Abstract
Purpose
This study was designed to determine whether men who engaged in recreational bicycle riding are more likely to be affected by lower urinary tract symptoms (LUTS) and sexual dysfunction than are man who exercised by amateur marathon running with less perineal impact.
Materials and Methods
A total of 22 healthy male amateur bicyclists and 17 healthy male amateur marathoners were enrolled in the study. We evaluated questionnaires including the International Prostate Symptom Score (IPSS) and the International Index of Erectile Function (IIEF), serum prostate-specific antigen (PSA), uroflowmetric values, postvoid residual (PVR) urine volume, and transrectal ultrasound of the prostate in all subjects. We also compared the prevalence of urination disorders (UD) and erectile dysfunction (ED).
Results
There were no significant differences between the two groups in age, body mass index, comorbidities, or exercise habits (p>0.05). Mean total and subscale scores of the IPSS and IIEF and the prevalence of UD (8/22 vs. 4/17, p=0.494) and ED (11/22 vs. 10/17, p=0.748) were not significantly different between the two groups. Also, there were no significant differences between the two groups in uroflowmetric parameters such as peak urinary flow rates, voided urine volume, PVR urine volume, prostate volume, or serum PSA level.
Bicycle riding is popular throughout the world for transportation, recreation, sports, and health-related benefits. There are 54,575,000 recreational cyclists in the United States [1]. Of these cyclists, 53% are men. In Korea, according to the needs of the times, such as economic development and increased leisure time, a trend for preferring environmentally friendly sports, and growing interest in health and well-being, the awareness of cycling as a leisure sport has recently increased. There were 24,406 recreational bicycle riders in 911 bicycle clubs in Korea as of January 2010 [2].
Bicycling is an ideal form of aerobic, nonimpact exercise with established protective cardiovascular effects and a beneficial influence on the risk of hypertension, diabetes, and stroke [3]. Although there are controversies about changes to the genitourinary system in subjects who cycle, bicycle riding has been known as a common source of acute traumatic injuries as well as overuse injuries [4-6]. Bicycling studies suggest perineal trauma, pressure, or both may have a role in these genitourinary hazards. Many of them directly affect the genitourinary tract, causing genital numbness, erectile dysfunction (ED), priapism, infertility, hematuria, and effects on serum prostate-specific antigen (PSA) levels [4,5].
Many healthy recreational bicycle riders have questioned urologists about the relationship between bicycle riding and prostate-related lower urinary tract symptoms (LUTS). But to the best of our knowledge, there has been no study of LUTS in male recreational bicyclists. With this study, our goal was to evaluate the impact of bicycle riding on LUTS and sexual dysfunction in men with the use of amateur marathoners as a control group of physically equivalent individuals with a low level of perineal pressure or trauma.
A total of 22 healthy male amateur bicycle riders from two bicycling clubs in Jeonju, Korea, were studied. The recruitment criteria were age between 40 and 50, bicycling period of more than 1 year before the study, three or more times of cycling per week, and 30 minutes or more of cycling duration per time. The controls were 17 healthy male marathoners from an amateur marathon club in Jeonju, Korea. They were matched with equivalent recruitment criteria. Before the study, all subjects were informed about the experimental procedures, which were in accordance with the ethical standards of Chonbuk National University Hospital, and were required to give written informed consent.
The evaluation contained a study questionnaire assessing sports participation habits, urological and medical history, the International Prostate Symptom Score (IPSS), the International Index of Erectile Function (IIEF), the International Continence Society (ICS) Male Questionnaire-Short form, the Overactive Bladder Symptom Score (OABSS), and the Premature Ejaculation Diagnostic Tool (PEDT). An IPSS of more than 7 defined the voiding dysfunction (VD) group, and erectile ED was defined as a score of 21 or less on the IIEF-5, an abridged 5-item version of the IIEF-15, which ensured identification of the mildest forms of ED.
Furthermore, we examined serum total prostate-specific antigen (tPSA), free prostate-specific antigen (fPSA), uroflowmetric values, postvoid residual (PVR) urine volume, and transrectal ultrasound (TRUS, B&K Medical, Herlev, Denmark) of the prostate in all subjects.
We analyzed the data with SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). To test differences between the two groups in serum tPSA, fPSA, uroflowmetric values, PVR urine volume, calculated volume of the prostate using TRUS, and the total or subscale score of each questionnaire, we used independent-sample t-tests with statistical significance as p<0.05. Also, we compared the two groups for the prevalence of VD and ED by using the chi-square or Fisher's exact tests with statistical significance as p<0.05.
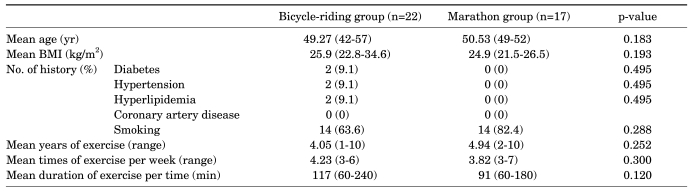
A total of 22 recreational bicyclists ranging in age from 42 to 57 years completed the questionnaires and were included in the assessment. The riders had cycled for a period of 1 to 10 years (range, 4.05±2.04 years), 3 to 6 times per a week (range, 4.23±1.19 times), and with 60 to 240 minutes of cycling duration per time (range, 91±59 minutes). The subjects' body mass index (BMI) ranged from 22.8 to 34.6 kg/m2 (range, 25.9±2.67 kg/m2). There were no significant differences between the two groups in age, BMI, comorbidities, or exercise habits (Table 1).
The results of the questionnaires are shown in Table 2. There were no significant differences in the total and subscale scores of the IPSS between the two groups. The prevalence of VD on the basis of the IPSS was not significantly different between the two groups (8/22 vs. 4/17, p=0.494). There were no significant differences in total and subscale scores of the IIEF between the two groups. The prevalence of ED based on the IIEF was not significantly different between the two groups (11/22 vs. 10/17, p=0.748). Also, we found no statistical differences in other questionnaires such as the OABSS, ICS male Questionnaire-Short form, and PEDT (Table 2).
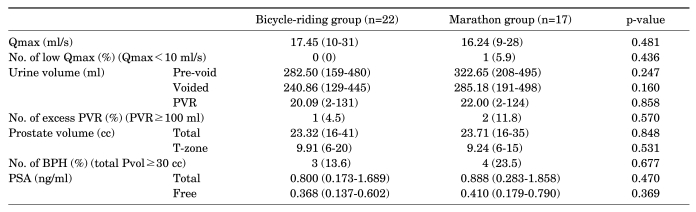
As shown in Table 3, there were no significant differences between the two groups regarding uroflowmetric parameters such as peak urinary flow rate (Qmax), voided urine volume, or PVR urine volume. In all subjects, prevoid urine volume was at least 150 ml and voided urine volume was at least 125 ml. In the cyclists, the mean calculated volume of the prostate by TRUS was 23.32 cc and there was no statistically significant difference between the two groups (23.32 vs. 23.71, p=0.848). Also, the serum tPSA level was within the normal range in all subjects and there was no significant difference between the two groups (0.800 vs. 0.888, p=0.470). The prevalence of a significantly low Qmax, excess PVR, or benign prostatic hyperplasia was not significantly different between the two groups (Table 3).
The reported incidence of bicycling-related urogenital symptoms varies considerably. The most common bicycling-associated urogenital problems are nerve entrapment syndromes presenting as genitalia numbness, which was reported in 50% to 90% of cyclists, followed by erectile dysfunction in 13% to 24%. Other less common symptoms include priapism, penile thrombosis, infertility, hematuria, torsion of the spermatic cord, prostatitis, perineal nodular induration, and elevated PSA, which are reported only sporadically [4]. Bicycle riding is used throughout the world for well-known exercise, fitness, and recreational benefits. As such, it is not surprising that these statements have created much controversy. In our study population, we investigated in particular the relationship between bicycle riding and LUTS or sexual dysfunction by use of questionnaires; thus, we did not ask the study group about complications such as genitalia numbness.
To date there have been no studies about LUTS in male recreational bicyclists. Recently, Saka et al reported that bicycle riding has no impact on serum PSA levels and urinary flow parameters [7]. The goal of their study was to investigate whether professional bicycle riding altered plasma concentration of tPSA, fPSA, percent free PSA (f/t PSA), and urinary flow parameters in healthy men.
We present a cross-sectional study of the effects of bicycle riding, a sport with perineal impact, on genitourinary function in men. In our study, the subjects were amateur recreational bicycle riders from clubs, and we aimed to find any hazards of bicycle riding in male LUTS or sexual dysfunction. Our hypothesis was that if bicycle riding had any impact on the genitourinary tract there would be significant differences in genitourinary functional parameters between a regular long-term bicycle-riding group and control group of physically equivalent individuals with a low level of perineal pressure or trauma, such as a regular long-term marathon running group. However, there were no significant differences between the two groups regarding the questionnaires, uroflowmetric parameters, PVR urine volume, prostate volume, or serum PSA level. Thus, we found the inverse of our hypothesis: that bicycle riding may have no hazardous impact on genitourinary health in recreational male bicycle riders.
The prevalence of LUTS or VD as defined by an IPSS of ≥8 was not significantly different between the two groups. Physical activity has been documented to be protective against LUTS in previous studies [8], and the perineal impact of bicycle riding does not seem to offset that effect. Many of the bicyclists enrolled were very energetic and confident of their health, and there were no significant differences in the uroflowmetric analysis results, TRUS-measured prostate volume, or serum PSA level. We assess this point in context as follows. Bicycle-riding-induced perineal impacts do not have enough influence on the prostate mechanically or physiologically. Previous reports about the effect of bicycling on serum PSA concentrations were not conclusive, but in recent studies the dominant finding was that there was no statistically or clinically significant change in PSA levels regardless of cycling [7-12]. No other published data have compared questionnaires evaluating LUTS, uroflowmetric analysis results, or TRUS-measured prostate volume of regular long-term amateur bicycle riders with a control group of physically equivalent individuals with a low level of perineal pressure or trauma such as a regular long-term runner group. Our study is important in terms of shedding light on this subject.
Bicycle riding was not associated with an increased incidence of sexual dysfunction in men. Previous studies have reported an association between bicycling and sexual dysfunction, but those studies were based on biological measurements such as penile blood flow [13], focused on sexual dysfunction after prolonged exposure to perineal impact [14], or suggested a trend but no strong association [15]. The results of our study support the observation of others that bicycle riding has no effect on LUTS and male sexual function [16].
Our study had some limitations. First, the cross-sectional study structure may have affected the validity of the results. We did not collect baseline data about LUTS and sexual dysfunction parameters before activity from either group. We implemented a cross-sectional study design as an efficient and cost-effective investigation to perform a preliminary exploration for an association with the potential to generate additional hypotheses for more structured research. Second, the small number of subjects may have introduced some selection bias into the results. However, we suspect that the influence of the bias may be weak because almost all of the 5th and 6th decades of each club participated in our study. We plan to do vertical, annual follow-up studies of the subjects.
The fact that the results of our study are consistent with data from other studies in similar sports supports the validity of our results and decreases the chance of systemic errors. More assessment of the effect of bicycle riding on the human pelvic anatomy and genitourinary complaints is warranted to further validate the results of this study.
Concern about bicycle riding as a leisure sport has recently increased as many urological outpatients and healthy recreational bicyclists have questioned urologists about the relationship between bicycle riding and prostate-related LUTS and sexual dysfunction. In our opinion, bicycle riding seems to have no statistically measurable effect on LUTS or sexual functioning in men, at least in amateur recreational bicyclists. There is a need for further large-scale research on this subject and study of the underlying mechanisms leading to cycling-related LUTS and sexual dysfunction. We plan to carry out vertical, annual follow-up of our subjects.
Notes
References
1. 1999 Superstudy of Sports Participation. America Sports Data, Inc.
2. Korea Council of Sport for All: registration state of amateur sports club at January, 2010 [Internet]. c1998-2010. cited 2010 Feb 24. Seoul: Korea Council of Sport for All;Available from: http://www.sportal.or.kr.
3. Hillman M. Cycling offers important health benefits and should be encouraged. BMJ. 1997; 315:490. PMID: 9284687.

4. Leibovitch I, Mor Y. The vicious cycling: bicycling related urogenital disorders. Eur Urol. 2005; 47:277–286. PMID: 15716187.

5. Seo HS, Lee NK. Predictors of PSA screening among men over 40 years of age who had ever heard about PSA. Korean J Urol. 2010; 51:391–397. PMID: 20577605.

6. Han MC, Kim JS, Shim BS. Analysis of the risk factors related to progression of chronic prostatitis. Korean J Urol. 2005; 46:1040–1045.
7. Saka T, Sofikerim M, Demirtas A, Kulaksizoglu S, Caniklioglu M, Karacagil M. Rigorous bicycling does not increase serum levels of total and free prostate-specific antigen (PSA), the free/total PSA ratio, gonadotropin levels, or uroflowmetric parameters. Urology. 2009; 74:1325–1330. PMID: 19781750.

8. Orsini N, RashidKhani B, Andersson SO, Karlberg L, Johansson JE, Wolk A. Long-term physical activity and lower urinary tract symptoms in men. J Urol. 2006; 176:2546–2550. PMID: 17085155.

9. Crawford ED 3rd, Mackenzie SH, Safford HR, Capriola M. The effect of bicycle riding on serum prostate specific antigen levels. J Urol. 1996; 156:103–105. PMID: 8648767.
10. Luboldt HJ, Peck KD, Oberpenning F, Schmid HP, Semjonow A. Bicycle riding has no important impact on total and free prostate-specific antigen serum levels in older men. Urology. 2003; 61:1177–1180. PMID: 12809893.

11. Herrmann M, Scharhag J, Sand-Hill M, Kindermann W, Herrmann W. Long-distance mountain biking does not disturb the measurement of total, free or complexed prostate-specific antigen in healthy men. Clin Chem Lab Med. 2004; 42:347–349. PMID: 15080570.

12. Lippi G, Corgnati A, Salvagno G, Schena F, Franchini M, Guidi G. Total and free PSA serum concentrations are not influenced by extensive physical exercise and bicycle riding. Int J Sports Med. 2005; 26:79–81. PMID: 15643540.

13. Sommer F, Schwarzer U, Klotz T, Caspers HP, Haupt G, Engelmann U. Erectile dysfunction in cyclists. Is there any difference in penile blood flow during cycling in an upright versus a reclining position? Eur Urol. 2001; 39:720–723. PMID: 11464064.
14. Andersen KV, Bovim G. Impotence and nerve entrapment in long distance amateur cyclists. Acta Neurol Scand. 1997; 95:233–240. PMID: 9150814.

15. Marceau L, Kleinman K, Goldstein I, McKinlay J. Does bicycling contribute to the risk of erectile dysfunction? Results from the Massachusetts Male Aging Study (MMAS). Int J Impot Res. 2001; 13:298–302. PMID: 11890518.

16. Taylor JA 3rd, Kao TC, Albertsen PC, Shabsigh R. Bicycle riding and its relationship to the development of erectile dysfunction. J Urol. 2004; 172:1028–1031. PMID: 15311030.

TABLE 2
Comparison of results of questionnaires between the two groups
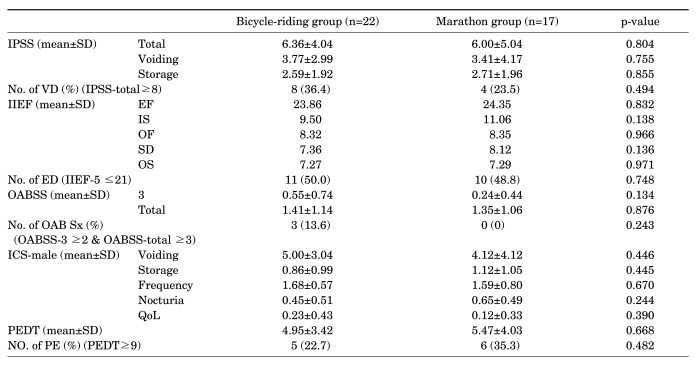
IPSS: International Prostate Symptom Score, IIEF: International Index of Erectile Function, EF: erectile domain, IS: intercourse satisfaction, OF: orgasm function, SD: sexual desire, OS: overall satisfaction, ED: erectile dysfunction, OABSS: Overactive Bladder Symptom Score, ICS: International Continence Society, QoL: quality of life, PEDT: Premature Ejaculation Diagnostic Tool, PE: premature ejaculation




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download