Abstract
Video-assisted thoracoscopic surgery for pediatric patients has gained popularity due to better outcomes than open surgery. For this procedure, one-lung ventilation may be necessary to provide an adequate surgical field. Confirming lung isolation is crucial when one-lung ventilation is required. Recently, we experienced a case in which one-lung ventilation was confirmed by ultrasonography using the lung sliding sign and the lung pulse in an infant. Since lung ultrasonography can be performed easily and quickly, it may be a useful method to confirm lung isolation, particularly in emergency surgeries with limited time, devices, and experienced anesthesiologists.
With advances in technology, minimally invasive thoracoscopic procedures in infants and children are gaining popularity. Although thoracoscopic surgery can be performed without lung isolation, the operative-sided lung should be isolated in some cases, because one-lung ventilation ensures good surgical conditions and low incidence of accidental lung injury [1]. Confirmation of lung isolation before surgery is therefore important to provide an adequate operative field during surgery. Recently, ultrasonography has been utilized in airway management including lung isolation in adult patients [23]. However, there are few reports on the application of ultrasonography for lung isolation in pediatric patients. Here, we report a case of using ultrasonography for lung isolation in an infant undergoing emergent thoracoscopic diaphragmatic hernia repair.
A 9-month-old boy (weight : 9 kg, height : 70.5 cm) was brought into our emergency department with a complaint of vomiting. His past medical history included a repair of a congenital diaphragmatic hernia 8 months prior. Chest radiography showed left lung haziness with pleural effusion and gaseous distended bowel loops in the upper abdomen. Computerized tomography of the chest revealed herniated bowel loops in the left lower lung field and consequent passive atelectasis, suggesting recurrent diaphragmatic hernia and bowel strangulation. Preoperative electrocardiogram and laboratory findings were all within normal ranges. He was given 1 L/min oxygen by nasal prong, and peripheral oxygen saturation was maintained at 100%. After completion of his evaluation, emergency thoracoscopic diaphragmatic hernia repair was decided.
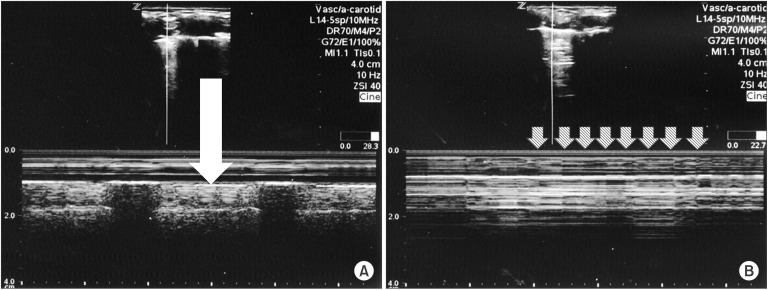
General anesthesia was induced with intravenous propofol 3 mg/kg, and rapid sequence intubation with a cuffed endotracheal tube (inner diameter 4.0 mm) was performed after intravenous infusion of atropine 0.02 mg/kg and succinylcholine 2 mg/kg. An endotracheal tube was fixed at a depth of 13 cm from the incisor. Breath sounds were bilaterally audible on chest auscultation, but with decreased sound at the left middle and lower lung field. Anesthesia was maintained with sevoflurane in 50% oxygen/air, and an arterial catheter was placed at the left radial artery. After successful ultrasound-guided central venous catheterization in the left internal jugular vein, chest radiography was performed to determine the positions of the central venous catheter and the endotracheal tube. A specific surgical plan had not yet been fully confirmed, and the need for isolating the operative-side lung was considered. To determine whether endobronchial intubation with a single-lumen tube was enough to provide one-lung ventilation, or whether other techniques such as bronchial blockers were required for lung isolation, we introduced the endotracheal tube into the right main bronchus as a trial. Although the breath sound at the left upper lung field was likely to decrease after inserting the tube 2 cm deeper, we could not ensure right endobronchial intubation. To confirm the placement of the tube, portable chest radiography was considered. However, the chest radiography would only be available 30 minutes later. Fiberoptic bronchoscopy was equipped in the operating room, but it was not favorable due to the lack of a skilled anesthesiologist and the risk of hypoxia. Therefore, we decided to identify the endobronchial intubation using ultrasonography (z.one ultra sp, ZONARE medical system, Mountain view, CA, USA). After withdrawal of the tube to a 13 cm depth, ultrasonography was commenced. The patient was positioned supine, and a 4 cm sized pediatric 5-14 MHz linear ultrasound probe was placed sagittally into both midclavicular lines. An initial exam revealed rhythmical movement of the pleural line synchronized with respiratory movement (lung sliding sign) at both upper lung fields. Using motion mode (M-mode) imaging, we identified a homogenous granular pattern (Fig. 1A), known as a 'seashore sign', below the echogenic pleural line. When we gently inserted the endotracheal tube, we observed pleural movement of the left upper lung field using real-time ultrasonography. After insertion of the endotracheal tube (at a depth of 15 cm), the lung sliding sign disappeared and a 'lung pulse', the recording of vibrations synchronized with heart activity, was detected (Fig. 1B). In contrast to the left side, the lung sliding sign of the right upper lung field could still be detected, suggesting that the right endobronchial intubation was performed successfully. After confirming the disappearance of left lung sliding sign, the endotracheal tube was pulled back to a 13 cm depth and the left lung sliding sign reappeared.
Finally, thoracoscopic surgery began without lung isolation, and an acceptable surgical field was obtained. The operation was completed with no adverse events, and the patient was delivered to the pediatric intensive care unit without extubation. Immediate postoperative chest radiography showed improved haziness in the left lung, and the patient was extubated 1 hour later. The patient was discharged without complications on postoperative day 11.
One-lung ventilation technique during thoracoscopic surgery requires advanced skills especially when performed in infants. Because of the small tracheal and bronchial diameter of infants, lung isolation is usually achieved by endobronchial intubation with single-lumen endotracheal tube [4]. It is imperative to confirm appropriate tube placement in order to provide an adequate surgical field. In our present case, ultrasonography was used to verify one-lung ventilation.
Traditionally, lung auscultation [5], chest wall observation [5], fiberoptic bronchoscopy [1], chest radiography, and fluoroscopy [6] have been used to confirm proper lung isolation. Auscultation and chest wall observation are simple techniques and require no special equipment, but are not reliable methods [5]. Although chest radiography and fluoroscopy are accurate enough to determine the appropriate tube position, they are time consuming [7] and may not be suitable in emergency situations. In addition, there are concerns about the risks associated with radiologic exposure [8]. Fiberoptic bronchoscopy is regarded as the gold standard to confirm proper endotracheal tube placement. However, in small infants, it is difficult to define the tracheobronchial anatomy [6] and there is a potential risk of desaturation during bronchoscopy due to their low oxygen reserve.
Recently, the applicability of ultrasonography has been expanded to airway management [2], and several authors have described ultrasonographic identification of endobronchial intubation [791011]. Two characteristic signs, the lung sliding sign and the lung pulse, can be used to verify endotracheal or endobronchial tube position. The lung sliding sign is the sliding movement of hyperechoic pleural layers against each other, synchronized with respiration [12]. The application of M-mode facilitates to identify lung sliding by detecting superficial multiple horizontal lines and fuzzy imaging under the pleura, referred to as the see-shore sign [12]. The presence of the lung sliding sign suggests normal lung movement with intact interpleural space during respiration [1013]. The lung pulse is the recording of vibrations synchronized with heart activity at the pleural line and can be explained by transmission of the heartbeat through a motionless lung [10]. In a well-ventilated lung, the lung sliding sign is dominant, overriding the heart signal. On non-ventilated lung segments, lung pulse immediately replaces the lung sliding sign [10]. The absence of the lung sliding sign and the presence of the lung pulse indicate the existence of non-ventilated lung segments produced by endobronchial intubation [10].
Confirmation of lung isolation using lung ultrasonography can be performed quickly and easily. Lung ultrasonography is less time-consuming than chest radiography [7] and lessens the risk of multiple radiation exposure. Moreover, it is a relatively simple technique that even the beginners can perform with least training [13].
Ultrasonographic lung isolation has some limitations. In the presence of pneumothorax, pleural adhesion, or subcutaneous emphysema, the lung sliding sign can be misleading [12]. Hence, careful evaluation of preoperative chest radiography and an initial ultrasonography exam before intubation are necessary [10]. In addition, the reliability and accuracy of lung ultrasonography to confirm the endotracheal tube position in pediatric patients have not been fully evaluated compared to adult patients [71011]. Moreover, when the patient's position changes or desaturation develops during one-lung ventilation, appropriate endotracheal tube position must be reconfirmed. However, the usefulness of lung ultrasonography to detect dislodgement of the tube has not been clearly elucidated. Hence, lung ultrasonography cannot be utilized as a standard technique instead of fiberoptic bronchoscopy. Despite these limitations, lung ultrasonography may be an attractive technique to confirm lung isolation in pediatric patients. It can be utilized as a good adjuvant method to fiberoptic bronchoscopy and as a fast and easy alternative method particularly in emergency situations.
References
1. Dave N, Fernandes S. Anaesthetic implications of paediatric thoracoscopy. J Minim Access Surg. 2005; 1:8–14. PMID: 21234138.

2. Kristensen MS. Ultrasonography in the management of the airway. Acta Anaesthesiol Scand. 2011; 55:1155–1173. PMID: 22092121.

3. Sustic A, Protic A, Cicvaric T, Zupan Z. The addition of a brief ultrasound examination to clinical assessment increases the ability to confirm placement of double-lumen endotracheal tubes. J Clin Anesth. 2010; 22:246–249. PMID: 20522353.
4. Golianu B, Hammer GB. Pediatric thoracic anesthesia. Curr Opin Anaesthesiol. 2005; 18:5–11. PMID: 16534311.

5. Sitzwohl C, Langheinrich A, Schober A, Krafft P, Sessler DI, Herkner H, et al. Endobronchial intubation detected by insertion depth of endotracheal tube, bilateral auscultation, or observation of chest movements: randomised trial. BMJ. 2010; 341:c5943. PMID: 21062875.

6. Cohen DE, McCloskey JJ, Motas D, Archer J, Flake AW. Fluoroscopic-assisted endobronchial intubation for single-lung ventilation in infants. Paediatr Anaesth. 2011; 21:681–684. PMID: 21492317.

7. Sim SS, Lien WC, Chou HC, Chong KM, Liu SH, Wang CH, et al. Ultrasonographic lung sliding sign in confirming proper endotrachea intubation during emergency intubation. Resuscitation. 2012; 83:307–312. PMID: 22138058.
8. Brenner DJ. Estimating cancer risks from pediatric CT: going from the qualitative to the quantitative. Pediatr Radiol. 2002; 32:228–231. PMID: 11956700.

9. Blaivas M, Tsung JW. Point-of-care sonographic detection of left endobronchial main stem intubation and obstruction versus endotracheal intubation. J Ultrasound Med. 2008; 27:785–789. PMID: 18424655.

10. Lichtenstein DA, Lascols N, Prin S, Meziere G. The "lung pulse": an early ultrasound sign of complete atelectasis. Intensive Care Med. 2003; 29:2187–2192. PMID: 14557855.

11. Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med. 2006; 13:239–244. PMID: 16495415.

12. Piette E, Daoust R, Denault A. Basic concepts in the use of thoracic and lung ultrasound. Curr Opin Anaesthesiol. 2013; 26:20–30. PMID: 23103845.

13. Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012; 38:577–591. PMID: 22392031.

Fig. 1
(A) Scanning image of the left upper thorax obtained through a rib interspace. Upper, real-time mode. Lower, time-motion mode. Two-dimensional imaging showed a hyperechoic pleural line between two ribs. In time-motion mode, there were multiple horizontal lines over the pleural line and homogenous granular echogenicity below it, referred to as the 'seashore sign' (white arrow). (B) Scanning image of left upper thorax obtained through a rib interspace after inserting the tracheal tube 2 cm deeper. Upper, real-time mode. Lower, time-motion mode. The homogenous granular pattern below the pleural line disappeared and 'lung pulse', regular vertical lines (white striped arrows) synchronized with the heartbeat, appeared.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download