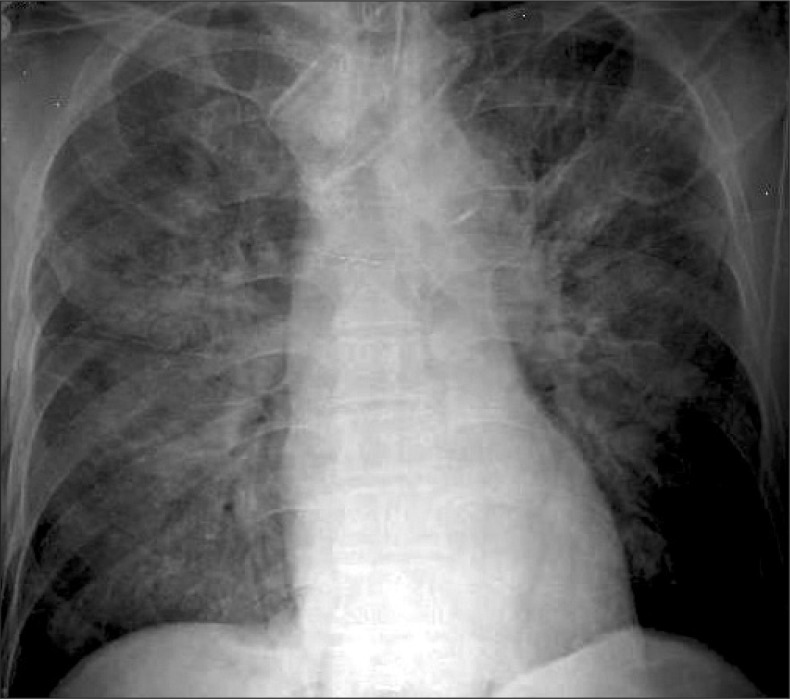
Negative pressure pulmonary edema (NPPE) related to upper airway obstruction is a well-described phenomenon [1], but NPPE related to bronchospasm has only rarely been reported [2]. We experienced NPPE during recovery from anesthesia in 77-year-old male with gastric cancer patient who underwent robot-assisted total gastrectomy. The patient was 157 cm tall and weighed 47.5 kg, and was a non-smoker with no allergy or medico-surgical history except for antihypertensive medication (bisoprolol for 1 yr). Preoperative laboratory findings, including pulmonary function test, were within normal ranges. Anesthesia was induced with propofol, remifentanil, and rocuronium and the anesthetic procedure proceeded without incident. Although peak airway pressure and PetCO2 increased during CO2 insufflation for pneumoperitoneum, they normalized after intravenous patient controlled analgesia (PCA) (fentanyl 1,000 µg/100 ml normal saline, 2 ml/hr) connection during surgery. Surgery was completed uneventfully in 190 min, and fentanyl (35 µg) was administered for analgesia. The endotracheal tube was removed when the patient responded to verbal commands, and neuromuscular function was then ascertained by train-of-four stimulation. However, after several minutes of assisted ventilation with a mask, the patient became drowsy, unresponsive to verbal commands or physical stimulation, and his spontaneous respiration weakened. Because pupil constriction was noted, PCA was discontinued and naloxone (0.4 mg) was slowly administered. Manual ventilation was maintained for 2-3 min while waiting the patient's awakening, when the patient coughed severely and subsequently developed signs of bronchospasm, such as, wheezing at forced exhalation and use of accessory muscles. Because ventilation was difficult via the oropharyngeal airway despite appropriate manipulations, tracheal intubation was performed with thiopental 50 mg and succinylcholine 50 mg. On auscultation, inspiratory and expiratory wheezing were apparent over the entire lung field. Arterial blood gas analysis (ABGA) immediately before intubation revealed pH 7.156, PCO2 75.8 mmHg, and PO2 84.4 mmHg. Controlled ventilation was maintained by isoflurane administration. Peak airway pressure was 48 mmHg at a tidal volume of 400 ml. Repeat ABGA revealed pH 7.283, PCO2 50.8 mmHg, and PO2 113.1 mmHg with a FiO2 of 1.0. Airway pressure was gradually decreased to 15 mmHg and signs of bronchospasm resolved 3 min after epinephrine 0.05 mg i.v. was administered. After 3-4 min of controlled ventilation, a pink and frothy secretion was noted inside the endotracheal tube, and breathing sounds were coarse over the entire lung field on auscultation. Furosemide 20 mg was administered and 8 cmH2O positive endexpiratory pressure was applied for possible pulmonary edema. Plain chest radiography revealed bilateral perihilar interstitial and alveolar infiltrates (Fig. 1). The patient was transferred to the intensive care unit for ventilatory care. After applying synchronized intermittent mandatory ventilation and continuous positive airway pressure mode for 12 hr under sedation, symptoms and signs improved. He was then extubated and nasal oxygen was supplied. ABGA showed values within normal range and the patient's general condition was improved. The patient was transferred to a general ward on POD 2.
In this patient, bronchospasm, which occurred during recovery from anesthesia, is believed to have been a cause of the pulmonary edema. Negative intrathoracic pressure is generated in the chest when a patient attempts to inspire against constricted airways during bronchospasm. Furthermore, this acute drop in intrathoracic pressure increases venous return to the right heart, and thus, increases pulmonary venous pressure. In addition, this increase in pressure in the venous circulation creates a transpulmonary hydrostatic pressure gradient and generates fluid movement.
Allergic bronchospasm is not a rare phenomenon in patients with a hypersensitive airway or asthma during anesthesia or recovery. However, our patient (a lifelong non-smoker) had no history of airway disease, and his preoperative pulmonary status was in the normal range. Non-allergic bronchospasm may also occur immediately after nonspecific stimuli [3]. In a survey of perioperative bronchospasm, non-allergic bronchospasm was found to be more frequent (79%) than allergic bronchospasm, and 20% of non-allergic bronchospasms were found to occur during the emergence/recovery period [4]. An acute increase in airway responsiveness may result from irritation of the well-innervated airway by a foreign body, such as, an endotracheal tube or suction catheter, or by secretions. In a large cohort study conducted by Schwilk et al. [5], the incidence of perioperative bronchospasm was 0.2% among 15,415 non-smoking patients without respiratory disease. In our patient, we believe that bronchospasm resulted from irritation by aspirated oral secretions during manual ventilation during re-narcotization. Non-allergic bronchospasm is usually not associated with cardiovascular symptom, but hypoxia following inadequate ventilation may lead to cardiovascular collapse, and may occasionally result in NPPE [3].
References
1. Lang SA, Duncan PG, Shephard DA, Ha HC. Pulmonary oedema associated with airway obstruction. Can J Anaesth. 1990; 37:210–218. PMID: 2178789.

2. Krodel DJ, Bittner EA, Abdulnour RE, Brown RH, Eikermann M. Negative pressure pulmonary edema following bronchospasm. Chest. 2011; 140:1351–1354. PMID: 22045880.

3. Dewachter P, Mouton-Faivre C, Emala CW, Beloucif S. Case scenario: bronchospasm during anesthetic induction. Anesthesiology. 2011; 114:1200–1210. PMID: 21460703.

4. Westhorpe RN, Ludbrook GL, Helps SC. Crisis management during anaesthesia: bronchospasm. Qual Saf Health Care. 2005; 14:e7. PMID: 15933304.

5. Schwilk B, Bothner U, Schraag S, Georgieff M. Perioperative respiratory events in smokers and nonsmokers undergoing general anaesthesia. Acta Anaesthesiol Scand. 1997; 41:348–355. PMID: 9113178.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download