Abstract
Purpose
We aimed to determine the treatment of choice criteria for benign prostatic hyperplasia (BPH) by analyzing the factors causing alpha-adrenergic receptor blocker (α-blocker) monotherapy failure.
Materials and Methods
This retrospective study enrolled 129 patients with BPH who were prescribed an α-blocker. Patients were allocated to a transurethral resection of prostate (TURP) group (after having at least a 6-month duration of medication) and an α-blocker group. We compared the differences between the two groups for their initial prostate volume, serum prostate-specific antigen (PSA), maximum urinary flow rate (Qmax), International Prostate Symptom Score (IPSS), and postvoid residual urine volume (PVR).
Results
Of the 129 patients, 54 were in the TURP group and 75 were in the α-blocker group. Statistically significant differences (p<0.05) between the two groups were found in the prostate volume (50.8 ml vs. 34.4 ml), PSA (6.8 ng/ml vs. 3.6 ng/ml), Qmax (6.84 ml/sec vs. 9.99 ml/sec), and IPSS (27.3 vs. 16.8). According to the multiple regression analysis, the significant factors in α-blocker monotherapy failure were the IPSS (p<0.001) and prostate volume (p=0.015). According to the receiver operating characteristic (ROC) curve-based prediction regarding surgical treatment, the best cutoff value for the prostate volume and IPSS were 35.65 ml (sensitivity 0.722, specificity 0.667) and 23.5 (sensitivity 0.852, specificity 0.840), respectively.
Benign prostatic hyperplasia (BPH) is the most prevalent of all conditions in aging men with a population prevalence in the 40 to 79-year age group ranging from 14% to 56% in different countries [1]. BPH can be a progressive disease and may progress to acute urinary retention (AUR) and BPH-related surgery [2]. Men with BPH commonly present with lower urinary tract symptoms that affect their quality of life and interfere with their activities of daily living. Both surgical and medical modalities are available for the treatment of BPH. Recently, alpha-adrenergic receptor blockers (α-blockers) and/or 5-alpha-reductase inhibitors (5-ARIs) have been mainly used for the medical treatment of BPH. However, controversy still exists regarding the choice of either medication, that is, α-blocker monotherapy or combined α-blocker and 5-ARI, or surgery as an initial treatment.
We analyzed the risk factors of medication failure in BPH patients who underwent a surgical procedure, particularly the transurethral resection of the prostate (TURP), because of subjective patient symptom aggravation and AUR after a course of at least 6 months of α-blocker monotherapy.
We retrospectively analyzed the data of 129 BPH patients who were treated with α-blockers in our department between January 2008 and May 2009. Patients were treated with α-blockers for at least 6 months. Patients with neurologic disorders, recurrent urinary tract infections, renal impairment, bladder stones, or bladder cancer were excluded. A transrectal prostate biopsy was performed on all patients with a PSA level ≥4 ng/ml and patients with prostate cancer were excluded. On the first visit to our department, we measured the prostate volume, serum prostate-specific antigen (PSA), maximum urinary flow rate (Qmax), International Prostate Symptom Score (IPSS), and postvoid residual urine volume (PVR) of each patient.
Patients were divided into two groups: the TURP group and α-blocker group. In the TURP group, TURP was performed after undergoing a minimum 6 month course of α-blocker medication because of subjective patient symptom aggravation or AUR. In the α-blocker group, only an α-blocker was prescribed for a minimum of 6 months for BPH.
We looked for factors that led to surgical treatment of BPH by comparing the differences between the TURP group and α-blocker group in regards to their initial prostate volume, PSA, Qmax, IPSS, and PVR. The cutoff value of individual factors was calculated using a receiver operating characteristic (ROC) curve.
Transrectal ultrasonography (TRUS) was performed to calculate the prostate volume. The maximal length, width, and height of the prostate were measured and an integrated volumetric program automatically calculated the volume using the formula: volume=width × length × height × 0.5236. Qmax was measured with a flowmeter. Each eligible patient was asked to fill out a self-evaluating IPSS questionnaire. PVR was measured using a diagnostic ultrasound bladder scan.
An independent t-test, ROC curve, and multiple regression analysis were used in statistical analysis with SPSS 12.0 for Windows. A p-value<0.05 indicated statistical significance.
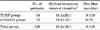
Of 129 patients, 54 were in the TURP group and 75 were in the α-blocker group. The average medication period was 19.1 months (range, 6-118 months) and 14.6 months (range, 6-78 months) for the TURP and α-blocker groups, respectively (Table 1). The mean patient age was 68.7 years (range, 61-79 years) and 66.9 years (range, 60-79 years), respectively (p>0.05) (Table 2). Of the TURP group patients, 32 developed AUR and 22 had aggravation of other subjective urinary symptoms (frequency, urgency, hesitancy, weak stream, etc.).
Statistically significant differences were found in the prostate volume (50.8α26.0 ml vs. 34.4α12.1 ml), PSA (6.8α9.4 ng/ml vs. 3.6α5.1 ng/ml), Qmax (6.84α3.50 ml/sec vs. 9.99α4.65 ml/sec), and IPSS (27.3α6.1 vs. 16.8α7.2) between the TURP and α-blocker groups (p<0.05). However, significant differences were not found in PVR (56.9α37.0 ml vs. 49.3α36.5 ml, p=0.243) (Table 2).
According to the ROC curve, the significant factor in α-blocker monotherapy failure was the IPSS (area under the curve (AUC)=0.864, asymptotic 95% confidence interval, 0.797-0.931). The TRUS (AUC=0.736, asymptotic 95% confidence interval, 0.649-0.823) and PSA (AUC=0.663, asymptotic 95% confidence interval, 0.569-0.756) followed. However, the Qmax was not the significant factor in α-blocker monotherapy failure (AUC<0.5, asymptotic 95% confidence interval, 0.194-0.371) (Fig. 1).
According to the multiple regression analysis, the most significant factor in α-blocker monotherapy failure was the IPSS (p<0.001). The TRUS (p=0.015, multiple regression analysis) followed. However, the PSA and Qmax were not significant factors in α-blocker monotherapy failure (p>0.05) (Table 2).
The best cutoff value for the prostate volume and IPSS were 35.65 ml (sensitivity 0.722, specificity 0.667) and 23.5 (sensitivity 0.852, specificity 0.840), respectively (Fig. 1).
BPH is the most common benign tumor in males. BPH treatment is divided into two categories, medical treatment and surgical treatment. Nowadays, medical treatment is the first line therapy in BPH and has been increasing steadily because surgical treatment has the risk of operative and postoperative complications.
The European Association of Urology (EAU) guidelines include α-blockers as a treatment option for BPH where lower urinary tract symptoms (LUTS) are bothersome and there is no absolute indication for surgery [3]. The α-blockers, the most common BPH treatment medications, improved the total symptom score on average by 30% to 45% and the Qmax by approximately 15% to 30% [4].
Treatment with an α-blocker has not been shown to reduce the overall long-term risk of AUR or BPH-related surgery [5,6]. In the Medical Therapy of Prostatic Symptoms (MTOPS) study, doxazosin delayed the time to AUR but did not significantly reduce the cumulative incidence at 4 years compared with the placebo [5]. Similarly, doxazosin did not significantly reduce the cumulative incidence of invasive therapy [5]. In the Alfuzosin Long-Term Efficacy and Safety Study, alfuzosin did not reduce the risk of AUR compared with the placebo. Although a trend towards a lower incidence of BPH-related surgery was seen in the alfuzosin group, this did not reach statistical significance when compared with the placebo group [6]. Because medication with an α-blocker did not reduce the incidence of BPH-related surgery, criteria for surgical treatment as an initial treatment for BPH is needed.
The results of a community-based study in which 492 men between 40 and 79 years underwent periodic urinary flow rate measurement over 6 years demonstrated that the peak urinary flow rate deteriorates by 2.1% per year and that this rate of deterioration is higher with increasing age, poor initial flow, larger prostate volume, and symptom severity [7]. In the same study population, Jacobsen et al demonstrated that the risk of AUR increases with the presence of lower urinary tract symptoms, depressed peak urinary flow rates, enlarged prostates, and older age [8]. In a sub-analysis of the Proscar Long-Term Effectiveness and Safety Study (PLESS), Roehrborn et al reported that baseline serum PSA and prostate volume predict BPH-related surgery and/or AUR [9]. Marberger et al also demonstrated that the 2-year incidence of AUR is approximately three-fold in men with a prostate volume of equal to or greater than 40 ml compared to those with a volume less than 40 ml [10]. These results confirm that BPH is a progressive disease and that the rate of progression is higher with worse baseline parameters. In our study, among various baseline parameters, IPSS and prostate volume were found to be predictive of future surgery. Our results are thus in line with previous observations that poor baseline parameters are risk factors for AUR or future surgery.
Crawford et al suggested that baseline prostate volume, PSA, Qmax, PVR, and age were important predictors of the risk of clinical progression of BPH, and that men with a baseline prostate volume of 31 ml or greater, PSA 1.6 ng/dl or greater, Qmax less than 10.6 ml/sec, PVR 39 ml or greater, or age 62 years or older had a significantly increased risk of clinical progression of BPH [11].
Hong et al reported that 100 of 437 patients converted to surgical treatment following long-term medication, that IPSS and prostate volume were the best predictive baseline parameters for predicting the outcome of medical treatment, and that based on the ROC curve, cutoff values of 21 and 32 ml for predicting the failure of medical treatment were presented for IPSS and prostate volume, respectively [12].
Lee et al showed that BPH patients with severe IPSS (≥17) and a larger prostate volume (>40 ml) had a higher risk of surgical intervention, and this suggested that, at the initial visit, the IPSS and prostate volume might be useful predictors of the eventual need for surgical intervention [13].
In our report, BPH patients on whom surgical treatments were performed following a minimum of 6 months of medical treatment were different from BPH patients with medical treatment alone. We did not analyze the AUR in our data, but we could predict the risk of AUR with prostate volume, Qmax, IPSS, and PVR. We suggest that the predictive factors of surgical treatment in BPH are the prostate volume and IPSS. Based on the ROC curve, cutoff values of 35 ml and 23 for predicting the failure of medical treatment were found for prostate volume and IPSS, respectively.
Current EAU guidelines for the management of BPH recommend 5ARIs for the treatment of bothersome LUTS in men with a prostate volume >30-40 ml, when there is no absolute indication for surgery [3]. Others have proposed that 5ARIs should be considered as a first line medical treatment in men with symptomatic, progressive BPH as indicated by a prostate volume ≥30 ml and/or PSA≥1.5 ng/ml [14]. In a meta-analysis by Boyle et al, finasteride was the most effective in men with a larger prostate (statistically significant difference in improvement of symptoms at the cutoff value of 40 ml) [15]. In our report, only an α-blocker was prescribed for BPH; therefore, a study of combination treatment with 5ARIs is needed.
Figures and Tables
FIG. 1
Receiver operation characteristics of each parameter. TRUS: transrectal ultrasonography (prostate volume), PSA: prostate-specific antigen, Qmax: maximum urinary flow rate, IPSS: International Prostate Symptom Score.
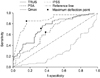
TABLE 2
Baseline clinical characteristics of each group

Values are MeanαSD (SD: standard deviation). TURP: transurethral resection of prostate, α-blocker: alpha-adrenergic receptor blocker, PSA: prostate-specific antigen, Qmax: maximum urinary flow rate, IPSS: International Prostate Symptom Score, PVR: postvoid residual urine volume, a: comparison by independent t-test between TURP group and α-blocker group, b: comparison by multiple regression analysis between TURP group and α-blocker group
References
1. Djavan B, Fong YK, Harik M, Milani S, Reissigl A, Chaudry A, et al. Longitudinal study of men with mild symptoms of bladder outlet obstruction treated with watchful waiting for four years. Urology. 2004. 64:1144–1148.
2. Kim CI, Chang HS, Kim BK, Park CH. Long-term results of medical treatment in benign prostatic hyperplasia. Urology. 2006. 68:1015–1019.
3. Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol. 2004. 46:547–554.
4. Djavan B, Chapple C, Milani S, Marberger M. State of the art on the efficacy and tolerability of alpha1-adrenoceptor antagonists in patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Urology. 2004. 64:1081–1088.
5. McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003. 349:2387–2398.
6. Roehrborn CG. Alfuzosin 10 mg once daily prevents overall clinical progression of benign prostatic hyperplasia but not acute urinary retention: results of a 2-year placebo-controlled study. BJU Int. 2006. 97:734–741.
7. Roberts RO, Jacobsen SJ, Jacobson DJ, Rhodes T, Girman CJ, Lieber MM. Longitudinal changes in peak urinary flow rates in a community based cohort. J Urol. 2000. 163:107–113.
8. Jacobsen SJ, Jacobson DJ, Girman CJ, Roberts RO, Rhodes T, Guess HA, et al. Natural history of prostatism: risk factors for acute urinary retention. J Urol. 1997. 158:481–487.
9. Roehrborn CG, McConnell JD, Lieber M, Kaplan S, Geller J, Malek GH, et al. PLESS Study Group. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. Urology. 1999. 53:473–480.
10. Marberger MJ, Andersen JT, Nickel JC, Malice MP, Gabriel M, Pappas F, et al. Prostate volume and serum prostate-specific antigen as predictors of acute urinary retention. Combined experience from three large multinational placebo-controlled trials. Eur Urol. 2000. 38:563–568.
11. Crawford ED, Wilson SS, McConnell JD, Slawin KM, Lieber MC, Smith JA, et al. Baseline factors as predictors of clinical progression of benign prostatic hyperplasia in men treated with placebo. J Urol. 2006. 175:1422–1426.
12. Hong SJ, Ko WJ, Kim SI, Chung BH. Identification of baseline clinical factors which predict medical treatment failure of benign prostatic hyperplasia: an observational cohort study. Eur Urol. 2003. 44:94–99.
13. Lee KS, Kim ME, Kim SJ, Kim HK, Kim HS, Kim CI, et al. Predictive factors of the long-term medical treatment failure in benign prostatic hyperplasia. Korean J Urol. 2008. 49:826–830.
14. Bartsch G, Fitzpatrick JM, Schalken JA, Isaacs J, Nordling J, Roehrborn CG. Consensus statement: the role of prostate-specific antigen in managing the patient with benign prostatic hyperplasia. BJU Int. 2004. 93:Suppl 1. 27–29.
15. Boyle P, Gould AL, Roehrborn CG. Prostate volume predicts outcome of treatment of benign prostatic hyperplasia with finasteride: meta-analysis of randomized clinical trials. Urology. 1996. 48:398–405.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download