Abstract
Epidural fibrosis is a contributing factor to the persistent pain that is associated with failed back surgery syndrome (FBSS) and other pathophysiologies, particularly as it inhibits the passage of regional medications to areas responsible for pain. Therefore, effective mechanical detachment of epidural fibrosis can contribute to pain reduction and improve function in FBSS patients. In this report, we describe the successful treatment of FBSS patients with epidural adhesiolysis using a Fogarty catheter via the transforaminal approach.
The incidence of failed back surgery syndrome (FBSS) following lumbar spinal surgery is commonly reported to be between 10 and 40% [1]. FBSS has a major negative impact on a patient's quality of life and functional status, and is more disabling than other forms of common chronic pain [2]. Thus, effective management is of great importance in patients with established FBSS. Epidural fibrosis is a common occurrence following spinal surgery and is an important causative factor of FBSS [3]. It has been suggested that lysis of epidural adhesions can reduce epidural fibrotic tissue and improve the delivery of administered drugs to the target lesion, thereby reducing pain. To our knowledge, however, there is no definitive treatment modality that removes epidural fibrosis. By utilizing Fogarty balloon catheters to lyse the fibrotic tissue in the epidural space, we were able to successfully treat patients with refractory FBSS.
A 62-year-old female presented at our hospital complaining of pain in the left buttock and a tingling sensation in the left L5 dermatome. Eight months prior, the patient's left leg pain did improve after undergoing discectomy at the L5-S1 level, but her pain recurred and she still had the tingling sensation in her left leg. Her visual analogue scale (VAS) score for pain was 8 out of 10 and her functional score on the Oswestry Disability Index was 56%. Examination revealed normal motor power and sensation in the lower extremities, and normal pulsation of the dorsalis pedis and tibial arteries. The results of the straight leg raise test of the left leg were negative. She complained of leg pain after walking for 20 meters, and an epidurogram performed after discectomy indicated filling defects in her left side at the L5-S1 level. She was treated with 900 mg/day of gabapentin and a transdermal fentanyl patch (25 µg/hr). We performed percutaneous epidural adhesiolysis at the left L5 level using a Navigation catheter (Epimed International, Gloversville, USA), and, for the next 2 months, the patient demonstrated reduced leg pain (VAS 3 of 10) and increased walking distance (100 meters). Three months after treatment, her symptoms worsened to a degree similar to that before the procedure, so we decided to perform transforaminal balloon adhesiolysis.
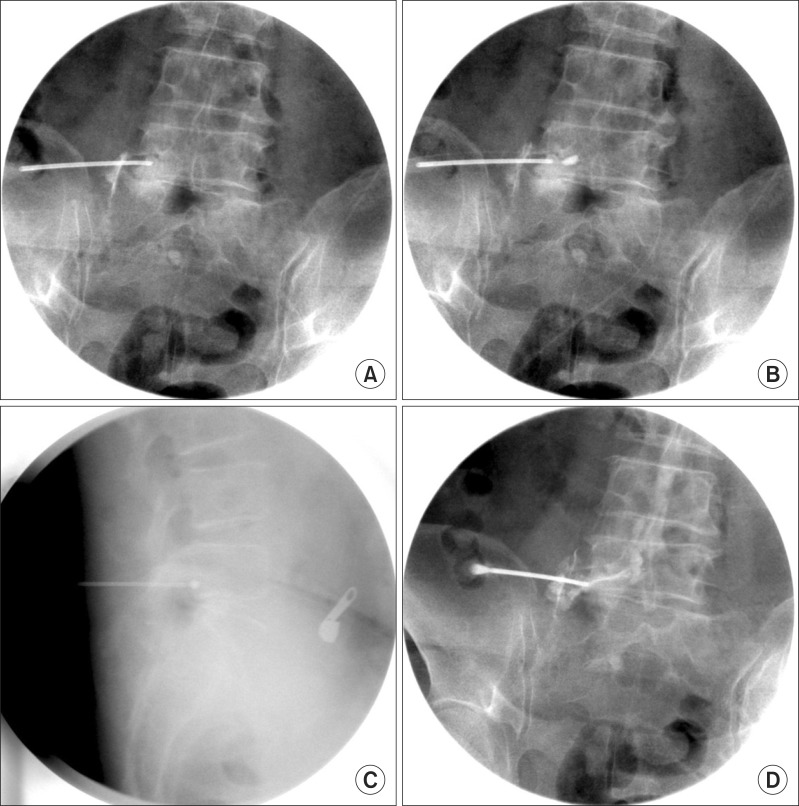
We obtained approval from our institutional review board and written informed consent from the patient. The patient was placed in the prone position, and a pillow was placed under her abdomen to minimize lumbar lordosis. After sterilizing the insertion site, an 18-gauge R-K needle (Epimed International, Gloversville, USA) was inserted into the left L5 intervertebral foramen. The filling defects in her left side at the L5-S1 level and the positioning of the tip in the anterior epidural space was confirmed by fluoroscopy with the aid of a contrast medium. A 3-Fr Fogarty catheter (Edward Lifescience, Irvine, CA, USA) filled with the contrast medium was introduced into the epidural space of the L5 intervertebral foramen and placed into the medial portion of the fibrotic area. Inflation of the balloon using 0.13 ml of the contrast medium followed by deflation was repeatedly performed throughout the affected region, from the lateral recess to the dural sleeve, with each inflation session lasting less than 5 seconds. If the patient complained of moderate discomfort during inflation of the balloon, the volume of the balloon was reduced. After removing the Fogarty balloon catheter, lysis of fibrosis was confirmed by fluoroscopy with the contrast medium, and 3 ml of a mixture of 0.8% lidocaine, 20 mg triamcinolone, and 1500 IU of hyaluronidase was administered (Fig. 1). There were no complications such as bleeding or severe pain throughout the procedure. The pain in her left leg (VAS 3 of 10) and functional status (40%) improved over the next 4 weeks and the patient reported no left leg pain (VAS 0 of 10), an improved functional status (32%), and increased claudication distance (200 meters) for the next 24 weeks.
A 76-year-old female patient who had undergone two lower back surgeries, a left partial laminectomy for disc herniation at the L4/5 and L5/S1 levels 4 years prior, and a discectomy at the L4/5 level 1 year and 5 months after the first operation was referred to our unit. Lower back pain and numbness in the left calf had developed about 6 months after the second operation and had gradually worsened. Her VAS score was 7 out of 10 and her Oswestry Disability Index was 48%. Examination revealed normal motor power and sensation in the lower extremities, and normal pulsation of the dorsalis pedis and tibial arteries. The straight leg raise test of her left leg was positive at 70 degrees. She complained of severe numbness and a pulling pain in her left leg after walking for more than 20 minutes. She had received various medications and treatments including transdermal fentanyl patch (12 µg/hr), Celecoxib 200 mg/day (Celebrex®, Pfizer, Inc., New York, NY, USA), repeated epidural steroid injections, and percutaneous epidural adhesiolysis using a Navigation catheter. Despite these interventions, she complained of persistent symptoms and only demonstrated a 20% improvement for 3 weeks after treatment; further, there were no improvements in her functional status or walking distance. We therefore decided to perform transforaminal balloon adhesiolysis. A filling defect in the medial side of her left L5 pedicle was confirmed by fluoroscopy using a contrast medium. A 3-Fr Fogarty catheter was introduced into the epidural space of her left L5 intervertebral foramen, followed by serial balloon decompression. After removal of the Fogarty balloon catheter, she was administered 3 ml of a mixture of 0.8% lidocaine, 20 mg triamcinolone, and 1500 IU hyaluronidase. There were no complications throughout the procedure. For the next 17 weeks, the patient reported reduced leg pain (VAS 2 of 10), an improved functional status (28%), and increased walking time (60 minutes). Eighteen weeks after treatment, her symptoms reoccurred but were more tolerable (VAS 4 of 10) than prior to treatment.
The hypothesized causes of FBSS include acquired stenosis, adjacent segment degeneration, internal disc disruption, recurrent disc herniation, retained disc fragments, spondylolisthesis, degenerative disc disease, radiculopathy, facet joint pain, sacroiliac joint pain, discitis, arachnoiditis, pseudoarthritis, segmental instability, and epidural fibrosis [4]. Some degree of epidural fibrosis is likely after any surgery that involves manipulation of the epidural space. Based on preclinical and clinical research, fibrosis may be a causative or contributing factor that results in persistent pain in 20 to 36% of FBSS patients [5]. Following spinal surgery, epidural scarring occurs, and, as a consequence, the nerve roots may become tethered, resulting in pain during movement of the spine [6]. Any subsequent perineural fibrosis may interfere with cerebrospinal fluid-mediated nutrition, resulting in hypersensitive nerve roots [7]. In addition, fibrosis may initiate vascular hypoxia by compromising the vascular supply of the nerve roots [8]. Fibrosis may inhibit the passage of regional medications to the areas of the spinal pathology that are responsible for pain [9], leading to the noted ineffectiveness of the repeated conventional epidural steroid injections that were provided to our patients for symptom relief.
We utilized 3-Fr Fogarty catheters to reduce epidural fibrosis and administer epidural drugs to the target area. The optimal rigidity of this catheter may have allowed it to reach the fibrotic area of the epidural space, whilst the pliable distal tip may have prevented damage to the nerve structures and the inflation of the balloon may have resulted in the effective mechanical detachment of the perineural fibrosis. We had already described our clinical experiences of using this technique to treat patients with spinal stenosis, and these patients reported markedly reduced pain, improved functional status, and increased claudication distance for 15 or 24 weeks [10]. Lysis of epidural fibrosis using a Fogarty catheter also appears to be effective in cases where epidural fibrosis is the main cause of FBSS. In our experience, this technique offers some distinct advantages. Using a contrast medium, instead of air, to inflate the balloon enables visualization of the degree of adhesion because the shape of the balloon becomes distorted at the site of adhesion. In addition, practitioners can adjust the power used to inflate the balloon by feeling the resistance that depends on the degree of adhesion and the pain severity reported by the patient, thereby minimizing trauma to neural structures. Furthermore, effective mechanical detachment of perineural fibrosis by balloon dilation contributes to the effective delivery of epidural medications to the target lesions.
Percutaneous epidural adhesiolysis using Racz or Navigation catheters is usually employed to treat patients with FBSS. To address the efficacy of percutaneous epidural adhesiolysis for the treatment of FBSS, a systematic review, which included three randomized controlled trials and four observational studies, was published. This review reported strong evidence following the use of this intervention that was indicative of short- and long-term pain relief, which was defined as an efficacy longer than 6 months. The review suggested that the effectiveness of adhesiolysis results from the placement of the catheter tip within the fibrotic area and the expansion of the perineural space, which once opened, allows the medication (e.g., steroids) to reach the appropriate lesion and provide neural blockades and anti-inflammatory effects [11]. Practically, however, epidural adhesiolysis using a Racz or Navigation catheter is often unsatisfactory. In cases of moderate to severe epidural adhesion, the catheter is not rigid enough to reach the target lesion. In addition, the catheter within the adhesion sites may continue to enter the same site, which can be time-consuming and result in patient discomfort. In the case of patient 2 described in this study, manipulation of the catheter was unsatisfactory and the patient demonstrated only a 20% improvement in pain for 3 weeks. The balloon adhesiolysis using a Fogarty catheter in patients 1 and 2 was a useful alternative to epidural adhesiolysis using a Navigation catheter.
Studies of patient safety should consider the effects of inflating the balloon on the spinal nerves. Intraneural edema develops after 2 hours of compression with either 50 mmHg or 200 mmHg of inflation pressure [12]. It has also been shown that the formation of edema in the spinal nerve root is more pronounced after rapid inflation, increased pressure, and increased duration of compression [13]. Therefore, the balloon pressure has to be slowly increased and the procedure has to be limited to less than 2 hours [14]. To ensure patient safety, we slowly inflated the balloon and limited each inflation session to 5 seconds. Also, based on our past successful experiences using this technique to treat spinal stenosis patients, we inflated the balloon with 0.13 ml of the contrast medium, which led to a balloon diameter of 6 to 8 mm. The volume for ballooning was adjusted according to the severity of pain.
We found that epidural adhesiolysis using a Fogarty catheter via the transforaminal approach to reach the target area is a useful procedure for treating FBSS in patients who have demonstrated limited improvement with repeated epidural steroid injections and percutaneous epidural adhesiolysis using a Navigation catheter. Effective mechanical detachment of perineural fibrosis via inflation of the balloon and drug delivery to the target site provided symptom improvement. Although additional studies are needed to determine the appropriate indications, complications, and usefulness of this method, our two current cases suggest that this method can potentially be used for the treatment of FBSS.
References
1. North RB, Ewend MG, Lawton MT, Kidd DH, Piantadosi S. Failed back surgery syndrome: 5-year follow-up after spinal cord stimulator implantation. Neurosurgery. 1991; 28:692–699. PMID: 1831547.
2. Thomson S, Jacques L. Demographic characteristics of patients with severe neuropathic pain secondary to failed back surgery syndrome. Pain Pract. 2009; 9:206–215. PMID: 19281499.

3. Chopra P, Smith HS, Deer TR, Bowman RC. Role of adhesiolysis in the management of chronic spinal pain: a systematic review of effectiveness and complications. Pain Physician. 2005; 8:87–100. PMID: 16850047.
4. Manchikanti L, Singh V. Failed back surgery: etiology and diagnostic evaluation. Spine J. 2004; 4:486–488. PMID: 15246312.
5. Trescot AM, Chopra P, Abdi S, Datta S, Schultz DM. Systematic review of effectiveness and complications of adhesiolysis in the management of chronic spinal pain: an update. Pain Physician. 2007; 10:129–146. PMID: 17256027.
6. Coskun E, Süzer T, Topuz O, Zencir M, Pakdemirli E, Tahta K. Relationships between epidural fibrosis, pain, disability, and psychological factors after lumbar disc surgery. Eur Spine J. 2000; 9:218–223. PMID: 10905440.

7. Rydevik BL. The effects of compression on the physiology of nerve roots. J Manipulative Physiol Ther. 1992; 15:62–66. PMID: 1740654.
8. Jayson MI. The role of vascular damage and fibrosis in the pathogenesis of nerve root damage. Clin Orthop Relat Res. 1992; 279:40–48. PMID: 1534723.

9. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 3--Post surgery syndrome. Pain Physician. 2008; 11:817–831. PMID: 19057628.
10. Kim SH, Koh WU, Park SJ, Choi WJ, Suh JH, Leem JG, et al. Clinical experiences of transforaminal balloon decompression for patients with spinal stenosis. Korean J Pain. 2012; 25:55–59. PMID: 22259719.

11. Epter RS, Helm S 2nd, Hayek SM, Benyamin RM, Smith HS, Abdi S. Systematic review of percutaneous adhesiolysis and management of chronic low back pain in post lumbar surgery syndrome. Pain Physician. 2009; 12:361–378. PMID: 19305485.
12. Olmarker K, Rydevik B, Holm S, Bagge U. Effects of experimental graded compression on blood flow in spinal nerve roots. A vital microscopic study on the porcine cauda equina. J Orthop Res. 1989; 7:817–823. PMID: 2795321.

13. Olmarker K, Rydevik B, Holm S. Edema formation in spinal nerve roots induced by experimental, graded compression. An experimental study on the pig cauda equina with special reference to differences in effects between rapid and slow onset of compression. Spine (Phila Pa 1976). 1989; 14:569–573. PMID: 2546258.
14. Basaran A, Topatan S. Spinal balloon nucleoplasty: a hypothetical minimally invasive treatment for herniated nucleus pulposus. Med Hypotheses. 2008; 70:1201–1206. PMID: 18096323.

Fig. 1
Serial images of balloon adhesiolysis using a 3-Fr Fogarty catheter filled with a contrast medium. (A) The needle was placed in the left L5 intervertebral foramen. (B, C) Balloon inflation was serially performed along the intervertebral neural foramen. (D) After balloon adhesiolysis, the spread of the contrast agent appears to be wider.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download