Abstract
Patients with Pierre Robin syndrome are characterized by micrognathia, retrognathia, glossoptosis, and respiratory obstruction and are prone to have a difficult-to-intubate airway. The McGrath® MAC video laryngoscope provides a better view of the glottis than a Macintosh laryngoscope, but it is not easy to insert an endotracheal tube through the vocal cords because a video laryngoscope has a much greater curvature than that of a conventional direct laryngoscope and an endotracheal tube has a different curvature. The Frova Intubating Introducer is used as a railroad for an endotracheal tube in cases of a difficult airway. We thought that a combination of these two devices would make it easy to insert an endotracheal tube through the vocal cords, as a McGrath® MAC video laryngoscope provides a better glottic view and the Frova Intubating Introducer is a useful device for placing an endotracheal tube through the glottis. We report a successful endotracheal intubation with use of the McGrath® MAC video laryngoscope and Frova Intubating Introducer in a patient with Pierre Robin syndrome.
Pierre Robin syndrome (PRS) accompanies a characteristic facies occurring in one in 8,500 live births and its clinical presentation is marked by micrognathia, retrognathia, glossoptosis, limited mouth opening, and cleft palate. Many children with PRS experience respiratory and feeding dysfunctions and may require prolonged tracheal intubation or surgical airway intervention in severe cases [1]. The facial malformation makes visualization of the glottis opening by direct laryngoscopy extremely difficult or impossible [2]. If tracheal intubation is necessary for anesthesia, awake fiber-optic intubation is recommended as the technique of choice [3]. However, this technique has certain limitations; the learning curve is steep, and considerable training is required to be proficient in its use. In addition, fiber-optic scopes are expensive, and their maintenance is time-consuming.
The McGrath® MAC video laryngoscope (Aircraft Medical, Edinburgh, UK) is commonly used to provide a good view of the upper airway when conventional direct laryngoscopy fails [4]. The design of a video laryngoscope is similar to conventional laryngoscopes, enabling clinicians familiar with direct laryngoscopy to use them successfully without the need for special training [5], and the technique is relatively easily acquired [6]. However, it is difficult to insert an endotracheal tube (ETT) because the blade of a video laryngoscope has a much greater curvature than that of a conventional direct laryngoscope.
The Frova Intubating Introducer (Cook Medical, Bloomington, IN, USA), one of the single-use tracheal introducers (frequently known as a bougie), has been in use for more than 10 years and may be the gold standard single-use introducer [7]. The difficult airway management guidelines developed by the Difficult Airway Society of the UK suggest early use of a tracheal tube introducer in cases of unanticipated intubation difficulties [8]. The combined use of a Frova Intubating Introducer and a McGrath® MAC video laryngoscope may provide a better method of managing the airway, as the latter provides a good glottic view and the former is useful for placing an ETT through the glottis.
We report a successful use of the McGrath® MAC video laryngoscope and Frova Intubating Introducer in a patient with PRS.
A 15-year-old male, who was diagnosed with PRS, was scheduled for repair of a pectus excavatum under general anesthesia. He had a history of tracheostomy at birth, a cleft palate operation at 1 month of age, and tracheostomy closure 1.5 years later. According to the consulting otolaryngologist, there was no pathological condition except sleep apnea. At the physical examination of his airway, the boy had the typical appearance of PRS. He had micrognathia, retrognathia, and his thyromental distance was 4.3 cm. He also had a mouth opening limitation and the maximum distance between incisors was 2.8 cm. His Mallampati class was grade 3, but he had no limited neck movement.
Because his parents disagreed with a conscious fiber-optic intubation for fear that their son would have a hard time during the procedure, we planned to induce anesthesia with propofol and succinylcholine and then intubate with the McGrath® MAC video laryngoscope and a malleable stylet. We prepared a Frova Intubating Introducer and fiber-optic bronchoscope for combined use. We also prepared a laryngeal mask airway (LMA) in case of difficult mask ventilation, according to the difficult airway guidelines [8]. Finally, if all of these methods failed, we planned to wake him because his parents wanted to cancel the surgery if the intubation failed.
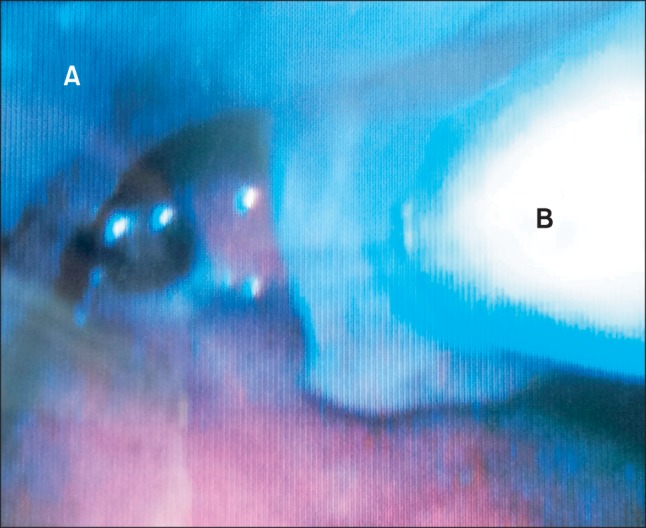
Anesthesia was induced in the operating room with 2 mg/kg propofol and 1 mg/kg succinylcholine after preoxygenation with 100% oxygen. Mask ventilation with manual assistance was performed easily. After full muscular relaxation, the McGrath® MAC video laryngoscope was inserted into the oropharynx and was placed posterior to the epiglottis because the epiglottis obscured the glottis and provided a half view of the glottis (Cormack-Lehane grade 2). However, insertion of the 60° angled malleable styletted ETT failed because the tube tip could be seen posterior to the arytenoids despite the external laryngeal maneuver. Then, a 90° angled malleable styletted ETT was used. The tube tip reached the glottis, but there was considerable resistance advancing the ETT through the vocal cords even though the stylet was withdrawn. Finally, the Frova Intubating Introducer with its tip modified as much as a 60° angle, similar to the McGrath® MAC video laryngoscope, was inserted through the vocal cords (Figs. 1 and 2). The Frova Intubating Introducer was used as a railroad for the ETT, and there was no difficulty advancing the ETT under vision with the video laryngoscope (Fig. 3). Correct placement of the ETT was further confirmed by auscultation and end-tidal CO2 detection. The surgical procedure, anesthetic maintenance, and recovery were uneventful.
We applied the McGrath® MAC video laryngoscope and Frova Intubating Introducer for endotracheal intubation in this case of a difficult airway and showed that the strategy was effective and successful.
Fiber-optic intubation is currently the gold standard for elective difficult airway management, but alternatives are described in the literature. The intubation techniques described include: Airtraq™ optical laryngoscopy (Prodol Meditec SA, Vizcaya, Spain), video laryngoscopy, non-fiber-optic intubation via LMA, fiber-optic intubation via LMA, and a paraglossal approach with tube advancement over a gum-elastic bougie [1]. We chose a McGrath® MAC video laryngoscope and malleable stylet because the McGrath® MAC video laryngoscope provides a good view of the glottis, and a malleable stylet helps direct the ETT to the glottis. As a precaution for a failed intubation, we also prepared a Frova Intubating Introducer and fiber-optic bronchoscope for combined use, and an LMA in case of a difficult mask ventilation according to the difficult airway guidelines [8]. It is important to have backup airway management plans because it takes less than 10 min for patients with a difficult airway to become hypoxic.
At our first attempt, insertion of the 60° angled malleable styletted ETT failed because the tube tip could be seen posterior to the arytenoids. This is a common problem with video laryngoscopes. In this case, external laryngeal pressure and withdrawal of the blade to lessen tilting of the laryngeal axis and to reduce the introducing angle may have been helpful [9]. However, these maneuvers did not work in our case. A 90° angled malleable styletted ETT was used on the second attempt. The tube tip reached the glottis, but there was considerable resistance advancing the ETT through the vocal cords. This occurs from time to time, as the tube tip may strike the anterior tracheal wall because of the angle of the stylet. In this case, the operator withdraws the stylet approximately 4 cm, withdraws the video laryngoscope by 1-2 cm and rotates the ETT slightly to facilitate passage into the trachea [5]. We withdrew the stylet and rotated the ETT to pass it into the trachea but failed. Finally, the Frova Intubating Introducer with its tip modified as much as a 60° angle like the McGrath® MAC video laryngoscope was attempted, and it was inserted through the vocal cords with no difficulty. This was a remarkable result because the tip of the 60° angled malleable styletted ETT, which had the same curvature as the Frova Intubating Introducer, could be seen posterior to the arytenoids even though the external laryngeal maneuver was applied. This can be explained as follows. Unlike the Macintosh laryngoscope, video laryngoscopes require a tilting force rather than a lifting force, and this force makes mouth opening too small to handle the ETT. Because the Frova Intubating Introducer has a smaller outer diameter than that of an ETT (4.6 mm for the Frova Intubating Introducer vs. 8.9 mm for a #6.5 ETT), it is easy to handle in a narrow space, as shown in this case. Thus, the Frova Intubating Introducer with its tip modified as much as 60° reached the glottis, whereas the same 60° angled malleable styletted ETT could not.
Although the Frova Intubating Introducer was designed for use with a Macintosh laryngoscope in the line of sight, and its tip should not be modified during Macintosh laryngoscopy, modifying its tip and combined use with a video laryngoscope provides some advantages. First, the Frova Intubating Introducer allows for easy handling in the narrow space under a video laryngoscope. Second, it creates less trauma than a styletted ETT. Less resistance advancing the 60° angled Frova Intubating Introducer through the vocal cords than that of a 90° angled malleable styletted ETT in our case supports this idea. Finally, preparing the Frova Intubating Introducer is less time consuming than a fiber-optic bronchoscope, so it can be used for an unanticipated difficult intubation.
The use of a video laryngoscope combined with a fiber-optic bronchoscope has been reported previously [10,11]. Fiber-optic bronchoscopy is a method of inserting an ETT with a video laryngoscope. However, this technique has some disadvantages; it needs more than two experienced anesthesiologists and one anesthesiologist should be familiar with the fiber-optic bronchoscope. In addition, the maintenance and preparation of a fiber-optic bronchoscope are time-consuming, limiting its use in the case of an unanticipated difficult intubation.
Use of a LMA is another good option in patients with PRS [12]; however, we thought it would be dangerous in this case because lung compliance might have decreased during repair of the pectus excavatum. We did not know that tracheal intubation with a Macintosh laryngoscope would be a success or failure in this patient because we did not use a Macintosh laryngoscope initially. Sometimes tracheal intubation is attempted with a Macintosh laryngoscope in anticipated difficult airway with little possibility of success, even though other methods for intubation, such as a video laryngoscope or fiber-optic bronchoscope, are available. This may be because of conceit or the challenging mind of the anesthetist. However, these unplanned attempts can put patients in danger. The difficult airway management guidelines developed by the Difficult Airway Society of the UK suggest that the initial tracheal intubation plan should not include more than four attempts [8]. The fact that multiple attempts can lead to tissue trauma causes more difficult intubation in subsequent trials, makes mask ventilation difficult, and results in hypoxia. Therefore, it is important to choose the first intubation plan carefully because fewer attempts lead to less airway trauma and increased patient safety.
In conclusion, we propose that the combined use of a McGrath® MAC video laryngoscope and a Frova Intubating Introducer is a useful option for a difficult airway with an upper airway anomaly.
References
1. Marston AP, Lander TA, Tibesar RJ, Sidman JD. Airway management for intubation in newborns with Pierre Robine sequence. Laryngoscope. 2012; 122:1401–1404. PMID: 22460229.
2. Nargozian C. The airway in patients with craniofacial abnormalities. Paediatr Anaesth. 2004; 14:53–59. PMID: 14717875.

3. Koerner IP, Brambrink AM. Fiberoptic techniques. Best Pract Res Clin Anaesthesiol. 2005; 19:611–621. PMID: 16408537.

4. Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005; 52:191–198. PMID: 15684262.

5. Rai MR, Dering A, Verghese C. The Glidescope system: a clinical assessment of performance. Anaesthesia. 2005; 60:60–64. PMID: 15601274.
6. Lim TJ, Lim Y, Liu EH. Evaluation of ease of intubation with the GlideScope or Macintosh laryngoscope by anaesthetists in simulated easy and difficult laryngoscopy. Anaesthesia. 2005; 60:180–183. PMID: 15644017.
7. Wilkes AR, Hodzovic I, Latto IP. Introducing new anaesthetic equipment into clinical practice. Anaesthesia. 2008; 63:571–575. PMID: 18477267.

8. Henderson JJ, Popat MT, Latto IP, Pearce AC. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004; 59:675–694. PMID: 15200543.
9. Kramer DC, Osborn IP. More maneuvers to facilitate tracheal intubation with the Glidescope. Can J Anaesth. 2006; 53:737. PMID: 16803924.

10. Choi GS, Park SI, Lee EH, Yoon SH. Awake Glidescope® intubation in a parient with a huge and fixed supraglottic mass -A case report-. Korean J Anesthesiol. 2010; 59(Suppl):S26–S29. PMID: 21286452.
11. Park CD, Lee HK, Yim JY, Kang IH. Anesthetic management for a parient with severe mento-sternal contracture: difficult airway and scarce venous access -A case report-. Korean J Anesthesiol. 2013; 64:61–64. PMID: 23372888.
Fig. 1
Comparison of the curvatures of the McGrath® MAC video laryngoscope blade, the modified Frova Intubating Introducer, and malleable styletted endotracheal tubes. (A) McGrath® MAC video laryngoscope, (B) Frova Intubating Introducer with its tip modified as much as a 60° angle, similar to the McGrath® MAC video laryngoscope, (C) 60° angled malleable styletted endotracheal tube, (D) 90° angled malleable styletted endotracheal tube.
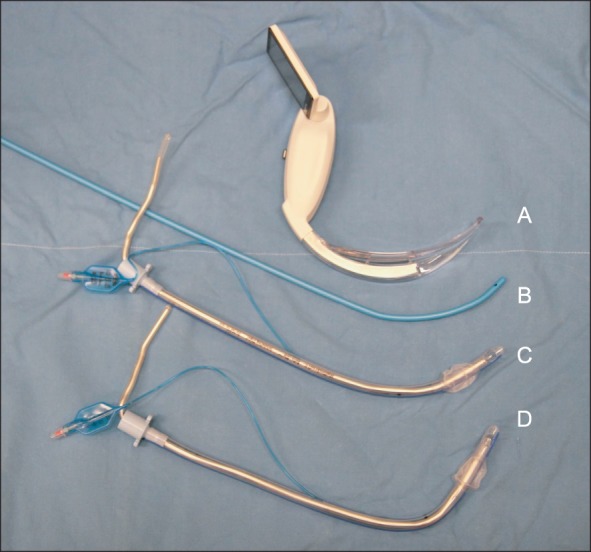
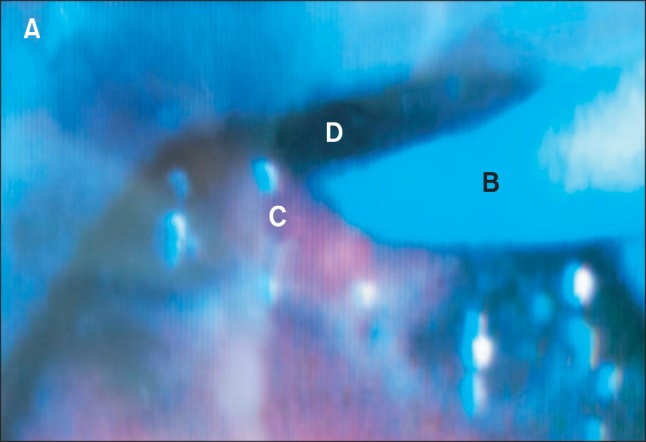
Fig. 2
Frova Intubating Introducer was inserted through the vocal cords under visualization of a McGrath® MAC video laryngoscope. The epiglottis was not seen because the video laryngoscope was placed posterior to the epiglottis. (A) Blade of the video laryngoscope, (B) Frova Intubating Introducer, (C) arytenoid cartilage, (D) glottic opening.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download