Abstract
There are many different approaches to ultrasound-guided supraclavicular brachial plexus block (US-SCBPB), and each has a different success rate and complications. The most commonly performed US-SCBPB is the corner pocket approach in which the needle is advanced very close to the subclavian artery and pleura. Therefore, it may be associated with a risk of subclavian artery puncture or pneumothorax. We advanced the needle into the central part of the neural cluster after penetrating the sheath of the brachial plexus in US-SCBPB. We refer to this new method as the "central cluster approach." In this approach, the needle does not have to advance close to the subclavian artery or pleura. The aim of this study was to evaluate the clinical outcomes of the central cluster approach in US-SCBPB.
A supraclavicular block can provide effective surgical anesthesia of the forearm and hand. However, there have always been complications such as pneumothorax, vascular punctures, local anesthetic toxicity due to unintended intravascular injection, Horner's syndrome, recurrent laryngeal nerve blockade, and phrenic nerve blockade [12]. After an initial period of popularity, the use of the supraclavicular block declined significantly because of these complications [12].
Ultrasound has made the supraclavicular block popular again owing to improved block quality and fewer complications with this method than with the nonultrasound-based supraclavicular block [3]. Ultrasound imaging can help accurately localize the brachial plexus, which is lateral and posterior to the subclavian artery and above the first rib. It can also help guide needle advancement to the target nerves and show the spread of the local anesthetic around the nerves in real time [45]. However, each approach is associated with its own success rates and complications in ultrasound-guided supraclavicular brachial plexus block (US-SCBPB) [1246789].
We tried a new approach in which the needle was advanced into the center of the brachial plexus at the supraclavicular area superolateral to the neural compartment. We named this method the "central cluster approach." We report the clinical outcome of the central cluster approach of US-SCBPB in 51 patients.
This study was approved by the ethical review board of our hospital. Written, informed consent was obtained from all patients. Fifty-one patients scheduled for forearm and hand surgery were enrolled in the study. The patients were aged 18-80 years, and had an American Society of Anesthesiologists physical status of I to III. The exclusion criteria included a body mass index greater than 35 kg/m2, infection at the injection site, existing neurologic disease, severe respiratory disease, coagulopathy, or any other contraindication to brachial plexus block [5]. Data were collected from January 2012 to March 2014.
Before the nerve blockade, all patients received standard monitoring (e.g., noninvasive blood pressure, electrocardiogram, and pulse oximetry). Before the procedure, anxiolysis was established with 1-2 mg of midazolam and 50 µg of intravenous fentanyl.
The US-SCBPB was performed with the patient lying supine and the head turned 30 degrees to the nonoperative side. A linear high-frequency (6-13 MHz) ultrasound probe (SonoSite M-Turbo; Sonosite, Bothell, WA, USA), which was covered with a sterile dressing, was placed in the supraclavicular fossa in the coronal-oblique plane parallel and immediately posterior to the clavicle (Fig. 1A). The brachial plexus was identified as a compact group of nerves lateral and posterior to the subclavian artery and above the first rib and pleura.
After sterilizing the skin and applying a local anesthetic (2-3 ml of 1% lidocaine), a 22-gauge 50 mm insulated block needle (Stimuplex A; B.Braun, Melsungen, Germany) was inserted through the skin at the lateral end of the probe and advanced along its axis in the same plane as the ultrasound beam (i.e., the in-plane approach). We evaluated the pulsation of the supraclavicular artery by color Doppler (Fig. 1B). The needle was advanced until it penetrated the brachial plexus sheath, and the needle tip was positioned in the center of the sheath compartment among the nerves. All blocks were performed by one expert staff anesthesiologist.
The needle tip was always visualized before the local anesthetic injection. Once the needle position was satisfactory and after confirming negative aspiration, the local anesthetic was injected in 3 ml increments after intermittent negative aspiration for 3-5 min using direct ultrasound visualization of the local anesthetic spread. This ensured the expansion of the brachial plexus sheath (Fig. 1C). The total volume of the local anesthetic mixture was 30 ml (10 ml of 1.5% lidocaine mixed with 20 ml of 0.5% ropivacaine and 1 : 200,000 epinephrine).
Patients were closely monitored in the perioperative period for any symptoms or signs of respiratory difficulty. An alcohol swab was used to evaluate the sensory nerve block. An independent resident checked the motor block every 5 min for 30 min in each nerve location.
The subsequent needle advancement was preceded by a needle withdrawal of at least 10 mm. We recorded the block onset time, which was defined as the time between the end of the injection and development of the complete block of the four nerves. A successful block was defined as complete sensory and motor block in all regions, as assessed within 30 min of the local anesthetic injection. If the block was considered unsuccessful in a single nerve territory, it was supplemented distally in the arm or forearm with an ultrasound-guided peripheral nerve block. If there were extensive areas of preserved sensation beyond a single nerve territory, a general anesthetic was scheduled to be administered at the discretion of the attending anesthesiologist. Intraoperative anxiolysis was achieved with 1-3 mg midazolam and 50 µg intravenous fentanyl.
Table 1 presents the patient demographic characteristics and perioperative data. Three patients complained of paresthesia during the procedure, which soon disappeared when the needle was withdrawn slightly. Four patients complained of tourniquet pain because of a prolonged operation, but the pain subsided quickly with fentanyl and intravenous midazolam. The number of needle passes was less than three in each patient, but we did not record the number of needle passes in every patient.
Table 2 documents the block outcomes and the complications of US-SCBPB. Symptoms of Horner's syndrome (one patient) and hoarseness (two patients) resolved 1-2 h after the nerve block. Symptomatic diaphragmatic paresis was confirmed in one patient by portable chest radiography; however, this outcome was not accompanied by pneumothorax, and mild shortness of breath resolved 1-2 h after the nerve block. Complete recovery of sensory and motor function was confirmed in all patients. No neurologic complications were reported during 6 weeks of follow up.
When using the central cluster approach, subclavian artery puncture or pneumothorax did not develop in any of the 51 patients. We advanced the needle tip to the supero-lateral part of the grapes of the brachial plexus, and penetrated more deeply to the center of the grapes. We named this procedure the "central cluster approach."
The first advantage of this approach is that the subclavian artery and pleura are away from the needle tip anatomically. The targets of the supraclavicular block are the trunks or divisions of the brachial plexus, which are anatomically near the subclavian artery and pleura [10]. Therefore, the incidence of pneumothorax and subclavian artery puncture are of concern, even though they are theoretically less likely under ultrasound guidance, and their incidence varies, depending on the method of approach [10].
The corner pocket approach is a well-utilized method in USSCBPB. The target for the needle tip placement is the corner bordered by the subclavian artery medially and the first rib and pleura inferiorly [2,6,11]. The local anesthetic is deposited at this point; therefore, the divisions of the brachial plexus float superiorly [2]. Many authors suggest that this approach can achieve a dense and complete block of the entire upper extremity within minutes, and for this reason, it is often preferred [2,6,7,11]. However, it also has a risk of subclavian artery puncture and pneumothorax because the block needle needs to be advanced very close to the subclavian artery and pleura [1]. In our institute's clinical experience, it is easier to handle the needle in the central cluster approach than in the corner pocket approach.
The second advantage of the central cluster approach is that the chance of circumferential or symmetrical spreading of local anesthetic is increased. In the traditional cluster approach, the needle tip is positioned just within the sheath compartment among the nerves [1,7]. The successful surgical anesthetic rate of this approach can be less than that of the corner pocket approach because of the increased chance of lopsided spreading of the local anesthetic at the injection point [7]. In contrast, the central cluster approach is a modification of the established cluster approach in that the needle is deeply positioned at the center of the neural cluster in the ultrasound image; therefore, local anesthetics can spread from the center to the periphery within the sheath (Fig. 2). In our study, the success rate was 92.2% (n = 47). Lopsided spreading of the local anesthetics at the injection point developed in only four (7.8%) patients.
One concern with the central cluster approach is the possibility of intraneural injection because the advance of the needle tip is more than a simple penetration of the plexus sheath. More than 50% of the brachial plexus in the supraclavicular region is composed of fat and connective tissue in the sheath [9,12]. We believe that the local anesthetic is deposited in these connective tissues, and not in the fascicles (which are visible as distinct round to oval hypoechoic nodules within the sheath) [9,13]. Nerve fascicles may escape direct injury from a block needle because the perineurium may be a more critical barrier of the fascicle than the epineurium, which is generally assumed to be the outermost border of the nerve within the sheath [9,13]. In our study, no patient withdrew their arm suddenly or communicated having severe pain during the procedure. No patient had paresthesia or neurologic injury during the 6-week follow-up period.
This was a preliminary study on the new approach. However, it did not have a control group. Therefore, we cannot definitely insist that the central cluster approach is superior to the existing corner pocket approach or cluster approach. Our study had an insufficient patient number to make a definitive recommendation on this topic. Therefore, a larger number of patients and a randomized controlled trial are required to testify to the superiority of this new approach. We focused on the success rate and complications of the central cluster approach. We did not investigate the time-based sensory and motor block of the four nerves, which was also a limitation of the study.
In conclusion, we performed the central cluster approach at the supraclavicular level. We advanced the needle into the center of the brachial plexus in 51 patients, and described the success rate and complications of this new method.
References
1. Perlas A, Lobo G, Lo N, Brull R, Chan VW, Karkhanis R. Ultrasound-guided supraclavicular block: outcome of 510 consecutive cases. Reg Anesth Pain Med. 2009; 34:171–176. PMID: 19282715.
2. Soares LG, Brull R, Lai J, Chan VW. Eight ball, corner pocket: the optimal needle position for ultrasound-guided supraclavicular block. Reg Anesth Pain Med. 2007; 32:94–95. PMID: 17196502.

3. Choi S, McCartney CJ. Evidence base for the use of ultrasound for upper extremity blocks: 2014 update. Reg Anesth Pain Med. 2014; [Epub ahead of print].
4. Chan VW, Perlas A, Rawson R, Odukoya O. Ultrasound-guided supraclavicular brachial plexus block. Anesth Analg. 2003; 97:1514–1517. PMID: 14570677.

5. Duggan E, El Beheiry H, Perlas A, Lupu M, Nuica A, Chan VW, et al. Minimum effective volume of local anesthetic for ultrasound-guided supraclavicular brachial plexus block. Reg Anesth Pain Med. 2009; 34:215–218. PMID: 19587618.

6. Morfey DH, Brull R. Finding the corner pocket: landmarks in ultrasound-guided supraclavicular block. Anaesthesia. 2009; 64:1381. PMID: 20092529.

7. Tran DQ, Munoz L, Russo G, Finlayson RJ. A trick shot to the corner pocket. Reg Anesth Pain Med. 2008; 33:503–504. PMID: 18774522.

8. Roy M, Nadeau MJ, Côté D, Levesque S, Dion N, Nicole PC, et al. Comparison of a single- or double-injection technique for ultrasoundguided supraclavicular block. Reg Anesth Pain Med. 2012; 37:55–59. PMID: 22030724.

9. Bigeleisen PE, Moayeri N, Groen GJ. Extraneural versus intraneural stimulation thresholds during ultrasound-guided supraclavicular block. Anesthesiology. 2009; 110:1235–1243. PMID: 19417603.

10. Butterworth JF, Mackey DC, Wasnick JD. Regional anesthesia and pain management. In : Madison SJ, Ilfeld BM, editors. Morgan's Clinical Anesthesiology. 5th ed. Seoul: Mc Graw Hill Education Publishers;2013. p. 986–989.
11. Samet R, Villamater E. Eight ball, corner pocket for ultrasound-guided supraclavicular block: high risk for a scratch. Reg Anesth Pain Med. 2008; 33:87. PMID: 18155063.

12. Bigeleisen PE. Nerve puncture and apparent intraneural injection during ultrasound-guided axillary block does not invariably result in neurologic injury. Anesthesiology. 2006; 105:779–783. PMID: 17006077.

13. Morfey D, Brull R. Ultrasound-guided supraclavicular block: What is intraneural. Anesthesiology. 2010; 112:250–251. PMID: 20032713.

Fig. 1
(A) The patient positioning and transducer location to obtain the short axis view of the neurovascular structures at the supraclavicular fossa. (B) Ultrasound image of the supraclavicular brachial plexus, which appears as a compact group of nerves (arrows) lateral and posterior to the subclavian artery (red) and above the first rib. (C) Ultrasound image of the brachial plexus after the injection of the local anesthetic. The block needle (arrows) is inserted in a superolateral direction until reaching the central part of the cluster of the brachial plexus. The brachial plexus sheath compartment is expanded after the local anesthetic injection. BP: brachial plexus, rib 1: first rib, SA: subclavian artery.
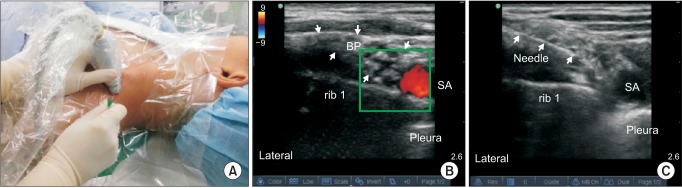
Fig. 2
Schematic diagram of the sonoguided supraclavicular brachial plexus block with in-plane needle advancement, and its related anatomy. In the traditional cluster approach, the needle tip is positioned just within the brachial plexus sheath. The central cluster approach is different from the cluster approach in that the needle is advanced into the central part of the sheath. Therefore, the chance of symmetrical spreading of local anesthetic from center to the peripheral within the sheath is increased (Illustration by Dr. WoonRak Son from Gachon University Gil Hospital).
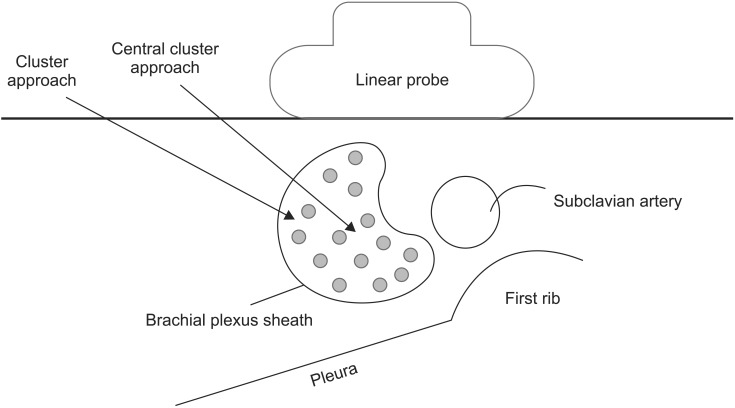
Table 1
Patient Demographic Characteristics and Perioperative Data
The values are presented as the mean number of patients ± the standard deviation. The procedure time is the sum of the imaging and needling times. The block onset time is the time between the end of the injection and the development of the complete block of the four nerves. ASA: American Society of Anesthesiologists.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download