The necessity of one lung ventilation (OLV) is increasing in various types of surgery, and double-lumen endotracheal tube (DLT), endobronchial blocker based Univent® (Univent, Fuji Systems Corp., Tokyo, Japan) tube, and endobronchial blocker through single-lumen endotracheal tube or laryngeal mask airway can be used for OLV [1]. There are some patients who need OLV after tracheostomy, and in those cases, the method that can be used for lung separation is limited. Here, we report a clinical experience in which OLV with an endobronchial blocker through a single lumen reinforced wire endotracheal tube was used in a patient who needed OLV after total laryngectomy.
A 64-year-old male patient was diagnosed with supraglottic cancer and had a permanent tracheostomy following a total laryngectomy in May, 2009 Treatment with chemotherapy and radiotherapy were carried out six times. Since a 7 mm sized solitary pulmonary nodule and 9.3 mm sized cavitary nodule were observed in the positron emission tomography (PET) done in April, 2010, the patient was scheduled to undergo a right upper lobectomy of the lung to treat and diagnose the metastatic cancer. He was 172 cm tall and 67.2 kg in weight.
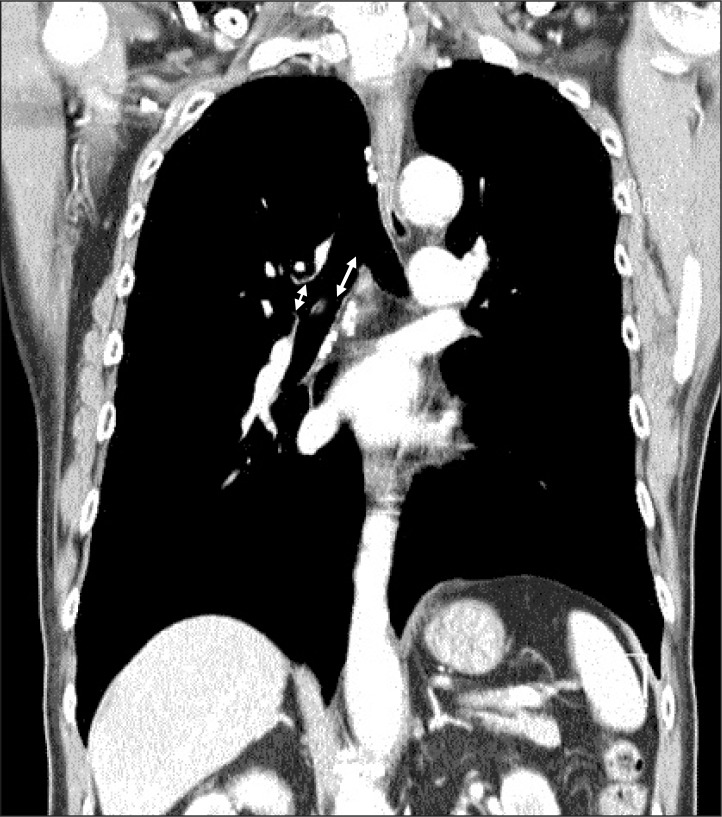
As total laryngectomy limited tracheal intubation orally, the patient had to be intubated through the stoma of the tracheostomy. We confirmed the patency and measured the size of the trachea and bronchus through the coronal and axial view of the chest CT (Fig. 1). The length and diameter of the right main bronchus was 23.38 mm and 17.40 mm, respectively. The diameter of the left main bronchus was 14.96 mm. Considering the operation site and the diameter of the left main bronchus, a 37 or 41 Fr DLT was preferred, but to avoid causing injury to the tissue around the stoma of tracheostomy and taking into consideration the angle formed by the trachea and the stoma, we decided to use a single-lumen reinforced wire endotracheal tube and endobronchial blocker (Coopdech®, Coopdech, Daiken medical Co., Osaka, Japan) which is more flexible than a DLT.
Before the induction of anesthesia, we supplied 100% oxygen through the stoma of the tracheostomy and while administering 0.02 µg/kg/min of intravenous remifentanil continuously, we examined the patient's airway with a pediatric flexible fiberoptic bronchoscope (FOB). We expected to have no difficulties in intubating through the stoma of the tracheostomy since it was impossible for the patient to wear a facial mask for positive ventilation. After 8 deep breaths with 100% oxygen and confirming the patient's loss of consciousness by injecting 1.5 mg/kg of propofol intravenously, endotracheal intubation was performed with a single-lumen reinforced wire endotracheal tube with a 7.5 mm internal diameter. The patient coughed mildly. After intravenous injection of 0.6 mg/kg of rocuronium bromide, we could not find any abnormalities in the ventilation by auscultating both lung sounds and confirmed there was sufficient muscle relaxation. With the end of the tube positioned 2 cm above the carina, the middle of the two black lines on the single-lumen reinforced wire endotracheal tube was placed at the stoma, and it was fixed tightly with Ioban™ (Ioban, 3M™ Health Care, St. Paul, USA). The endobronchial blocker was inserted into the right main bronchus, 1 cm directly under the carina with the guidance of a pediatric FOB. After reconfirming the position by auscultation, the endobronchial blocker was also fixed.
Anesthesia was maintained with 0.02-0.1 µg/kg/min of remifentanil, 0.5-2 vol% of sevoflurane, and oxygen and air at 3 L/min. During the operation, muscle relaxation was maintained by administration of intravenous rocuronium. Total anesthetic duration was 3 hours and 20 minutes, and the duration of OLV was 1 hour and 20 minutes. In the lateral position, the peak airway pressure (PAP) of two lung ventilation (tidal volume, 8 ml/kg; respiratory rate, 11 times/min; positive end expiratory pressure, 4 cmH2O) was 21 cmH2O. During OLV (peak inspiratory pressure, 17 cmH2O; respiratory rate, 11 times/min; positive end expiratory pressure, 4 cmH2O), we tried to keep the PAP at or under 21 cmH2O. Sixty percent oxygen was used and the results of the arterial blood gas analysis during OLV were as follows: pH 7.42, PaCO2 40 mmHg, PaO2 77 mmHg, and 95% oxygen saturation. All results from the arterial blood gas analysis during OLV were maintained as the standards measured under spontaneous respiration. All vital signs during the surgery were within normal range. When the patient's consciousness, muscle relaxation and spontaneous respiration were restored after the surgery, extubation was performed. The patient was transferred to the general ward after one day of observation in the intensive care unit.
Coe et al. [2] reported on 8 cases in which a DLT was inserted through the stoma of a tracheostomy, and Seo et al. [3] reported on the clinical experience of OLV anesthesia using a Univent® tube for a patient who had undergone a total laryngectomy. Campos [4] explained various methods of OLV in patients with tracheostomy. DLT is preferred to remove bleeding or respiratory secretion from the operated lung, but compared with a DLT or Univent® tube of the same internal diameter, the endobronchial blocker through the single-lumen endotracheal tube has a smaller external diameter and more flexibility and is more convenient to fix and eliminates the possible injury of the surrounding tissue of the stoma of the permanent tracheostomy.
Yang et al. [5] pointed out the possibility of incomplete collapse of the right upper lobe of the lung in a case using an endobronchial blocker. In our case, the length of the right bronchus was 23.38 mm;, the length of the endobronchial blocker cuff was 20 mm; therefore, the safety margin was as narrow as 3.38 mm, but there were no difficulties such as collapsing the right upper lobe of the lung.
In conclusion, we report a successful clinical experience of OLV in a patient who had undergone total laryngectomy by inserting the endobronchial blocker through the single-lumen reinforced wire endotracheal tube after understanding the patient's anatomical structure and airway condition (CT and FOB) preoperatively, along with a review of the relevant literature.
References
1. Campos JH. Current techniques for perioperative lung isolation in adults. Anesthesiology. 2002; 97:1295–1301. PMID: 12411817.
2. Coe VL, Brodsky JB, Mark JB. Double-lumen endobronchial tubes for patients with tracheostomies. Anesth Analg. 1984; 63:882. PMID: 6465590.

3. Seo DM, Lee JH, Lee SG, Ban JS, Min BW. One lung ventilation using a Univent® tube in a patient with permenant tracheostomy after total laryngectomy: a case report. Korean J Anesthesiol. 2006; 50:213–216.
4. Campos JH. Lung isolation techniques for patients with difficult airway. Curr Opin Anaesthesiol. 2010; 23:12–17. PMID: 19752725.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download