Abstract
Purpose
Urosepsis is the most feared complication of transrectal prostate biopsy. The incidence may be increasing from <1% to 2%–3% in contemporary series. Historically, fluoroquinolones have been effective antibiotic prophylaxis to prevent infective complications but antibiotic resistance is increasing. The increase in antibiotic resistance may contribute to reported increases in urosepsis and hospitalization after transrectal biopsy. This article will review other methods clinicians may employ to reduce the incidence of infective complications after prostate biopsy.
Materials and Methods
A systematic review of the literature was conducted using literature databases PubMed and Ovid MEDLINE in August 2015 in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) criteria.
Results
Effective strategies to reduce infective complications after transrectal prostate biopsy include augmented prophylaxis with other antibiotics, rectal swab culture directed antibiotic prophylaxis or a transperineal biopsy approach. Needle disinfection, minimizing the number of biopsy needles and rectal disinfectants may also be of use. These methods may be of particular utility in patients with risk factors for developing urosepsis such as recent antibiotic use and overseas travel.
The most feared complication of transrectal prostate biopsy is urosepsis which may be increasing in frequency from <1% 2 decades ago to approximately 2%–3% in recent studies [123]. The predominant causative organism is Escherichia coli [2]. The mechanism for this complication is that the transrectal biopsy approach involves penetrating the rectal mucosa and subsequently risks inoculating prostatic tissue, which is quite vascular, with bowel flora.
Prostate biopsy is a common procedure with over 1 million biopsies performed per year in the United States [4]. Therefore, even a low rate of complications can cause harm to significant numbers of patients. The estimated economic impact of urosepsis post transrectal biopsy in England and Wales may be up to £11,000,000 annually [5].
The benefit of prophylactic antibiotics in reducing infection after prostate biopsy was definitively established by a Cochrane review [6]. However, the authors did not consider current concerns regarding fluoroquinolone resistance.
Up to one quarter of men undergoing prostate biopsy in recent series are colonized with rectal flora demonstrating fluoroquinolone resistance [78]. It appears that the number of biopsies is not associated with the development of resistance and that once resistance develops it tends to persist [7]. Fluoroquinolone resistance is a significant clinical concern as, in E. coli bacteraemia, fluoroquinolone resistance has been independently associated with mortality due to difficulties in initiating effective antibiotic therapy [9].
Well known risk factors for post transrectal biopsy urosepsis include recent hospitalization, recent antibiotic use—particularly fluoroquinolones, diabetes and recent overseas travel [12101112]
In the context of emerging fluoroquinolone resistance this paper will describe a number of possible interventions aimed at reducing infective complications after prostate biopsy.
A systematic review of the literature was undertaken to assess publications on prevention of sepsis af ter transrectal ultrasound (TRUS) biopsy, Fig. 1. The review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) criteria [13]. The Search was conducted using literature databases PubMed and Ovid MEDLINE using the terms "antibiotic," "prostatic neoplasms," "infection," "prophylaxis," "resistance" (and their MeSH terms, synonyms) related to "cancer" in August 2015. Other search terms used to identify particular techniques included "rectal preparation," "bowel preparation," "enema", "suppository," "rectal swab," "culture directed," "disposable," and "transperineal." The search was limited to English language articles considering humans published between January 2000 and August 2015. "Cascading" was used to identify references cited in these articles helped identify relevant and significant publications not previously included in the search. The results of key papers are summarised in Table 1.
A large study of 75,000 Canadian men reported rising rates of post biopsy infection requiring readmission in from 0.6% in 1996 to 3.6% in 2005 which was thought to be due to rising antibiotic resistance rates, particularly fluoroquinolone resistant E. coli [3]. The findings were supported by Carignan et al. [2] who described, from 2002 to 2011, increases in infective complications from 0.52% to 2.15% in conjunction with increases in the ciprofloxacin minimum inhibitory concentration (MIC) amongst those with infective complications. This suggests increasing ciprofloxacin resistance may be a contributing mechanism to the overall increase of infective complications.
Further, Carignan et al. [2] noted that the mean MIC of fluoroquinolone sensitive isolates increased across their study; such that, following a single dose, prostatic concentrations of ciprofloxacin may in many cases actually be below the MIC 24–48 hours after biopsy during which time the epithelial break has not been healed which implies a significant risk of infection [2]. However, we did not identify any recent studies demonstrating an advantage to multiple compared to single dosing regimens. A related point is that antibiotic prophylaxis administered too early before a procedure may be ineffective and that multiple doses of potentially unnecessary antibiotics increases concerns regarding the development of antibiotic resistance.
Another recent contributor to antibiotic resistance is the rising prevalence of the extended spectrum beta lactamase phenotype amongst Enterobacteriaciae such as E. coli and Klebsiella species which confers increased resistance to fluoroquinolones [14].
The Australian therapeutic guidelines currently recommend ciprofloxacin 500 mg per oral (PO) 60–120 minutes before a transrectal prostate biopsy [12]. A large multicentre study of 9,015 biopsies demonstrated an overall reduction of infective complications from 1.19% to 0.57% after the introduction of augmented prophylaxis with either gentamicin 120 mg or cefazolin 1- to 2-g intramuscular administered in addition to ciprofloxacin 500 mg PO 1 hour before and again the evening after the biopsy [15]. Batura et al. [16] demonstrated the addition of amikacin 1 g intravenous (IV) immediately before the procedure to their existing prophylactic antibiotic regime, which included 500 mg twice daily (BD) PO ciprofloxacin 2 days before through 5 days after and 500 mg per rectum metronidazole once after the procedure, significantly lowered infective complications decreased from 3.9% to 1.4% and the relative risk of bacteraemia decreased by 90% [16].
Rather than relying on empirical antibiotic prophylaxis, some advocate cultures f rom rectal swabs to direct specific antibiotic therapy if resistant organisms, such as fluoroquinolone resistant bacteria, are identified. A recent study of 487 patients reported that culture directed antibiotics based on the results of a rectal swab reduced infective complications from 2.9% to 1.9% compared to empirical prophylactic antibiotic therapy [8]. A recent North American study reported a significant reduction in hospitalization of 1.19% to 0.47% after the addition of culture directed antibiotic prophylaxis compared to their historical practice of empirical antibiotic prophylaxis [15]. Taylor et al. [17] used a ciprofloxacin based culture method to assess for fluoroquinolone resistance in rectal swabs. They found ciprofloxacin resistance in 20% of patients. In their study of 457 men they found that targeted antimicrobial prophylaxis reduced infective complications such that 38 rectal swabs would preclude 1 infective complication. However, their results were not statistically significant. They calculated a saving in favour of targeted biopsy of $4,449 for each infective complication averted [17]. The authors of each of these studies suggested that rectal swab culture directed antibiotic prophylaxis may be a cost effective manner to manage the issue of increasing fluoroquinolone resistance. Qi et al. [18] investigated the mechanisms for antibiotic resistance in rectal swabs and found it results from a heterogeneous group of phenotypes which supports the use of culture directed antibiotic prophylaxis rather than extended generic antibiotic prophylaxis. The main limitation of rectal swab cultures is that they must be taken 24–48 hours prior to the biopsy which complicates practicalities [17].
The 2011 Cochrane review evaluated the utility of a disinfectant enema. No differences were found in a direct comparison of prophylactic antibiotics and disinfectant enemas. Two studies considered the addition of a disinfectant enema to antibiotics and found it may reduce the incidence of bacteraemia compared to antibiotics alone [6].
Park et al. [19] describe the variety of rectal disinfectants: bisacodyl, phosphate and povidone-iodine administered as enemas or suppositories. The different techniques translated to a range of septic complications 0.2%–9.3% and overall infective complications 2.6%–23.6% [19].
Park et al. [19] recently demonstrated that a povidoneiodine suppository or enema reduced bacterial colony counts from rectal swabs by approximately a factor of one thousand from around 106 to 103. Park et al. [19] describe a series of 1,684 patients treated with a combination of prophylactic antibiotics and povidone-iodine suppository. In this series they reported zero septic complications and a low (0.65%) overall infective complications. Unfortunately their antibiotic regime was not similar to other studies (a 3rd generation cephalosporin and cefixime 100 mg PO for 5 days) and so their results may not be directly comparable to other studies. Recently, Abughosh et al. [11] performed a randomized prospective trial of 865 men demonstrated a nonstatistically significant reduction in septic complications of 1.6% to 1.0% with the addition of povidone-iodine rectal cleansing to oral ciprofloxacin [11]. The authors suggested that povidone-iodine rectal disinfectant may be a useful adjunct to antibiotic prophylaxis, particularly for patients at risk of fluoroquinolone resistance, as they felt it was quick, inexpensive and easy to perform.
Another approach described by Issa et al. [20] in 2013 involved disinfecting biopsy needles between each core using formaldehyde. They reported a reduction in infective complications by two-thirds compared to historical data from their institution. An additional benefit of this technique is that it is not subject to concerns regarding fluoroquinolone resistance and the authors demonstrated ex vivo that such isolates were still susceptible to formaldehyde. The authors estimated that the technique involved 3.9 mg of formaldehyde which is lower than the maximum daily exposure recommended by the environmental protection agency of 14 mg. However, a 2010 study found no significant added benefit from a povidone-iodine solution to disinfect biopsy needles between cores when standard antibiotic prophylaxis was employed [21]. Other methodologies include dipping the needle into betadine between biopsies or wiping the biopsy specimen off the needle with alcohol. Although supportive data on these last 2 methods is lacking, washing the needle in formaldehyde produces better cores for analysis than swiping onto material such as paper [22].
Tuncel et al. [23] reported that the use of a disposable needle guide, compared to a reusable needle guide disinfected between patients, significantly reduced the number of fevers and urinary tract infections after biopsy [23]. These results were not supported by a later study by Gurbuz et al. [24] who observed no difference. Both studies had similar antibiotic prophylaxis and disinfection regimes and it may be that the differences were due to technical differences in the model of needle guide used.
A recent study has demonstrated that the number of biopsy needles is proportional to the infection risk. The study suggested an increasing risk of infective complications with 6, 12, and 18 needles. However, the study did not investigate the number of severe infections such as sepsis or measure infection severity as indicated by hospitalizations [25]. Another small study suggested that the size of the biopsy needle was not associated with either cancer detection rate or the number of infective complications [26]. These studies suggest it may be prudent for a urologist, in the context of a palpable nodule or targeted biopsy, to take fewer cores if a patient is at elevated risk of infection.
Transperineal biopsy is a novel prostate biopsy technique. The transperineal approach enables the urologist to thoroughly swab the perineum with a disinfectant solution to eliminate skin flora [27]. Additionally, unlike a transrectal approach, transperineal biopsy avoids penetrating bowel mucosa and therefore minimizes blood exposure to bowel flora. Transperineal biopsy, in combination with variable antibiotic prophylaxis, has been shown to have a near-zero septic complication rate with a recent Australian study of 6,609 biopsies resulting in only 5 hospital re-admissions for sepsis [28]. Another study of 634 patients, also treated with amikacin 500 mg IV at induction and ciprofloxacin 500 mg BD for 3 days, had zero episodes of sepsis [29]. Some authors suggest that transperineal biopsy may not necessitate antibiotic prophylaxis and the avoidance of unnecessary antibiotic therapy can be considered good antibiotic stewardship [28]. Australian guidelines state that antibiotic prophylaxis may or may not be required, but suggest 2 g IV cephazolin 15–30 minutes beforehand if antibiotic prophylaxis is desired [12].
Recent advances in multiparametric magnetic resonance imaging (MRI) allow an expanding clinical scope for noninvasive imaging. Some authors argue MRI may be more useful than a TRUS biopsy in specific situations, such as anterior tumours, which reduces the need for repeated TRUS biopsies therefore incidentally lowering biopsy complication rates [430].
Antibiotic resistance, particularly fluoroquinolone resistance, appears to be driving an increase in the number of infective complications, including urosepsis, occurring after prostate biopsy. Effective strategies to reduce this feared complication include augmented prophylaxis, rectal swab culture directed antibiotic prophylaxis and a transperineal biopsy approach. Needle disinfection, minimizing the number of biopsy needles and rectal disinfectants may also be of use.
References
1. Bruyere F, Malavaud S, Bertrand P, Decock A, Cariou G, Doublet JD, et al. Prosbiotate: a multicenter, prospective analysis of infectious complications after prostate biopsy. J Urol. 2015; 193:145–150. PMID: 25063492.
2. Carignan A, Roussy JF, Lapointe V, Valiquette L, Sabbagh R, Pepin J. Increasing risk of infectious complications after transrectal ultrasound-guided prostate biopsies: time to reassess antimicrobial prophylaxis? Eur Urol. 2012; 62:453–459. PMID: 22575912.

3. Nam RK, Saskin R, Lee Y, Liu Y, Law C, Klotz LH, et al. Increasing hospital admission rates for urological complications after transrectal ultrasound guided prostate biopsy. J Urol. 2013; 189(1 Suppl):S12–S17. PMID: 23234616.

4. Ahmed HU, Emberton M. The role of magnetic resonance imaging in targeting prostate cancer in patients with previous negative biopsies and elevated prostate-specific antigen levels. BJU Int. 2009; 104:269–270. PMID: 19594515.
5. Batura D, Gopal Rao G. The national burden of infections after prostate biopsy in England and Wales: a wake-up call for better prevention. J Antimicrob Chemother. 2013; 68:247–249. PMID: 23047808.

6. Zani EL, Clark OA, Rodrigues Netto. Antibiotic prophylaxis for transrectal prostate biopsy. Cochrane Database Syst Rev. 2011; (5):CD006576. PMID: 21563156.

7. Cohen JE, Landis P, Trock BJ, Patel HD, Ball MW, Auwaerter PG, et al. Fluoroquinolone resistance in the rectal carriage of men in an active surveillance cohort: longitudinal analysis. J Urol. 2015; 193:552–556. PMID: 25111911.

8. Dai J, Leone A, Mermel L, Hwang K, Pareek G, Schiff S, et al. Rectal swab culture-directed antimicrobial prophylaxis for prostate biopsy and risk of postprocedure infection: a cohort study. Urology. 2015; 85:8–14. PMID: 25458193.

9. Laupland KB, Gregson DB, Church DL, Ross T, Pitout JD. Incidence, risk factors and outcomes of Escherichia coli bloodstream infections in a large Canadian region. Clin Microbiol Infect. 2008; 14:1041–1047. PMID: 19040476.

10. Patel U, Dasgupta P, Amoroso P, Challacombe B, Pilcher J, Kirby R. Infection after transrectal ultrasonography-guided prostate biopsy: increased relative risks after recent international travel or antibiotic use. BJU Int. 2012; 109:1781–1785. PMID: 22040349.

11. Abughosh Z, Margolick J, Goldenberg SL, Taylor SA, Afshar K, Bell R, et al. A prospective randomized trial of povidoneiodine prophylactic cleansing of the rectum before transrectal ultrasound guided prostate biopsy. J Urol. 2013; 189:1326–1331. PMID: 23041343.

12. Therapeutic Guidelines Limited. Prophylaxis: urological surgery. eTG complete [Internet]. West Melbourne: Therapeutic Guidelines Limited;2014. 2015 Aug 23. Available from: http://www.tg.org.au/.
13. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009; 6:e1000100. PMID: 19621070.

14. Toner L, Papa N, Aliyu SH, Dev H, Lawrentschuk N, Al-Hayek S. Extended-spectrum beta-lactamase-producing Enterobacteriaceae in hospital urinary tract infections: incidence and antibiotic susceptibility profile over 9 years. World J Urol. 2015; 10. 28. [Epub]. DOI: 10.1007/s00345-015-1718-x.
15. Womble PR, Linsell SM, Gao Y, Ye Z, Montie JE, Gandhi TN, et al. A Statewide Intervention to Reduce Hospitalizations after Prostate Biopsy. J Urol. 2015; 194:403–409. PMID: 25896556.

16. Batura D, Rao GG, Bo Nielsen P, Charlett A. Adding amikacin to fluoroquinolone-based antimicrobial prophylaxis reduces prostate biopsy infection rates. BJU Int. 2011; 107:760–764. PMID: 21029317.

17. Taylor AK, Zembower TR, Nadler RB, Scheetz MH, Cashy JP, Bowen D, et al. Targeted antimicrobial prophylaxis using rectal swab cultures in men undergoing transrectal ultrasound guided prostate biopsy is associated with reduced incidence of postoperative infectious complications and cost of care. J Urol. 2012; 187:1275–1279. PMID: 22341272.

18. Qi C, Malczynski M, Schaeffer AJ, Barajas G, Nadler RB, Scheetz MH, et al. Characterization of ciprofloxacin resistant Escherichia coli isolates among men undergoing evaluation for transrectal ultrasound guided prostate biopsy. J Urol. 2013; 190:2026–2032. PMID: 23727416.

19. Park DS, Hwang JH, Choi DK, Gong IH, Hong YK, Park S, et al. Control of infective complications of transrectal prostate biopsy. Surg Infect (Larchmt). 2014; 15:431–436. PMID: 24840927.

20. Issa MM, Al-Qassab UA, Hall J, Ritenour CW, Petros JA, Sullivan JW. Formalin disinfection of biopsy needle minimizes the risk of sepsis following prostate biopsy. J Urol. 2013; 190:1769–1775. PMID: 23714433.

21. Koc G, Un S, Filiz DN, Akbay K, Yilmaz Y. Does washing the biopsy needle with povidone-iodine have an effect on infection rates after transrectal prostate needle biopsy? Urol Int. 2010; 85:147–151. PMID: 20453481.

22. Satasivam P, Thomas R, Rao K, Jack GS, Lawrentschuk N, Bolton DM. Fragmentation of transrectal ultrasound-guided biopsy cores is influenced by the method of specimen retrieval. Urology. 2014; 83:622–625. PMID: 24581525.

23. Tuncel A, Aslan Y, Sezgin T, Aydin O, Tekdogan U, Atan A. Does disposable needle guide minimize infectious complications after transrectal prostate needle biopsy? Urology. 2008; 71:1024–1027. PMID: 18400273.

24. Gurbuz C, Canat L, Atis G, Caskurlu T. Reducing infectious complications after transrectal prostate needle biopsy using a disposable needle guide: is it possible? Int Braz J Urol. 2011; 37:79–84. PMID: 21385483.

25. Ghafoori M, Velayati M, Aliyari Ghasabeh M, Shakiba M, Alavi M. Prostate biopsy using transrectal ultrasonography; the optimal number of cores regarding cancer detection rate and complications. Iran J Radiol. 2015; 12:e13257. PMID: 26060552.

26. McCormack M, Duclos A, Latour M, McCormack MH, Liberman D, Djahangirian O, et al. Effect of needle size on cancer detection, pain, bleeding and infection in TRUS-guided prostate biopsies: A prospective trial. Can Urol Assoc J. 2012; 6:97–101. PMID: 22511415.

27. Chang DT, Challacombe B, Lawrentschuk N. Transperineal biopsy of the prostate: is this the future? Nat Rev Urol. 2013; 10:690–702. PMID: 24061531.
28. Grummet JP, Weerakoon M, Huang S, Lawrentschuk N, Frydenberg M, Moon DA, et al. Sepsis and 'superbugs': should we favour the transperineal over the transrectal approach for prostate biopsy? BJU Int. 2014; 114:384–388. PMID: 24612341.

29. Vyas L, Acher P, Kinsella J, Challacombe B, Chang RT, Sturch P, et al. Indications, results and safety profile of transperineal sector biopsies (TPSB) of the prostate: a single centre experience of 634 cases. BJU Int. 2014; 114:32–37. PMID: 24053629.

30. Toner L, Weerakoon M, Bolton DM, Ryan A, Katelaris N, Lawrentschuk N. Magnetic resonance imaging for prostate cancer: Comparative studies including radical prostatectomy specimens and template transperineal biopsy. Prostate Int. 2015; 3:107–114. PMID: 26779455.

Fig. 1
Flowchart of study selection as per the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) statement.
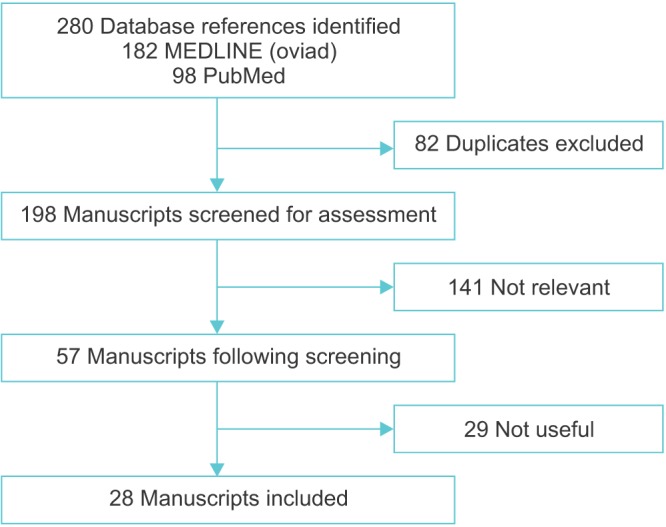
Table 1
Measures taken in selected studies to reduce infective complications from prostate biopsy
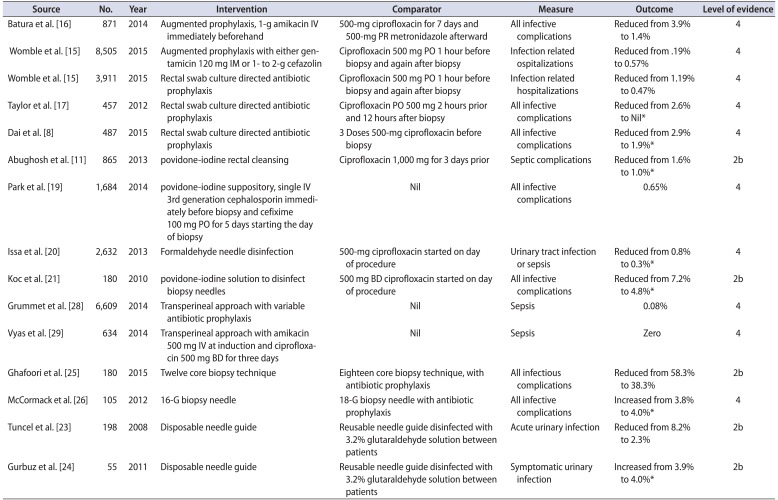
| Source | No. | Year | Intervention | Comparator | Measure | Outcome | Level of evidence |
|---|---|---|---|---|---|---|---|
| Batura et al. [16] | 871 | 2014 | Augmented prophylaxis, 1-g amikacin IV immediately beforehand | 500-mg ciprofloxacin for 7 days and 500-mg PR metronidazole afterward | All infective complications | Reduced from 3.9% to 1.4% | 4 |
| Womble et al. [15] | 8,505 | 2015 | Augmented prophylaxis with either gentamicin 120 mg IM or 1- to 2-g cefazolin | Ciprofloxacin 500 mg PO 1 hour before biopsy and again after biopsy | Infection related ospitalizations | Reduced from .19% to 0.57% | 4 |
| Womble et al. [15] | 3,911 | 2015 | Rectal swab culture directed antibiotic prophylaxis | Ciprofloxacin 500 mg PO 1 hour before biopsy and again after biopsy | Infection related hospitalizations | Reduced from 1.19% to 0.47% | 4 |
| Taylor et al. [17] | 457 | 2012 | Rectal swab culture directed antibiotic prophylaxis | Ciprofloxacin PO 500 mg 2 hours prior and 12 hours after biopsy | All infective complications | Reduced from 2.6% to Nil* | 4 |
| Dai et al. [8] | 487 | 2015 | Rectal swab culture directed antibiotic prophylaxis | 3 Doses 500-mg ciprofloxacin before biopsy | All infective complications | Reduced from 2.9% to 1.9%* | 4 |
| Abughosh et al. [11] | 865 | 2013 | povidone-iodine rectal cleansing | Ciprofloxacin 1,000 mg for 3 days prior | Septic complications | Reduced from 1.6% to 1.0%* | 4 |
| Park et al. [19] | 1,684 | 2014 | povidone-iodine suppository, single IV 3rd generation cephalosporin immediately before biopsy and cefixime 100 mg PO for 5 days starting the day of biopsy | Nil | All infective complications | 0.65% | 4 |
| Issa et al. [20] | 2,632 | 2013 | Formaldehyde needle disinfection | 500-mg ciprofloxacin started on day of procedure | Urinary tract infection or sepsis | Reduced from 0.8% to 0.3%* | 4 |
| Koc et al. [21] | 180 | 2010 | povidone-iodine solution to disinfect biopsy needles | 500 mg BD ciprofloxacin started on day of procedure | All infective complications | Reduced from 7.2% to 4.8%* | 2b |
| Grummet et al. [28] | 6,609 | 2014 | Transperineal approach with variable | Nil | Sepsis | 0.08% | 4 |
| Vyas et al. [29] | 634 | 2014 | Transperineal approach with amikacin 500 mg IV at induction and ciprofloxacin 500 mg BD for three days | Nil | Sepsis | Zero | 4 |
| Ghafoori et al. [25] | 180 | 2015 | Twelve core biopsy technique | Eighteen core biopsy technique, with antibiotic prophylaxis | All infectious complications | Reduced from 58.3% to 38.3% | 2b |
| McCormack et al. [26] | 105 | 2012 | 16-G biopsy needle | 18-G biopsy needle with antibiotic prophylaxis | All infective complications | Increased from 3.8% to 4.0%* | 4 |
| Tuncel et al. [23] | 198 | 2008 | Disposable needle guide | Reusable needle guide disinfected with 3.2% glutaraldehyde solution between patients | Acute urinary infection | Reduced from 8.2% to 2.3% | 2b |
| Gurbuz et al. [24] | 55 | 2011 | Disposable needle guide | Reusable needle guide disinfected with 3.2% glutaraldehyde solution between patients | Symptomatic urinary infection | Increased from 3.9% to 4.0%* | 2b |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download