social Affairs;2011.
15. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea national health and nutrition examination survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.

16. World Health Organization (CH), Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Commission on Social Determinants of Health Final Report. Geneva: World Health Organization;2008.
17. Sandjaja , Poh BK, Rojroonwasinkul N, Le Nyugen BK, Budiman B, Ng LO, Soonthorndhada K, Xuyen HT, Deurenberg P, Parikh P. SEANUTS Study Group. Relationship between anthropometric indicators and cognitive performance in Southeast Asian school-aged children. Br J Nutr. 2013; 110:Suppl 3. S57–S64.

18. Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007; 107:1952–1961.

19. Kim K, Kim MK, Shin YJ. The concept and measurement of food security. J Prev Med Public Health. 2008; 41:387–396.

20. Larson NI, Story MT. Food insecurity and weight status among U.S. children and families: a review of the literature. Am J Prev Med. 2011; 40:166–173.
21. Sawaya AL, Martins PA, Grillo LP, Florêncio TT. Long-term effects of early malnutrition on body weight regulation. Nutr Rev. 2004; 62:S127–S133.

22. Frongillo EA. Understanding obesity and program participation in the context of poverty and food insecurity. J Nutr. 2003; 133:2117–2118.

23. Laitinen J, Ek E, Sovio U. Stress-related eating and drinking behavior and body mass index and predictors of this behavior. Prev Med. 2002; 34:29–39.

25. Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007; 370:1929–1938.

26. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, Uauy R. Maternal and Child Nutrition Study Group. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013; 382:427–451.

27. Pomeroy E, Stock JT, Stanojevic S, Miranda JJ, Cole TJ, Wells JC. Stunting, adiposity, and the individual-level "dual burden" among urban lowland and rural highland Peruvian children. Am J Hum Biol. 2014; 26:481–490.

28. Sawaya AL, Martins P, Hoffman D, Roberts SB. The link between childhood undernutrition and risk of chronic diseases in adulthood: a case study of Brazil. Nutr Rev. 2003; 61:168–175.

29. Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008; 87:1107–1117.

30. James WP, Nelson M, Ralph A, Leather S. Socioeconomic determinants of health. The contribution of nutrition to inequalities in health. BMJ. 1997; 314:1545–1549.

31. Vereecken CA, Inchley J, Subramanian SV, Hublet A, Maes L. The relative influence of individual and contextual socio-economic status on consumption of fruit and soft drinks among adolescents in Europe. Eur J Public Health. 2005; 15:224–232.

32. Demment MM, Haas JD, Olson CM. Changes in family income status and the development of overweight and obesity from 2 to 15 years: a longitudinal study. BMC Public Health. 2014; 14:417.
33. Power C, Manor O, Matthews S. Child to adult socioeconomic conditions and obesity in a national cohort. Int J Obes Relat Metab Disord. 2003; 27:1081–1086.

34. Poulton R, Caspi A, Milne BJ, Thomson WM, Taylor A, Sears MR, Moffitt TE. Association between children's experience of socioeconomic disadvantage and adult health: a life-course study. Lancet. 2002; 360:1640–1645.

35. Delisle HF. Poverty: the double burden of malnutrition in mothers and the intergenerational impact. Ann N Y Acad Sci. 2008; 1136:172–184.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download